Category: Ultrasound
Keywords: ONSD, POCUS, ocular exam, intracranial pressure (PubMed Search)
Posted: 2/24/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Point-of-care ultrasound (POCUS) measurement of the optic nerve sheath diameter (ONSD) has been shown to correlate with increases in intracranial pressure (ICP).
In adults, an ONSD measurement of less than 5 mm is considered normal, while a measurement greater than 6 mm suggests elevated ICP.
How to Measure the Optic Nerve Sheath Diameter:
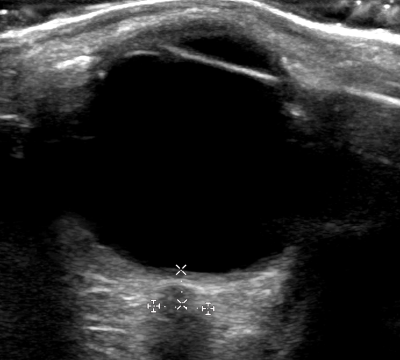
A small cross-sectional study examined whether ONSD measurements varied when taken at different depths. The findings indicated that ONSD increased by 0.32 mm at a depth of 4 mm and decreased by 0.54 mm at a depth of 2 mm.
These variations highlight the importance of maintaining a consistent measurement depth. To ensure accuracy and avoid misinterpretation, the ONSD should always be measured 3 mm posterior to the retina.
Gottlieb M, Kayarian F, Johnson J, Peksa GD. Differences in mean optic nerve sheath diameter measurements based on depth. Am J Emerg Med. 2024 Aug;82:197-198. doi: 10.1016/j.ajem.2024.06.013.
Category: Ultrasound
Keywords: aorta; POCUS; aortic dissection (PubMed Search)
Posted: 2/3/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
The suprasternal notch view is a valuable tool for assessing the aorta and identifying signs of thoracic aortic dissection. Proper technique is essential to obtain a clear image and improve diagnostic accuracy.
Steps to Obtain the Suprasternal Notch View:
Position the Patient:
Ideally, place the patient in a supine position.
If the patient cannot tolerate lying flat, the scan can be performed with the patient in an upright position.
Probe Selection & Orientation:
Use a phased array probe in cardiac mode.
Direct the probe marker slightly toward the patient’s left shoulder (or right hip if using abdominal mode).
Optimize Patient Positioning:
Ask the patient to extend their neck to improve visualization.
Having the patient rotate their head to the side may further enhance imaging.
Placing a rolled towel under the shoulders can help achieve optimal neck extension.
Probe Manipulation:
Angle the probe inferiorly toward the chest.
Adjust the depth to clearly visualize the aortic arch.
Kinnaman KA, Kimberly HH, Pivetta E, Platz E, Chudgar A, Adduci A, Stone MB, Rempell JS. Evaluation of the Aortic Arch from the Suprasternal Notch View Using Focused Cardiac Ultrasound. J Emerg Med. 2016 Apr;50(4):643-50.e1. doi: 10.1016/j.jemermed.2015.12.002.
Category: Ultrasound
Keywords: POCUS, ventricular arrythmia, nerve blocks (PubMed Search)
Posted: 1/20/2025 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Stellate Ganglion Blocks (SGB) have been reported in case reports as a last-line treatment for patients with refractory ventricular arrhythmias.
A recent multicenter study evaluated the efficacy and safety of SGB in managing refractory ventricular arrhythmias.
The study included 117 critically ill patients, with 9 on ECMO, 5 with Impella devices, and 15 with LVADs.
70% were given long-acting bupivacaine, 28% were given ropivacaine and 1 patient received lidocaine.
SGBs were primarily performed by anesthesiologists during short periods of when the patients were not in ventricular arrhythmia
The median 24-hour episodes of VT/VF decreased from 9.0 (interquartile range [IQR]: 3.0–31.0) pre-SGB to 1.0 (IQR: 0.0–5.0) post-SGB.
