Category: Orthopedics
Keywords: Methylene Blue, Intra-articular, Joint (PubMed Search)
Posted: 11/21/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Evaluation of Potential Intra-Articular Joint Lacerations
Skin and soft tissue injuries in proximity to a joint often prompt concern of whether the injury violated the joint space. Joint Space involvement is important to exclude as it can lead to septic joints and long term disability.
One easy way to determine if the joint capsule has been violated is to inject methylene blue into the joint and watch to see if any of the methylene blue extravasates through the soft tissue.
Indications for a methylene blue injection include:
There are no absolute contraindications. Though clearly the procedure does not need to be done when the injury highly suggests an open joint injury and the patient will require operative debridement and exploration.
To watch a video of a injection head to eMedicine by clicking http://emedicine.medscape.com/article/114453-overview
Shlamovitz, Gil. Injection, Intra-Articular Methylene Blue. eMedince, Accessed November 2010. http://emedicine.medscape.com/article/114453-overview
Category: Orthopedics
Keywords: Spinal Epidural Abscess (PubMed Search)
Posted: 10/30/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Risk Factors for Spinal Epidural Abscesses
Building on Dr. Corwell's pearl from last week concerning Spinal Epidural Abscess, risk factors for Spinal Epidural Abscesses other than IV drug abuse are:
The infection can occur via three routes 1) hematogenous spread 2) Direct Extension from a local infection such as osteoomyelitis, and 3) iatrogenic introduction which is thought to be responsible for 14-22% of the cases. A catheter in the epidural space for more than 2 days has a infection rate of 4.3%.
Marc Tompkins, Ian Panuncialman, Phillip Lucas, Mark Palumbo. Spinal Epidural Abscess The Journal of Emergency Medicine, Volume 39, Issue 3, September 2010, Pages 384-390
Category: Orthopedics
Keywords: Subungual Hematomas (PubMed Search)
Posted: 10/16/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Subungual Hematomas:
Category: Orthopedics
Keywords: Patellofemoral syndrome (PubMed Search)
Posted: 10/2/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
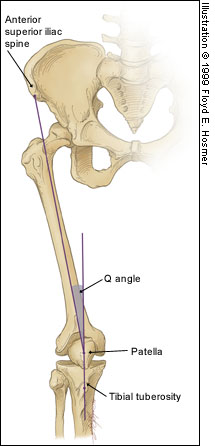
Patellofemoral Syndrome (Chondromalacia Patella)
Juhn MS et al. Patellofemoral pain syndrome: a review and guidelines for treatment. Am Fam Physician. (1999)
Category: Orthopedics
Keywords: Pain, Geriatrics (PubMed Search)
Posted: 9/18/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Pain Control in the Elderly
So the take home lesson for this pearl is that the elderly have a lower risk of delirium if their pain is treated appropriately.
Duggleby W, Lander J: Cognitive status and postoperative pain: older adults. J Pain Symptom Manage 1994; 9: 19-27.
Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L, Marcantonio ER: The impact of postoperative pain on the development of postoperative delirium. Anesth Analg 1998; 86: 781-785.
Category: Orthopedics
Keywords: Adhesive Capsulitis (PubMed Search)
Posted: 8/28/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Adhesive Capsulitis -- Frozen Shoulder
Category: Orthopedics
Keywords: Rotator Cuff Tears, Chronic, Acute (PubMed Search)
Posted: 8/21/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Rotator Cuff Tears:
Four muscles make up the rotator cuff (SITS) which control internal and external rotation of the shoulder and abduct the shoulder.
Tears can be due to acute injuries (falls, heavy lifting, forceful abduction), though the majority (>90%) of rotator cuff tears are chronic in nature and due to subacromial impingement and decreased blood supply to the tendons.
Most patients can be treated with sling immobilization, NSAIDs and referral to sports medicine or orthopaedic surgeons. Elderly patients should be referred quickly as prolonged immobilization can lead to a frozen shoulder.
