Category: Trauma
Keywords: c-spine, fracture, Burst (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/16/2024)
Click here to contact Robert Flint, MD
Identify this radiographic finding:
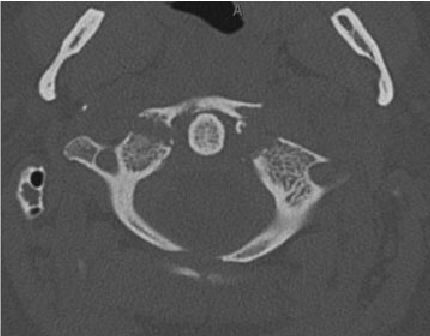
"Jefferson fracture is the eponymous name given to a burst fracture of the atlas. It was originally described as a four-part fracture with double fractures through the anterior and posterior arches, but three-part and two-part fractures have also been described.
50% are associated with other cervical spine injuries
33% are associated with a C2 fracture
25-50% of young children have a concurrent head injury
blunt cerebrovascular injury (BCVI): vertebral artery injury
extracranial cranial nerve injury" 1.
Category: Trauma
Keywords: fracture, spine, x-ray (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/9/2024)
Click here to contact Robert Flint, MD
Identify this injury and other associated injuries:
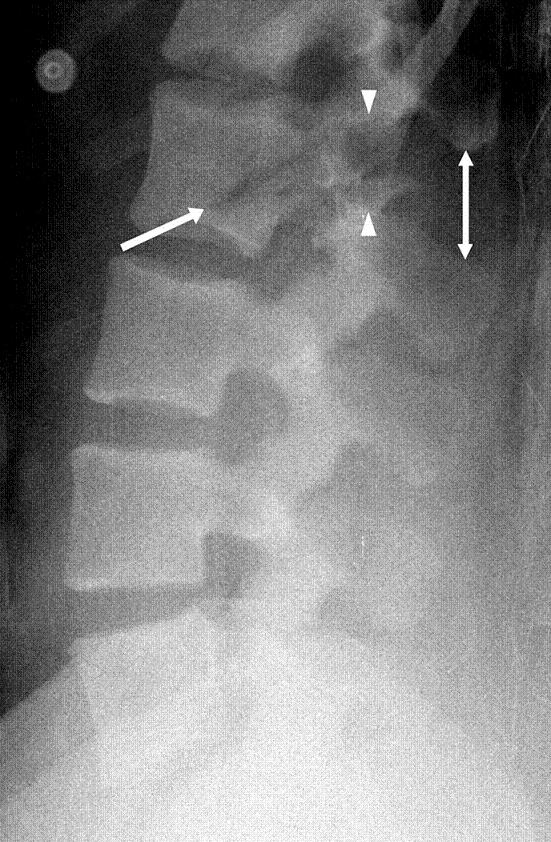
“Chance fractures also referred to as seatbelt fractures, are flexion-distraction type injuries of the spine that extend to involve all three spinal columns. These are unstable injuries and have a high association with intra-abdominal injuries. There is a high incidence of associated intra-abdominal injuries (especially the pancreas, duodenum, and abdominal aorta) that can result in increased morbidity and mortality. Associated intra-abdominal injuries appear to be more common in the pediatric age group with an incidence approaching 50%.” 2.
1.Chance Fracture - Medicalopedia
2. Jones J, Kogan J, Vadera S, et al. Chance fracture. Reference article, Radiopaedia.org (Accessed on 06 Sep 2024) https://doi.org/10.53347/rID-10186
Category: Trauma
Keywords: blunt bowel injury, BIPS, prediction, blunt trauma (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/8/2024)
Click here to contact Robert Flint, MD
Predicting which blunt abdominal trauma patients have mesenteric or bowel wall injuries early in their ED course will decrease morbidity and mortality. It is also a challenge even in the age of advanced CT imaging. This study from India looks at the Bowel Injury Prediction Score as a possible means to catch these injuries early in the course of care. The score uses white blood cell count over 17,000 (1 point), abdominal tenderness at the time of presentation(1 point), as well as a McNutt's scoring scale grade 4 (1 point) (table). The study found those with a score greater than 2 (out of 0-3) were much more likely to have bowel or mesenteric injury at time of laparotomy. Tenderness and CT findings were more likely to be predictive of bowel injury than WBC greater than 17,000. “BIPS had 94.5% sensitivity, 72% specificity, 88% PPV, and 86% NPV for identifying patients with sBBMI.”