2 patients had complications; recurrent laryngeal nerve block with resultant hoarseness and brachial plexus block.
Limitations: This study was conducted in a controlled setting (ie not in active arrest, not in the emergency department) and involved a selective cohort. Randomized controlled trials (RCTs) are needed to validate these findings.
Chouairi F, Rajkumar K, Benak A, Qadri Y, Piccini JP, Mathew J, Ray ND, Toman J, Kautzner J, Ganesh A, Sramko M, Fudim M. A Multicenter Study of Stellate Ganglion Block as a Temporizing Treatment for Refractory Ventricular Arrhythmias. JACC Clin Electrophysiol. 2024 Apr;10(4):750-758. doi: 10.1016/j.jacep.2023.12.012.
Category: Ultrasound
Keywords: POCUS, vascular access, pediatrics (PubMed Search)
Posted: 12/16/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
In adult patients, ultrasound-guided long catheter IVs for difficult venous access have been shown to provide increased duration of use, reduced complication rates, and greater cost-effectiveness.
However, there are relatively few studies examining the use of ultrasound for IV access in pediatric patients.
A recent study, the DIAPEDUS study, investigated the success rate of peripheral IV access with and without ultrasound assistance in pediatric patients with difficult venous access.
The study included 110 pediatric patients. IVs were placed by 25 nurses and 6 pediatricians, each of whom had completed departmental training involving at least 20 ultrasound-guided IV placements prior to the study.
The results showed a significantly higher success rate on the first attempt with ultrasound-guided techniques (90% vs. 18%), along with reduced procedural time and fewer attempts overall.
Bottom Line: For patients with known difficult venous access, ultrasound-guided IV placement should be the first-line approach.
D'Alessandro M, Ricci M, Bellini T, Chianucci B, Calevo MG, Piccotti E, Moscatelli A. Difficult Intravascular Access in Pediatric Emergency Department: The Ultrasound-Assisted Strategy (DIAPEDUS Study). J Intensive Care Med. 2024 Mar;39(3):217-221. doi: 10.1177/08850666231199050
Bahl A, Johnson S, Hijazi M, Mielke N, Chen NW. Cost effectiveness of ultrasound-guided long peripheral catheters in difficult vascular access patients. J Vasc Access. 2024 Jul;25(4):1204-1211. doi: 10.1177/11297298231154297.
Category: Ultrasound
Keywords: POCUS, Lung ultrasound, EMS (PubMed Search)
Posted: 12/2/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Early treatment of congestive heart failure (CHF) exacerbations is associated with improved mortality rates and shorter hospital length of stay. Lung ultrasound is a valuable tool in diagnosing CHF exacerbations. Recently, several studies have explored the use of lung ultrasound in the prehospital settings to expedite diagnosis and treatment.
A recent systematic review and meta-analysis evaluated the diagnostic accuracy and clinical impact of prehospital lung ultrasound. The authors found similar test characteristics to point-of-care ultrasound (POCUS) performed in the emergency department.
The eight studies included in the analysis utilized varying lung ultrasound protocols, analyzing between 2 and 8 lung zones. Notably, only two studies involved paramedics performing the ultrasounds, yet no significant difference in diagnostic accuracy was observed.
Further research is needed to evaluate the training requirements for prehospital providers and the broader impact of prehospital lung ultrasound on treatment strategies and patient outcomes.
Category: Ultrasound
Keywords: POCUS; MSK; Achilles tendon (PubMed Search)
Posted: 11/18/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Achilles tendon injuries are commonly encountered in the emergency department. While MRIs are often unavailable, POCUS offers a quick and effective alternative for evaluating such injuries. In one review, the sensitivity of ultrasound for detecting complete Achilles tendon ruptures was 94.8%.
For the POCUS evaluation of the Achilles tendon:
- Place the patient in a prone position with their foot relaxed.
-Begin distally at the tendon’s insertion on the calcaneus and scan proximally, keeping the probe marker oriented toward the patient’s head.