Category: Orthopedics
Posted: 8/7/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Some common injuries and their board review associated complications
Category: Endocrine
Keywords: DKA, Management (PubMed Search)
Posted: 7/31/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Diabetic Ketoacidosis Treatment:
Charfen MA, Fernadez-Frackelton M. Diabetic Ketoacidosis. EMCNA 2005:609-628.
Category: Toxicology
Keywords: anticholinergic, sympathomimetic, pupil (PubMed Search)
Posted: 7/22/2010 by Michael Bond, MD
(Updated: 7/24/2010)
Click here to contact Michael Bond, MD
A patient arrives via EMS agitated with VS: P 140, BP 155/100, R 18, T 101F. There is an admitted drug exposure and you examine his eyes which are dilated. You shine the light in the eyes - if the pupil reacts, would that be consistent with anticholinergic or sympathomimetic toxidrome?
Answer: Anticholinergic exposure paralyzes pupillary constrictor muscles and causes dilated pupils that do not react to light. Think about when you go to the eye doctor's office. They put homoatropine in your eyes so that when they look with the slit lamp they can see the retina without interference from pupillary constriction. Sympathomimetic exposure like cocaine activates pupillary dilator muscles, the constrictors are still intact and will give a reflexive constriction to light. This patient has reactive pupils and by the mere fact is in Baltimore probability dictates a sympathomimetic exposure like cocaine.
Category: Orthopedics
Keywords: Salter Harris (PubMed Search)
Posted: 7/17/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
The Salter Harris Classification System is used in pediatric epiphyseal fractures. The higher the type of fracture the poorer the prognosis
Some common exam facts about Salter Harris Fractures are:
The Classification system as listed by Type:
A image of the fractures can be found on FP Notebook at http://www.fpnotebook.com/_media/OrthoFractureSalterHarris.jpg
Category: Gastrointestional
Keywords: Diverticular, bleeding, gastrointestinal (PubMed Search)
Posted: 7/3/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Diverticular Bleeding
Category: Orthopedics
Keywords: Odontoid, fracture (PubMed Search)
Posted: 6/26/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Odontoid Fractures:
There are three types of C2 odontoid fractures:

Category: Dermatology
Keywords: Toxicodendron dermatitis, treatment (PubMed Search)
Posted: 6/19/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Toxicodendron dermatitis:
This is the contact dermatitis caused by the plant genus Toxicodendronm, better known as Poison Ivy. Here are some types to prevent the dermatitis and how to treat it:
Category: Orthopedics
Keywords: Calcaneus Fracture, Bohler Angle (PubMed Search)
Posted: 6/13/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Calcaneus Fractures:
Calcaneus fractures can easily be missed on plain films and the true extent of the injury might not be appreciated until a CT is done. However, you can increase your change of picking up a calcaneal fracture by evaluating Bohler's Angle.
Lateral radiographs of the foot are needed to evaluate the Bohler angle. This is the angle made by drawing a line from anterior process of the calcaneus to the peak of the posterior articular surface and a second one drawn from the peak of the posterior articular surface to the peak of the posterior tuberosity. (See Picture) The average angle is 25-40°. Angles less than 25' are strongly suggestive of a fracture and the patient should probably get a CT of their foot if there is clinical suspicion.
Photo and additional discussion can be found at http://www.blackburnfeet.org.uk/hyperbook/trauma/calcanealFx/imaging.htm and on eMedicine -- Calcaneus Fractures by Scott Nicklebur, MD http://emedicine.medscape.com/article/1232246-overview
Category: Orthopedics
Keywords: Wound Care, Antiseptics (PubMed Search)
Posted: 6/5/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Wound Care:
Patients and many providers want to irrigate or wash a wound with an antiseptic solution in order to decrease the risk of infection. Most studies have shown that irrigation whether with tap water or sterile water is effective enough in reducing bacterial counts in a wound so does adding an antiseptic solution offer any additional benefit.
It turns out that hydrogen peroxide, and iodine based solutions can actually hinder wound healing as they causes delays in the migration and proliferation of fibroblasts at concentrations that are not even bactericidal. Chlorhexidine, and silver containing antiseptics [i.e.: silver sulfadiazine and silver nitrate] are bactericidal at concentrations that do not affect fibroblasts.