My take away is an abnormal CT scan or significant tenderness of presentation warrant concern for mesenteric or bowel wall injury and surgical evaluation is appropriate for these patients. An elevated or normal white blood cell count isn't helpful in these patients. Surgeons may use this scale to help them decide if a patient warrants a trip to the operating room
| GRADE | FINDING |
|---|---|
| 1 | Isolated mesenteric contusion without associated bowel wall thickening or adjacent interloop fluid collection |
| 2 | Mesenteric hematoma?<?5 cm without associated bowel wall thickening or adjacent interloop fluid collection |
| 3 | Mesenteric hematoma?>?5 cm without associated bowel wall thickening or adjacent interloop fluid collection |
| 4 | Mesenteric contusion or hematoma (any size) with associated bowel wall thickening or adjacent interloop fluid collection |
| 5 | Active vascular or oral contrast extravasation bowel transaction or pneumoperitoneum |
Gupta SK, Singh PK, Sharma S, Gupta SK. Prospective validation of Bowel Injury Prediction Score for early diagnosis of surgically significant blunt bowel and mesenteric injury. Trauma. 2023;0(0). doi:10.1177/14604086231187523
Category: Trauma
Keywords: IPV, violence, injury, ulna, orthopedics (PubMed Search)
Posted: 9/1/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this systemic literature review of orthopedic injuries identified in intimate partner violence (IPV) the authors remind us that finger, hand, and especially isolated ulnar fractures are very commonly associated with IPV. When we see these injury patterns extra effort is required to determine if IPV is involved.
| Citation | **Bhandari et al.**3 | **Khurana et al.**18 | **Loder et al.**12 | **Porter et al.**13 | **Kavak et al.**7 | **Thomas et al.**17 |
|---|---|---|---|---|---|---|
| Division of injury locations | Fingers, wrist, shoulder dislocation, humerus fracture | Finger, hand, wrist, forearm, elbow, humerus, shoulder | Finger, hand, wrist, forearm, elbow, humerus, shoulder | Radius/ulna, humerus, upper extremity, right/left | Phalanx, radius, ulna (diaphysis/metaphysis, distal/proximal) | Phalanges (distal/medial/proximal), hand/finger, forearm, arm/shoulder right/left |
| Most common UEF location | Fingers (n = 11) | Finger (34.3%) | Finger (9.9%) | Radius and ulna (n = 80; 5.9%) | Ulna (14.5%) | Finger (46%) |
| Most common injury type‡ | Musculoskeletal sprains (all n = 21; 28% back n = 7; neck n = 6) | UEF (27.2%) | Contusions/abrasion (43.4%) | Rib fracture (17.5%) | Soft-tissue lesions (n = 1,007, 82.2%) | UEF (52%) |
* IPV = intimate partner violence, UEF = upper extremity fracture, and UEI = upper extremity injury.
† Summary table demonstrating the location prevalence of UEIs caused by cases of IPV. Fractures were quantified separately from other UEIs in this specific table.