-Next, obtain a transverse view by rotating the probe marker toward the patient’s right side.
-You can even do a sonographic Thompson’s Test!
Findings:
Complete Rupture: Displays as a full disruption of the tendon fibers.
Partial Tear: Shows intact tendon tissue with surrounding edema.
Tendinitis: Appears as a thickened tendon with increased vascularity on color Doppler imaging.
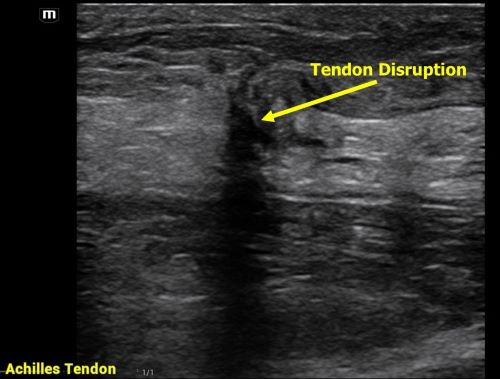
Aminlari A, Stone J, McKee R, Subramony R, Nadolski A, Tolia V, Hayden SR. Diagnosing Achilles Tendon Rupture with Ultrasound in Patients Treated Surgically: A Systematic Review and Meta-Analysis. J Emerg Med. 2021 Nov;61(5):558-567. doi: 10.1016/j.jemermed.2021.09.008.
Category: Ultrasound
Keywords: POCUS; ocular; neurology (PubMed Search)
Posted: 11/4/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
If significant orbital edema prevents visual assessment of the pupillary light reflex, ocular ultrasound can be a useful alternative.
Ocular Ultrasound Made Easy: Step-By-Step Guide - POCUS 101
Ramamoorthy T, Manu Ayyan S, Deb AK. Diagnostic Value of Point-of-Care Ultrasound-Guided Assessment of Relative Afferent Pupillary Defect in Adult Ocular Trauma Patients Presenting to the Emergency Department: A Prospective Cohort Study. J Ultrasound Med. 2024 Jul;43(7):1343-1351. doi: 10.1002/jum.16458.
Category: Ultrasound
Keywords: POCUS; Aspiration Risk; Intubation; Gastric Ultrasound (PubMed Search)
Posted: 10/20/2024 by Alexis Salerno Rubeling, MD
(Updated: 10/21/2024)
Click here to contact Alexis Salerno Rubeling, MD
Recent guidelines from anesthesia societies and recent literature emphasize the use of gastric POCUS for aspiration risk assessment. While the role of gastric POCUS in the emergency department is still being explored, one recent article highlighted its use in assessing patients with upper gastrointestinal bleeding (UGIB).
Performing Gastric POCUS:
Patient Position: Place the patient in the right lateral decubitus position, if unable can perform in supine position.
Probe Selection & Placement: Use a curvilinear probe in the sagittal position at the level of the subxiphoid process, similar to the longitudinal view of the proximal abdominal aorta.
Scanning Technique: Fan the probe left to right to assess the gastric antrum.
Interpretation of Gastric Antrum:
Empty Antrum: Appears as a "bull's eye" or flat, with no visible liquid inside.

Full Stomach: Distended antrum with floating contents.

Intermediate: Shows a small amount of anechoic fluid without floating contents.
Quantitative Evaluation:
It is also possible to perform a quantitative evaluation of the gastric antrum to further assess stomach contents, this may be more useful in patients with intermediate gastric antrum.
For more details, refer to the articles and videos cited.
Perlas A, Van de Putte P, Van Houwe P, Chan VW. I-AIM framework for point-of-care gastric ultrasound. Br J Anaesth. 2016 Jan;116(1):7-11. doi: 10.1093/bja/aev113.