So in the end, if you feel the need to use an antiseptic, use chlorhexidine or a silver containing antiseptic. The use of hydrogen peroxide and iodine based solutions should be abandoned as they are not even bactericidal at concentrations that have profound affects on the fibroblasts.
Thomas, GS. Mechanisms of Delayed Wound Healing by Commonly Used Antiseptics. J Trauma 2009; 66:82-91
Category: Orthopedics
Keywords: Septic Arthritis (PubMed Search)
Posted: 5/29/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Septic Arthritis versus Arthritis:
Though CRP and ESR levels are significantly higher in patients that have septic arthritis, a 1998 study showed that there is extensive overlap between patients with septic arthritis crystal assoicated arthritis that both CRP and ESR have low sensitivity, specificity and predictive values. Peripherial WBC counts did not differ between the two disease processes..
The morale of the story: If you are suspecting septic arthritis you need to perform an arthorcentesis to analysis the synovial fluid. Systemic biomarkers can not support one diagnosis over the other.
Soderquist B, Jones I, Fredlund H, Vikerfors T: Bacterial or crystal-associated arthritis? Discriminating ability of serum inflammatory markers. Scand J Infect Dis 1998; 30: 591-596.
Category: Orthopedics
Keywords: Osteomyelitis (PubMed Search)
Posted: 5/22/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Osteomyelitis:
King RW, Johnson D: Osteomyelitis. In: eMedicine. WebMd; 2009.
Category: Orthopedics
Keywords: Radial Head, Fracture (PubMed Search)
Posted: 5/16/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Radial Head Fractures:
Radial head fractures can often be difficult to visualize on plain films especialing Mason Type 1 fractures (see prior pearl on classification system) which are nondisplaced. Often the only sign of a fracture will be a posterior fat pad sign which is always considered to be pathologic. The posterior fat pad lies outside the synovium of the elbow joint and is normally hidden in the fossa of the distal humerus preventing it from being seen on lateral films of a normal elbow. Trauma to the elbow that results in a intraarticular fracture (typically a radial head fracture) produces an intra-articular hemorrhage that distends the synovium and displaces the fat out of the fossa, producing the typical triangular radiolucent shadow posterior to the distal end of the humerus.
Elbow Fat Pad Sign in Atlas of Signs in Musculoskeletal Radiology
A. Gentili MD, M. Beller MD, S. Masih MD, L.L. Seeger MD
http://www.gentili.net/signs/11.htm
Category: Orthopedics
Keywords: Benzodiazepines, Back Pain, Sciatica (PubMed Search)
Posted: 5/8/2010 by Michael Bond, MD
(Updated: 5/9/2010)
Click here to contact Michael Bond, MD
Conservative Treatment of Back Pain:
Muscle relaxanats and benzodiazipnes are often used in the non-operative management of sciatica and non-specific low back pain. In fact, a 2003 Cochrane review concluded that muslce relaxanats were effective in the management of non-specific low back pain. However, a recent analysis of randomized trials reported little efficacy or only minor benefits with the use of benzodiazapines in treatment of low back pain.
A recent prospective, randomized, placebo-controlled, double-blinded trial conducted in Germany that enrolled a total of 60 patients found that the use of diazepam was equivilant to placebo in the reduction of distance of referred pain at day 7 of treatment. Diazepam was also noted on average to increase the length of stay of those patients hospitalized by 2 days (median hospital days of 8 for placebo versus 10 for diazepam), and the probablility of pain reduction on a visual analog scale by more than 50% was twice as high in the placebo group (p< 0.0015). Placebo reduced the patients pain more than diazepam.
Though the sample size was small; this study should really make one reevaluate the use of diazepam in the treatment of back pain. Early movement and discouraging bed rest have been associated with decreased back pain, so one mechanism by which benzodiazepines may make things work is by causing enough sedation to prevent early movement.
Brotz D, Maschke E, Burkard S, Engel C, Manz C, Ernemann U, Wick W, Weller M: Is there a role for benzodiazepines in the management of lumbar disc prolapse with acute sciatica? Pain 2010.