‡ In all included articles the most common injury type was an injury to the head or neck; these are excluded because of the study aim.
Orthopaedic Injury Patterns in Intimate Partner Violence: Defensive Wounds and Fracture PatternsA Systematic Literature Review
Roan Willson, BS Erika Roddy, MDHolly Martinson, PhDCaitlin Farrell Skelton, MPHLisa Taitsman, MD, MPH
The Journal of Bone and Joint Surgery
August 2024; 12 (8): e24.00082
DOI 10.2106/JBJS.RVW.24.00082
Category: Trauma
Keywords: trauma, hyperopia, oxygen, length of stay (PubMed Search)
Posted: 8/29/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This retrospective study of Swiss trauma patients looked at blood gas oxygen levels within 3 hours of arrival to the trauma bay in severely injured patients over age 16. When comparing hypoxic, hyperoxic and normo-oxic patients there was no difference in 28 day mortality. Those with above normal oxygen levels tended toward longer hospital stays. The above normal oxygen cohort also were more likely to be intubated in the field.
This study fits with others showing around 20% of trauma patients arrive to our trauma bays over oxygenated. More research is needed to see the impact this has on care. Be mindful of over oxygenation especially in intubated trauma patients.
Iten, M., Pietsch, U., Knapp, J. et al. Hyperoxaemia in acute trauma is common and associated with a longer hospital stay: a multicentre retrospective cohort study. Scand J Trauma Resusc Emerg Med 32, 75 (2024). https://doi.org/10.1186/s13049-024-01247-5
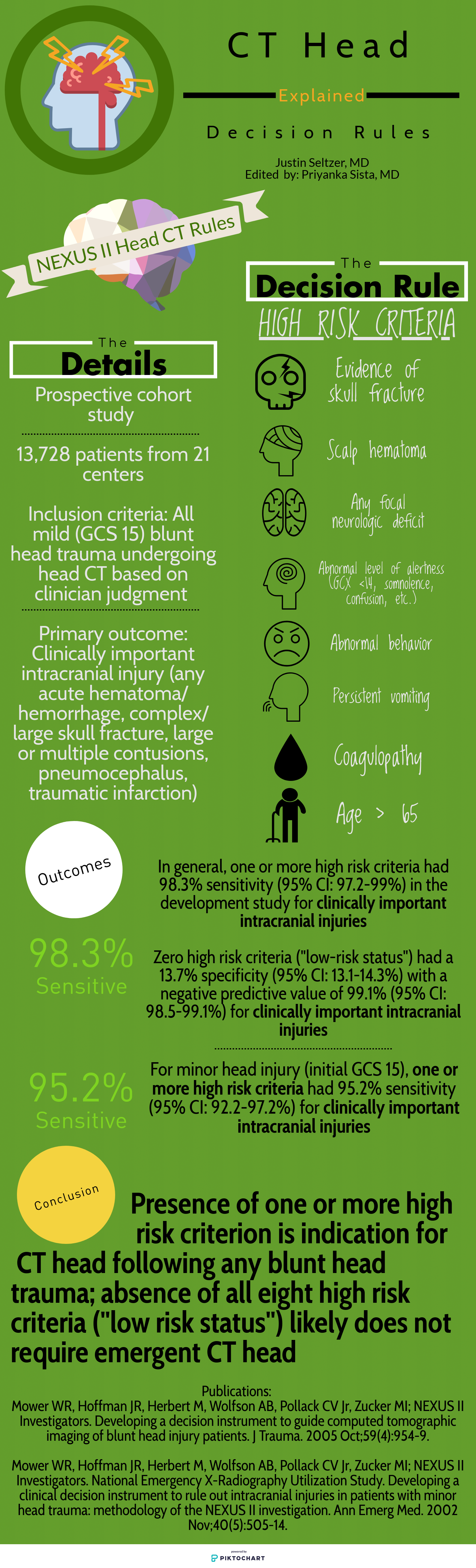
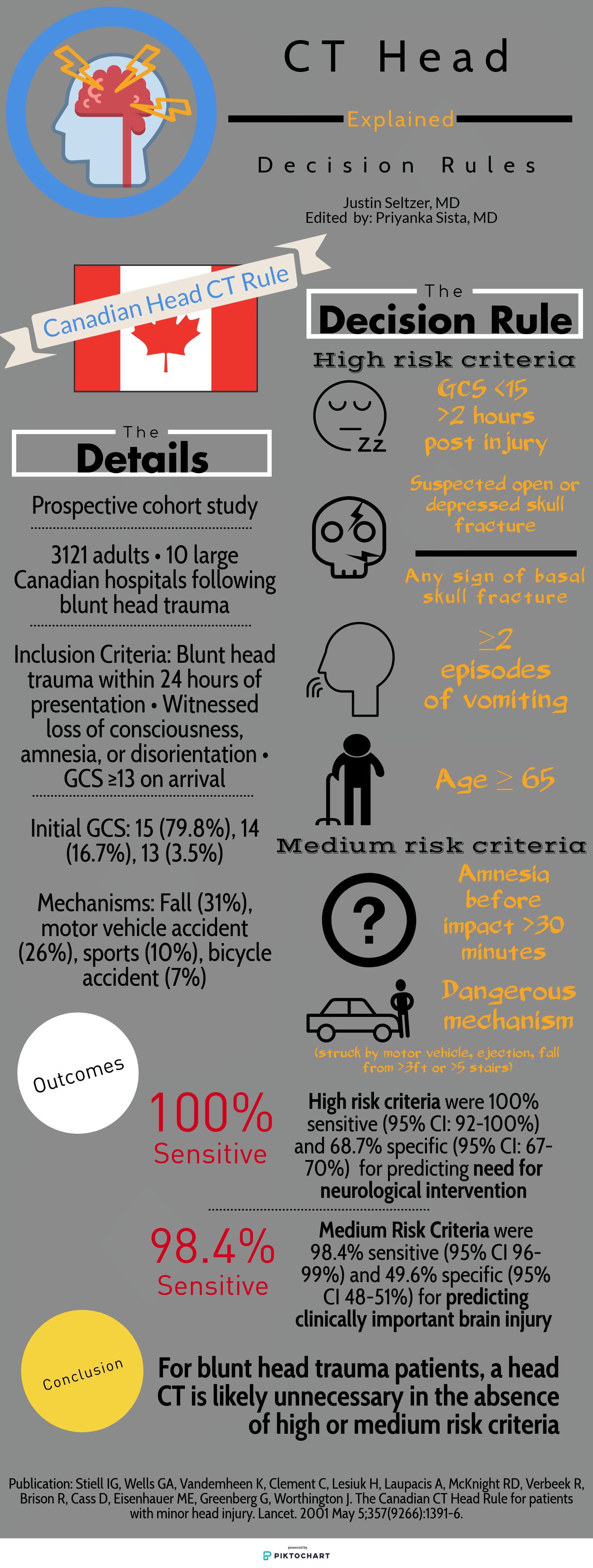
Category: Trauma
Keywords: Head injury, decision tools (PubMed Search)
Posted: 8/18/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Deciding who needs exposure to radiation after blunt head injury has been looked at by both the Canadian Head Injury Guidelines as well as NEXUS. This website has excellent graphics outlining the rules. Note age over 65 alone is predictive of significant intracranial injury. All recent studies indicate age over 65 even with a low suspicion mechanism such as fall from standing is still a significant risk for intracranial pathology.
Category: Trauma
Keywords: Fall, alcohol, geriatric, head injury (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/15/2024)
Click here to contact Robert Flint, MD
A study looking at patients over age 65 with head injuries from falls assessed the association of alcohol use with severity of injury. The alcohol use was self-reported which does limit the findings. The study found “Of 3128 study participants, 18.2% (n = 567) reported alcohol use: 10.3% with occasional use, 1.9% with weekly use, and 6.0% with daily use.” Those daily drinkers had a higher incidence of intercranial injuries.