Adrian RJ, Alsharif P, Shokoohi H, Alerhand S. Gastric Ultrasound in the Management of Emergency Department Patients with Upper Gastrointestinal Bleeding: A Case Series and Sonographic Technique. JEM 2024. doi.org/10.1016/j.jemermed.2024.07.015
Hot Tip How to Use Ultrasound to Assess the Gastric Antrum GUARD Protocol. https://www.youtube.com/watch?v=VH9VwVFY3yQ
Category: Ultrasound
Keywords: POCUS; FAST exam (PubMed Search)
Posted: 9/30/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
The Lipliner Sign is causing a lot of buzz within the ultrasound community, particularly concerning its implications for focused assessment with sonography for trauma (FAST) exams. This artifact arises from postprocessing techniques that enhance organ visualization but can inadvertently create a hypoechoic line that resembles free fluid leading to false positive exams.
Key points to note:
Nature of the Artifact: The Lipliner Sign manifests as a linear, hypoechoic outline around an organ, misleading clinicians into thinking there's free fluid present.
Differentiation: As mentioned in this case report, free fluid typically appears wedge-shaped and tapers as it moves into dependent areas, while the Lipliner Sign is more linear and closely follows the organ's contour.
Manufacturer Variability: This artifact can be observed across different ultrasound machine manufacturers.
Clinical Implications: Misinterpretation of the Lipliner Sign could lead to unnecessary interventions or misdiagnoses in trauma settings, underscoring the importance of thorough training and awareness of potential artifacts.
Category: Ultrasound
Keywords: musculoskeletal, POCUS, joint arthrocentesis, shoulder dislocation, joint injection (PubMed Search)
Posted: 8/19/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
To obtain a posterior shoulder view: Have the patient sit up with the back of the bed down. Position the curvilinear probe in the posterior aspect of the shoulder with the probe parallel to the patient bed, at the level just below the scapular spine and the marker towards the patient's left. You can have the patient rotate their arm to help you visualize the movement of the humeral head.
In the normal anatomy, the humeral head should be at the level of the glenoid (this is a patient's left shoulder):
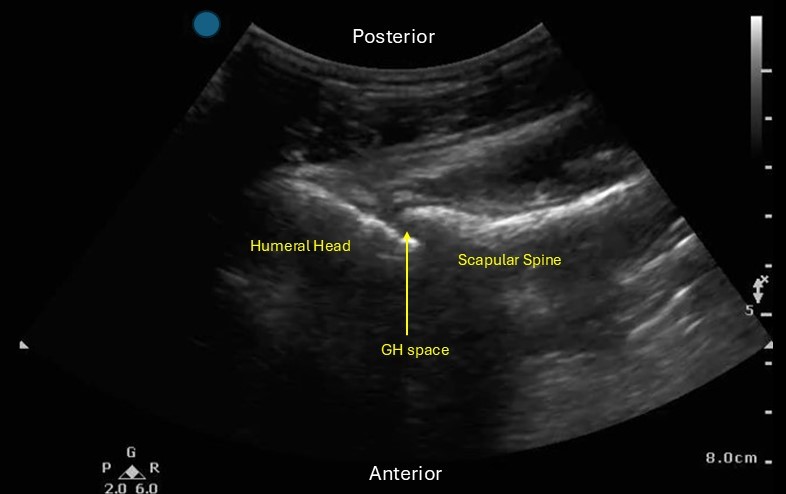
Locate the glenohumeral joint space. You can evaluate the GH joint for effusion, perform joint arthrocentesis/injection and look for signs of shoulder dislocation.
If you are evaluating for signs of a dislocation:
Posterior dislocation: the humeral head will be more SUPERFICIAL in the image than the scapular spine
Anterior dislocation: the humeral head will be DEEPER in the image than the scapular spine.
Category: Ultrasound
Keywords: POCUS, Trauma, Cardiac Tamponade, Pericardial Effusion, FAST exam (PubMed Search)
Posted: 8/5/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
In a critically ill trauma patient, the FAST exam is used to evaluate for potential internal injuries. Specifically, the subxiphoid view of the FAST exam helps assess for signs of pericardial tamponade. However, distinguishing between a pericardial effusion and an epicardial fat pad can be challenging.