The authors concluded: “Alcohol use in older adult emergency department patients with head trauma is relatively common. Self-reported alcohol use appears to be associated with a higher risk of ICH in a dose-dependent fashion. Fall prevention strategies may need to consider alcohol mitigation as a modifiable risk factor.”
Zirulnik A, Liu S, Wells M, et al. Alcohol use is associated with intracranial hemorrhage in older emergency department head trauma patients. JACEP Open. 2024; 5:e13245. https://doi.org/10.1002/emp2.13245
Category: Trauma
Keywords: Cspine, nexus, Canadian, rule (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/12/2024)
Click here to contact Robert Flint, MD
A reminder of two validated tools used to determine the need for cervical spine imaging in adult blunt trauma patients. A recent meta analysis concluded:
“Based on studies, both CCR and NEXUS were sensitive rules that have the potential to reduce unnecessary imaging in cervical spine trauma patients. However, the low specificity and false-positive results of both of these tools indicate that many people will continue to undergo unnecessary imaging after screening of cervical SCI using these tools. In this meta-analysis, CCR appeared to have better screening accuracy.”
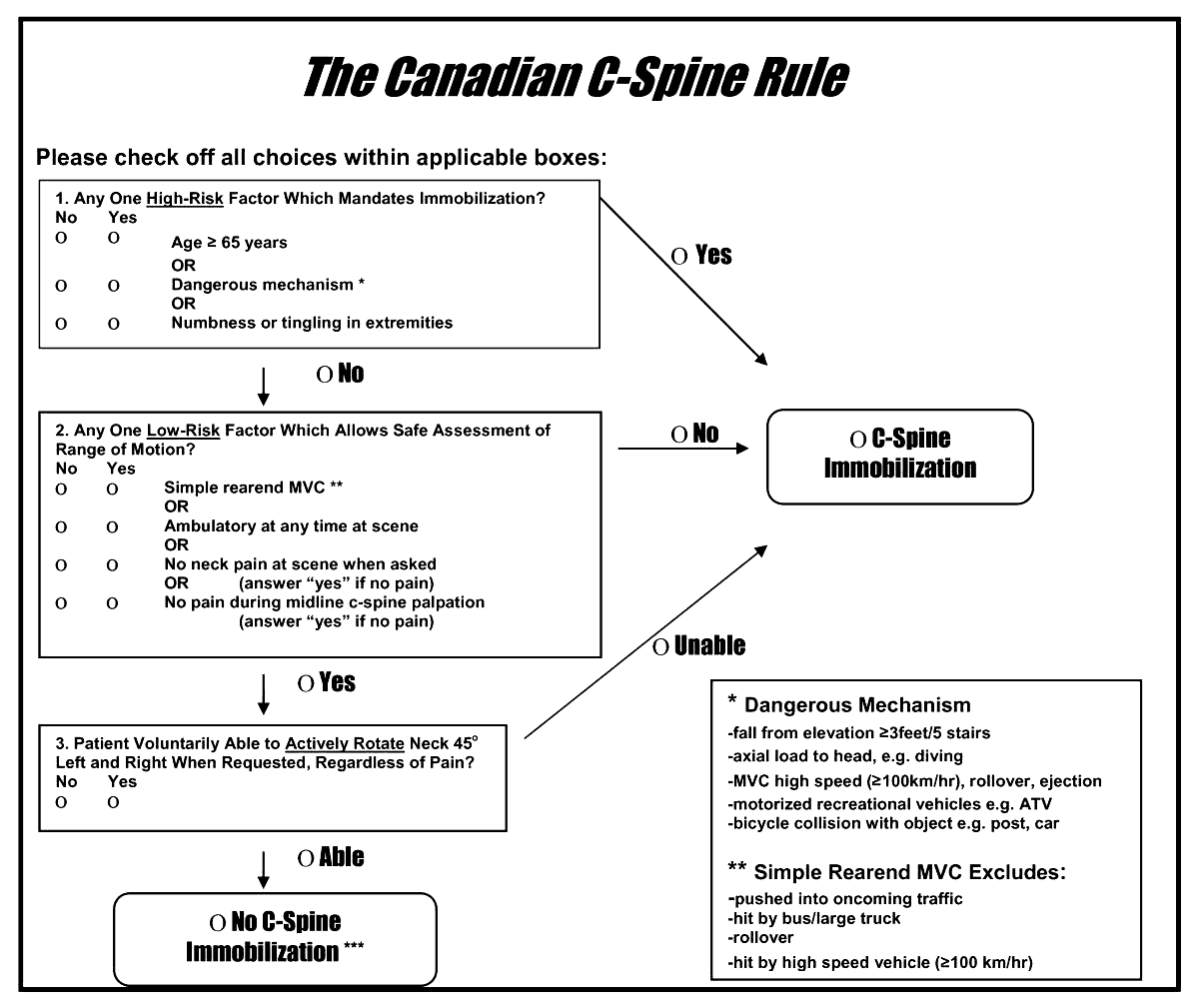
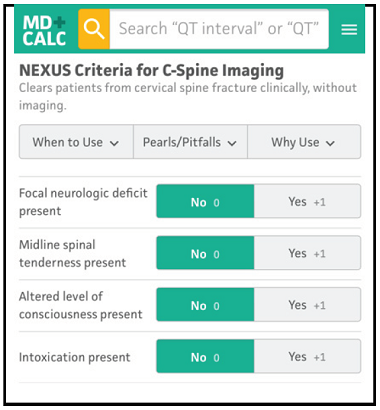
Arch Acad Emerg Med. 2023; 11(1): e5.
Published online 2023 Jan 1. doi: 10.22037/aaem.v11i1.1833
PMCID: PMC9807951
PMID: 36620739
Canadian C-spine Rule versus NEXUS in Screening of Clinically Important Traumatic Cervical Spine Injuries; a systematic review and meta-analysis
Category: Trauma
Keywords: Cspine, pecarn, rule, injury (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/11/2024)
Click here to contact Robert Flint, MD
A just released study published in the Lancet gives us guidance on which pediatric blunt trauma patients need cervical spine imaging. Age range was 0-17 years.
“Out of 22,430 children included in the study, 433 (1.9%) were found to have Cervical spine injury (CSI). The study identified 4 high risk factors for CSI to be used to triage children to CT (12% risk for a cervical spine injury):
In children without high-risk findings, 5 additional findings identified children with intermediate, non-negligible risk of CSI (3.6% risk of a cervical spine injury):
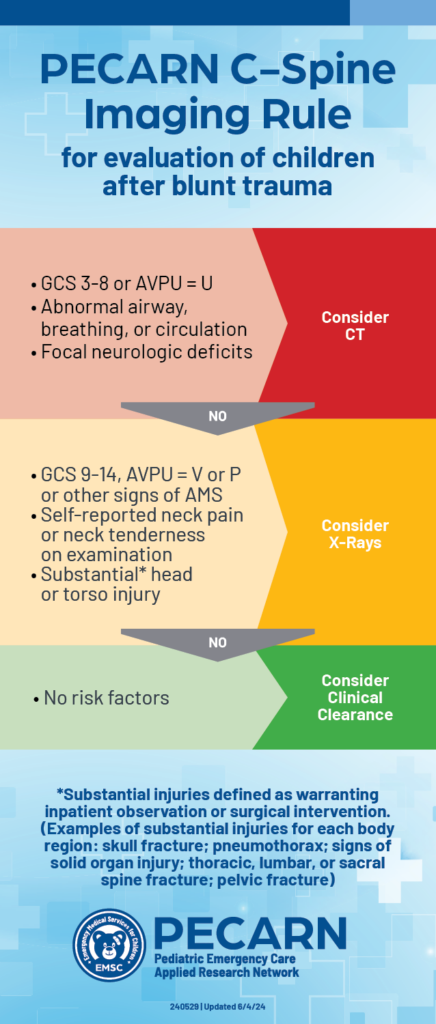
PECARN prediction rule for cervical spine imaging of children presenting to the emergency department with blunt trauma: a multicentre prospective observational study
Prof Julie C Leonard, MD Monica Harding, MS Prof Lawrence J Cook, PhD Prof Jeffrey R Leonard, MD
Prof Kathleen M Adelgais, MD Fahd A Ahmad, MD et al.
Published:June 03, 2024DOI:https://doi.org/10.1016/S2352-4642(24)00104-4
2. https://pecarn.org/pecarn_news/clinical-decision-rule-cervical-spine/
Category: Trauma
Keywords: Pneumothorax, chest X-ray, 38 mm, observation (PubMed Search)
Posted: 7/29/2024 by Robert Flint, MD
(Updated: 7/31/2024)
Click here to contact Robert Flint, MD
A cut-off of 35mm on CT scan has been shown to be predictive of which traumatic pneumothoracies require thoracostomy tube placement vs. safety of observation. This retrospective study looked at chest X-ray findings to see if there was a similar size cut-off where patients could be safely observed rather than undergo this invasive procedure. They found 38mm was the size over which observation failed. Of note, lactic acidosis and need for supplemental oxygen also predicted the need for chest tube placement
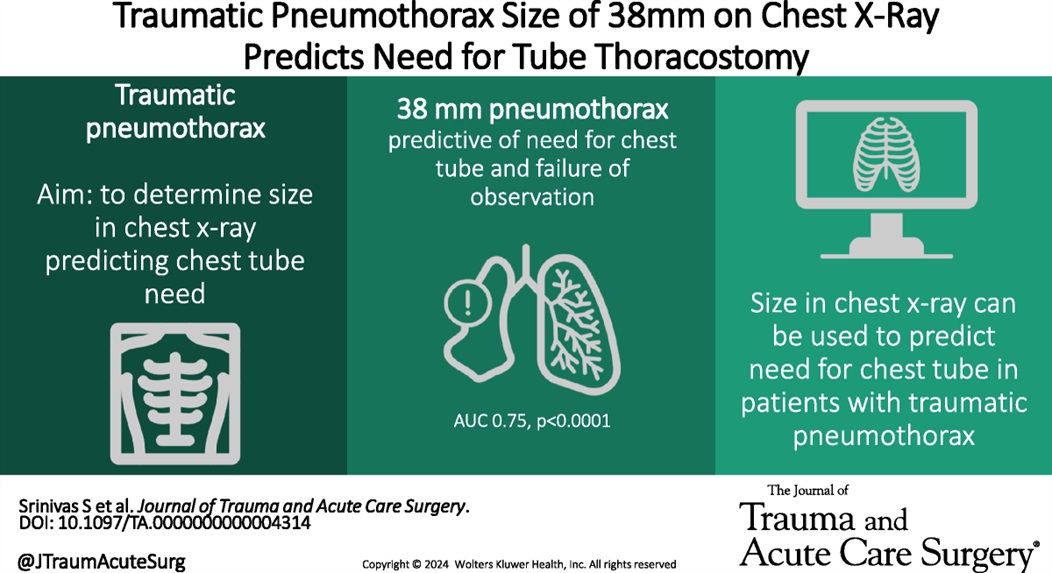
Using chest X-ray to predict tube thoracostomy in traumatic pneumothorax: A single-institution retrospective review
Srinivas, Shruthi MD; Henderson, Katelyn BS; Bergus, Katherine C. MD; Jacobs, Ayanna MD; Baselice, Holly MPH; Donnelly, Edwin MD, PhD; Valdez, Carrie MD; Tracy, Brett M. MD; Coleman, Julia R. MD, MPH
Journal of Trauma and Acute Care Surgery 97(1):p 82-89, July 2024. | DOI: 10.1097/TA.0000000000004314
Category: Trauma
Keywords: TBI, hypotension, vasopressors (PubMed Search)
Posted: 7/29/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
In this prospective, observational study of trauma patients with isolated head trauma, 62% of patients developed post-intubation hypotension. Comparing patients receiving hypertonic saline, vasopressors, crystalloid, or blood those receiving hypertonic saline and vasopressors had less post-intubation hypotension.