One study indicated that the sensitivity of EPs in differentiating between effusion and fat pad was 73%, with a specificity of 44% when reviewing difficult patient video clips.
Here are some tips to help you distinguish between effusion and fat pad:
Change your view: Use the parasternal long axis view, which is more sensitive for effusion. Fat pads are usually anteriorly, and effusions tend to accumulate posteriorly in a supine patient.
Screen for other signs of tamponade: Adjust your subxiphoid view to visualize the IVC entering the right atrium, allowing better visualization of the right side of the heart.
Movement: Fat tends to move synchronously with the heart, whereas hemopericardium moves independently.
Echogenicity: Fat typically appears brighter on ultrasound, while blood tends to be less echogenic.
For further learning, refer to the supplemental Material from the referenced articles.
Bronshteyn YS, Hashmi N, Privratsky JR, Barbeito A. Blood or Fat? Differentiating Hemopericardium versus Epicardial Fat Using Focused Cardiac Ultrasound. Diagnostics (Basel). 2024 Apr 15;14(8):818. doi: 10.3390/diagnostics14080818. PMID: 38667464
Blaivas M, DeBehnke D, Phelan MB. Potential errors in the diagnosis of pericardial effusion on trauma ultrasound for penetrating injuries. Acad Emerg Med. 2000 Nov;7(11):1261-6. doi: 10.1111/j.1553-2712.2000.tb00472.x
Category: Ultrasound
Keywords: POCUS, dvt, vascular (PubMed Search)
Posted: 7/29/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS for DVT is a tricky examination.
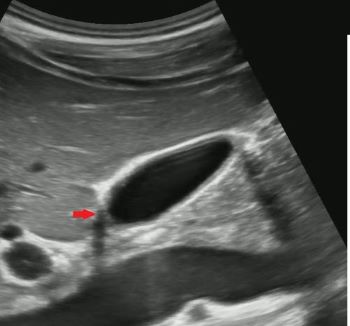
Exam of positive study on transverse:
Longitudinal Image showing clot:

Category: Ultrasound
Keywords: POCUS, fluid resuscitation, Inferior Vena Cava (PubMed Search)
Posted: 7/15/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Many may look at the Inferior Vena Cava (IVC) to get a sense of a patient's “fluid responsiveness.” However, there are many pitfalls to using the IVC. An article by Via et al outlines these pitfalls and is an interesting read!
To summarize, IVC can be affected by:
Bottom Line: Think twice before using IVC to evaluate for fluid responsiveness.
Via G, Tavazzi G, Price S. Ten situations where inferior vena cava ultrasound may fail to accurately predict fluid responsiveness: a physiologically based point of view. Intensive Care Med. 2016 Jul;42(7):1164-7. doi: 10.1007/s00134-016-4357-9.
Category: Ultrasound
Keywords: POCUS, GI, SBO (PubMed Search)
Posted: 7/8/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
POCUS has been shown to have a 92.4% sensitive (95% CI 89.0% to 94.7%) and 96.6% specific for identifying SBO.
Some characteristics of SBO include:
-dilated fluid filled bowel
-contents of bowel moving to and fro like a washer machine
-wall thickening and ability to see plicae circulares
- in high grade obstruction you may also notice intraperitoneal fluid near the dilated bowel.
Gottlieb M, Peksa GD, Pandurangadu AV, Nakitende D, Takhar S, Seethala RR. Utilization of ultrasound for the evaluation of small bowel obstruction: A systematic review and meta-analysis. Am J Emerg Med. 2018 Feb;36(2):234-242. doi: 10.1016/j.ajem.2017.07.085.
Category: Ultrasound
Keywords: POCUS; FAST exam; Trauma (PubMed Search)
Posted: 6/17/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Although the FAST exam can be helpful in expediting care of patients with intraabdominal injuries, there are a few pitfalls.
Pitfalls:
1. The FAST exam has a wide sensitivity which depends on sonographer skill and the patient's body habitus. It is best used as a “Rule In NOT Rule Out” exam.