TBI patients who develop hypotension have worse outcomes. This study reminds us the use of vasopressors in trauma patients to maintain blood pressure is appropriate in the correct circumstances.
Anand, Tanya MD, MPH, MT(ASCP); Hejazi, Omar MD; Conant, Madolyn BS; Joule, Dylan BS; Lundy, Megan MD; Colosimo, Christina DO, MS; Spencer, Audrey MD; Nelson, Adam MD; Magnotti, Lou MD; Joseph, Bellal MD
Journal of Trauma and Acute Care Surgery 97(1):p 112-118, July 2024. | DOI: 10.1097/TA.0000000000004306
Category: Trauma
Keywords: Txa, TBI, seizure, risk (PubMed Search)
Posted: 7/21/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
According to this study, no TXA 2g bolus was not found to increase the number of seizures in TBI pts.
TXA has been shown to improve mortality in inter cranial hemorrhage trauma patients if given within 2 hours. TXA is also known to lower seizure threshold. This study was a secondary analysis of a larger study comparing placebo to 1 g TXA bolus plus 8 hour infusion or 2g bolus TXA in the prehospital setting. There was no difference in the number of pts experiencing seizure or outcome in those receiving the 2g bolus of TXA.
The Association Between Tranexamic Acid and Seizures in Moderate or Severe Traumatic Brain Injury
David V. Deshpande BS a, W. Ian McKinley MD, MS b, Andrew J. Benjamin MD, MS c, Martin A. Schreiber MD, FACS, FCCM d, Susan E. Rowell MD, MBA, MCR
Volume 301, September 2024, Pages 359-364 https://doi.org/10.1016/j.jss.2024.06.035
Category: Trauma
Keywords: facial trauma, orbit, fracture (PubMed Search)
Posted: 7/7/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Patient struck in left eye. The patient was asked to look up during exam and this is the finding. What imaging modality would you order if so inclined, what is the injury, and what is the disposition/plan?

Concern for a left orbital “blowout” fracture with muscle entrapment. Also called the trapdoor fracture. CT is the imaging modality of choice not plain films. This injury requires emergent consultation with a face surgeon (plastics, ENT or oculoplastics.). Right orbital fracture in the photo below.
-668ade5e780f0.jpg)
1.https://www.researchgate.net/figure/Girl-with-blowout-fracture-of-the-left-orbit-and-enophthalmos_fig1_351847537
2.|The Lancet. VOLUME 395, ISSUE 10221, P370, FEBRUARY 01, 2020
Paul Geraeds Kemps, BSc Michaël Herman Frank, MD
Published: February 01, 2020DOI:https://doi.org/10.1016/S0140-6736(19)33223-4
Category: Trauma
Keywords: Ketamine intranadal fentanyl trauma pain (PubMed Search)
Posted: 6/30/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
192 trauma patients who were receiving pre-hospital fentanyl for moderate to severe pain were randomized to placebo or intranasal 50 mg ketamine as an adjunct for pain control. There was no difference between the two groups in decrease in pain scale.
The authors concluded: “In our sample, we did not detect an analgesic benefit of adding 50 mg intranasal ketamine to fentanyl in out-of-hospital trauma patients.”
Jason T. McMullan, MD, MS Christopher A. Droege, PharmD Kathleen M. Chard, PhD Kim Ward Hart, MA
Christopher J. Lindsell, PhD Richard J. Strilka, MD, PhD
Open AccessPublished:June 12, 2024DOI:https://doi.org/10.1016/j.annemergmed.2024.04.018
Category: Trauma
Keywords: troponin fall geriatric trauma (PubMed Search)
Posted: 6/20/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
A prospective European study of patients over age 65 presenting with a ground level fall obtained troponin levels to ascertain if myocardial infarction was a cause of the ground level fall. Troponin levels were elevated in a majority of patients however only 0.5% were defined as having a myocardial infarction. Of the 3% who died within 1 year, troponin was found to be higher than those that survived the one-year study period. The authors concluded “Our data do not support the opinion that falls may be a common presenting feature of MI. We discourage routine troponin testing in this population. However, hs-cTnT and hs-cTnI were both found to have prognostic properties for mortality prediction up to 1?year.”
Diagnostic and prognostic value of cardiac troponins in emergency department patients presenting after a fall: A prospective, multicenter study
Tanguy Espejo, Lukas Terhalle, Alexandra Malinovska MD, Henk B. Riedel MD, Laura Arntz MD, Livia Hafner, Karen Delport-Lehnen MD, Joanna Zuppinger MD,
First published: 26 March 2024
Academic Emergency Medicine
Category: Trauma
Keywords: hemorrhage, tourniquet, innovation, Delphi (PubMed Search)
Posted: 6/9/2024 by Robert Flint, MD
(Updated: 6/16/2024)
Click here to contact Robert Flint, MD
Appropriately, a great deal of time and energy is being expended to educate on the use of tourniquets to prevent mass hemorrhage. Are the current generation of tourniquets the best that we can have? These authors performed a Delphi study to assess needs with tourniquet design.
They concluded the next generation of tourniquets should have the following: “Capable of being used longer than 2 hours, applied and monitored by anyone, data displays, semiautomated capabilities with inherent overrides, automated monitoring with notifications and alerts, and provide recommended actions.”
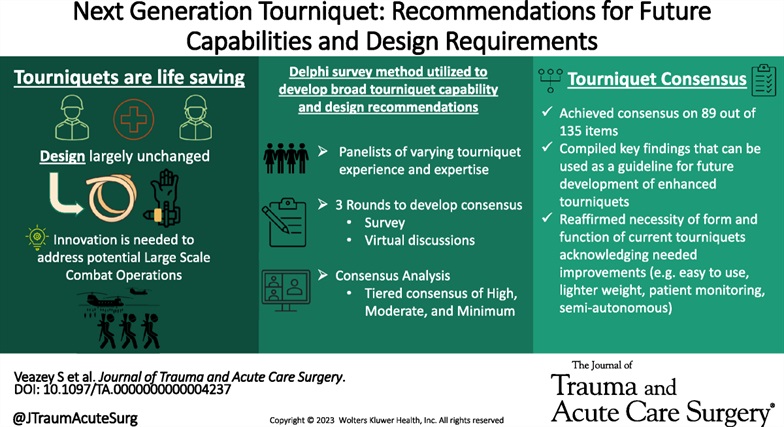
Veazey, Sena R. MS; Mike, Jared F. PhD; Hull, Darke R. BS; Ryan, Kathy L. PhD; Salinas, Jose PhD; Kragh, John F. Jr MD. Next-generation tourniquet: Recommendations for future capabilities and design requirements. Journal of Trauma and Acute Care Surgery 96(6):p 949-954, June 2024. | DOI: 10.1097/TA.0000000000004237
Category: Trauma
Keywords: BIG, transfer, head trauma, brain injury (PubMed Search)
Posted: 6/9/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study used the modified Brain injury Guidelines retrospectively to assess whether the guidelines would have saved transfers to their level one facility safely. They concluded the guidelines would have effectively prevented unnecessary mBIG 1 and mBIG2 transfers with no patient harm.
TABLE 1 - Modified Brain Injury Guidelines Radiologic Stratification, as per Kahn et al.
| mBIG 1 | mBIG 2 | mBIG 3 | |
|---|---|---|---|
| Skull fracture | No | Non-displaced | Displaced |
| SDH | ?4 mm | 4–7.9 mm | ?8 mm |
| EDH | No | No | Yes |
| SAH | ?3 sulci and <1 mm | Single hemisphere or 1–3 mm | Bihemisphere or >3 mm |
| IVH | No | No | Yes |
| IPH | ?4 mm | 4–7.9 mm | ?8 mm or multiple |
EDH, epidural hematoma; IPH, intraparenchymal hemorrhage; IVH, intraventricular hemorrhage; SAH, subarachnoid hemorrhage.