2. The FAST exam is not good for identifying bowel injury or retroperitoneal bleeding and may not be able to pick up low volume hemoperitoneum.
3. The FAST exam is not able to identify the type of fluid e.g. ascites vs blood.
Some Tips for Performing the FAST exam:
1.Go slow, fan through the view completely. In the RUQ view make sure you are evaluating the liver tip.
2. Place the patient in slight Trendelenburg.
3. If you have clinical concern for injury, don't stop at a negative FAST.
Savatmongkorngul S, Wongwaisayawan S, Kaewlai R. Focused assessment with sonography for trauma: current perspectives. Open Access Emerg Med. 2017 Jul 26;9:57-62. doi: 10.2147/OAEM.S120145.
Category: Ultrasound
Keywords: Abdomen, ultrasound, trauma, contrast (PubMed Search)
Posted: 5/23/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This very small study looked at the utility of using IV contrast media to enhance abdominal sonography in identifying injuries in blunt abdominal trauma patients. The comparison was CT scanning of the abdomen to identify injuries. The study concluded:
“With the addition of contrast and careful inspection of solid organs, abdominal sonography with contrast performed by the emergency physician improves the ability to rule out traumatic findings on abdominal CT. CEUS performed by emergency physicians may miss injuries, especially in the absence of free fluid, in cases of low-grade injuries, simultaneous injuries, or poor-quality examinations.”
To me, this is a limited study and the technique is not ready for wide spread use but further study is warranted.
Viviane Donner MD, Julian Thaler MD, Wolf E Hautz Prof. Dr.Med, MME, Thomas Christian Sauter Prof. Dr.Med, MME, Daniel Ott MD, Karsten Klingberg MD, Aristomenis K Exadaktylos Prof.Dr.Med, Beat Lehmann MD
First published: 19 April 2024
Journal of the American College of Emergency Physicians OpenVolume 5, Issue 2
Category: Ultrasound
Keywords: Pleural Effusion; POCUS (PubMed Search)
Posted: 4/22/2024 by Alexis Salerno Rubeling, MD
(Updated: 4/29/2024)
Click here to contact Alexis Salerno Rubeling, MD
How do you look for signs of a pleural effusion with ultrasound?
Place your ultrasound probe in the mid axillary line with the probe marker placed towards the patient's head.
Find the movement of the diaphragm and scan just above the diaphragm.
In normal lung, air scatters the ultrasound signal, and you are not able to see structures above the diaphragm.
With a pleural effusion, you can see:
Category: Ultrasound
Keywords: POCUS; Lumbar Puncture; Neurology (PubMed Search)
Posted: 4/15/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
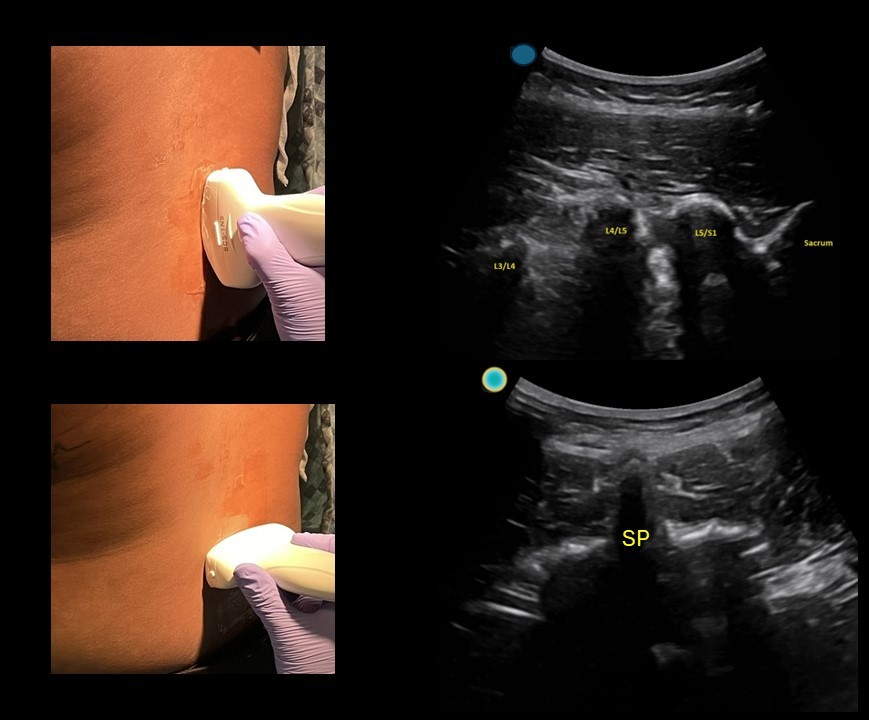
Simple tool to help improve your next lumbar puncture: Use ultrasound for site marking.
This can be done in a patient sitting up or laying on their side.
-First start with the probe marker midline towards the patient's head and use the ultrasound to identify the L4/L5 and L3/L4 space.
-Use a surgical pen away from the gel to mark midline on both sides of the probe, using the midline marker on the ultrasound probe. You can use m mode to help you identify the middle of the image when using a curvilinear probe.
-Then rotate the probe towards the patient's left and use the ultrasound to identify the midline point (spinous process)
-Use a surgical pen away from the gel to mark midline on both sides of the probe, using the midline marker on the ultrasound probe.
-Clean off the gel, connect the skin markings and use a 3 cc syringe to mark the center of the crosshair.
-Sterilize and start your LP!
Category: Ultrasound
Keywords: POCUS; Ultrasound Artifacts (PubMed Search)
Posted: 4/1/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Ultrasound artifacts can sometimes be helpful, but sometimes they can be misleading.
For example:
1)Does this patient have a gallstone?
No, this is edge artifact! This is due to the ultrasound signals refracting off the side of the gallbladder wall.

No, this is side lobe artifact! This is due to a bright reflector outside of the central beam of the ultrasound signal that the machine mistakenly places with in the center of the beam. Side lobe artifact can occur near fluid filled masses such as the gallbladder and bladder.

No, this is mirror artifact!! This is due to ultrasound signals bouncing off a highly reflective surface such as the diaphragm. The ultrasound machine misinterprets the time delay from the reflected ultrasound signal as a structure deeper in the image.
Category: Ultrasound
Keywords: ultrasound, nerve block (PubMed Search)
Posted: 3/11/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
What happens if you have a patient who steps on a nail? How can you make this procedure easier for you and the patient?
– Use a Posterior Tibial Nerve Block! !
To Perform This Procedure:
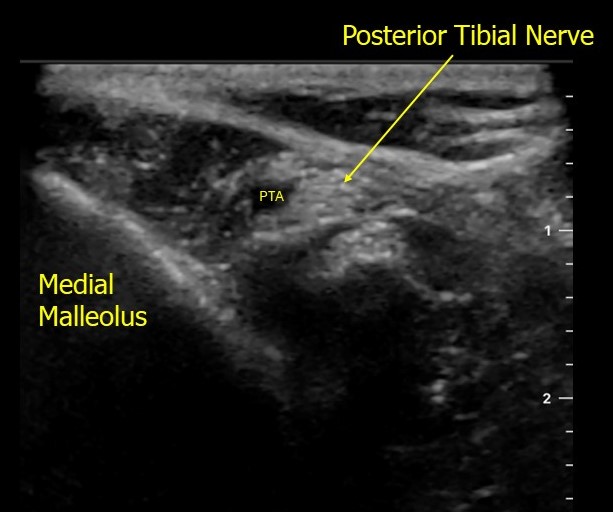
https://www.acep.org/patient-care/map/map-posterior-tibial-nerve-block-tool
Tibial — Highland EM Ultrasound Fueled pain management (highlandultrasound.com)