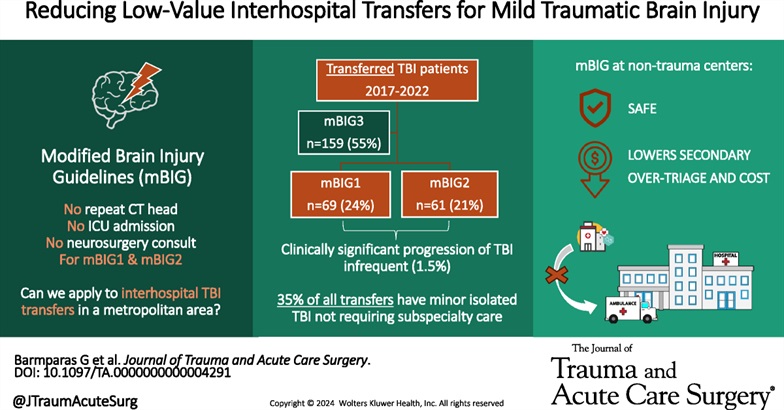
Shen, Aricia MD; Mizraki, Nathaniel MD; Maya, Marcel MD; Torbati, Sam MD; Lahiri, Shouri MD; Chu, Ray MD; Margulies, Daniel R. MD; Barmparas, Galinos MD. Reducing low-value interhospital transfers for mild traumatic brain injury. Journal of Trauma and Acute Care Surgery 96(6):p 944-948, June 2024. | DOI: 10.1097/TA.0000000000004291
Category: Trauma
Posted: 5/29/2024 by Robert Flint, MD
(Updated: 6/1/2024)
Click here to contact Robert Flint, MD
In this Scandinavian study looking at 2,362 head injury patients on oral anticoagulants, the authors found only 5 cases of delayed hemorrhage and none of the five underwent neurosurgery. The authors concluded:
“In patients with head trauma, on oral anticoagulation, the incidence of clinically relevant delayed intracranial hemorrhage was found to be less than one in a thousand, with detection occurring four days or later after initial presentation.”
It would appear based on this study and others that it is safe to discharge these patients with a normal head CT and giving strict return precautions for headache, nausea, vomiting or other changes.
André, L., Björkelund, A., Ekelund, U. et al. The prevalence of clinically relevant delayed intracranial hemorrhage in head trauma patients treated with oral anticoagulants is very low: a retrospective cohort register study. Scand J Trauma Resusc Emerg Med 32, 42 (2024). https://doi.org/10.1186/s13049-024-01214-0
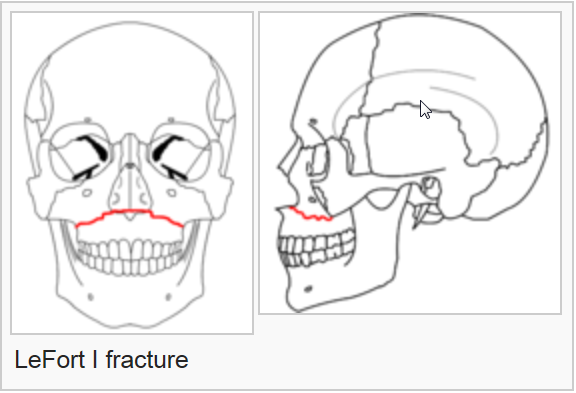
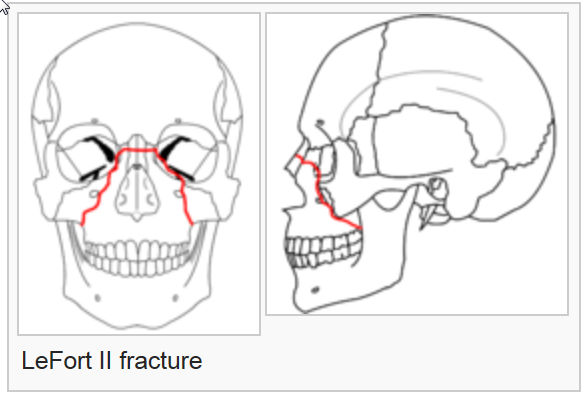
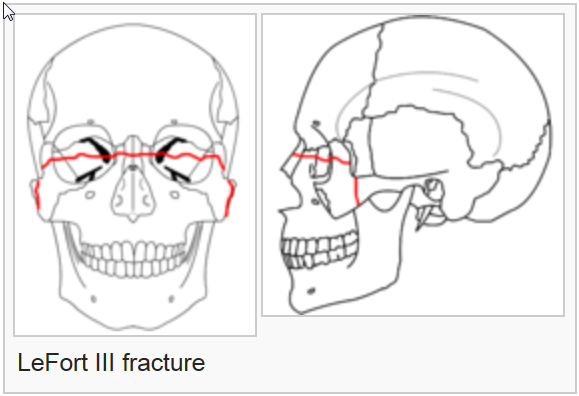
Category: Trauma
Keywords: Lefort, facial, trauma, fracture (PubMed Search)
Posted: 5/26/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
On exam, assess for facial instability and airway patency. CT scan is the imaging of choice. The higher the number, the more complex the fracture, the more unstable and the more difficult the airway managment will be. Look for open lacerations or blood in the sinuses and treat with antibiotics if these are found. Consult ENT or plastics urgently for further management.
The reference is a nice review of these fractures
Category: Trauma
Keywords: vasopressor, hemorrhage, shock, trauma (PubMed Search)
Posted: 5/19/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this podcast, the concept of vasopressor use in hemorrhagic shock is discussed. Key take away points:
