Category: Administration
Keywords: Communication, Teamwork (PubMed Search)
Posted: 1/28/2026 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
How well does your ED care team communicate? For some high yield strategies and reasons for improvement, read on…
To explore effective and ineffective communication in the ED and its impact of patient care, physician and nurses from several academic EDs completed an online anonymous survey, then attended focus group sessions. Responses highlighted the following themes:
1: Situations, built physical environment, and medium of communications all impact quality of communication.
2: Core elements of desired professional communication include respect, closed-loop communication, and attention, often conveyed through non-verbal behaviors.
3: Poor communication begets poor communication in later interactions
4: Effective communication is seen as fundamental to patient care but also has impacts beyond patient care
5: Clinician gender and gender dyads influence communication dynamics, age and experience dyads did not.
Do any of these themes resonate with you? What can you do within your department to improve physician-nurse communication and the care you provide?
Jones DC, Phillips J, Graveson A, et al. Emergency Physician and Emergency Nurse Communication in the Emergency Department: A Mixed-methods Study. West J Emerg Med. 2026;27(1)91–98.
Category: Administration
Posted: 1/10/2026 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Plain films are often the first imaging test ordered in patient’s with knee injuries.
Plain films do NOT directly show the ACL but may reveal indirect signs of an ACL tear.
Key Plain Film Findings:
1) Effusion
ACL injury generates a large joint effusion (swelling/hemarthrosis). The presence of a fat/fluid interface (lipohemarthrosis) suggests associated bone injury.
This may be seen as joint fluid on the plain film lateral view. This view is best obtained with the patient in the supine position. This allows a layering of fluid in the suprapatellar bursa. A fat/fluid level indicates the presence of a lipohemarthrosis, signifying the likelihood of an intraarticular fracture.
http://radiologykey.com/wp-content/uploads/2019/03/f10-02ad-9781437727791.jpg
( A ) The normal suprapatellar bursa is seen on the lateral view as a line extending obliquely anterior and superior from the superior/posterior surface of the patella to the posterior surface of the quadriceps tendon.
(B) A small to moderate-sized effusion.
(C) A larger effusion.
In (D) the quadriceps tendon is bulged outward by an even larger joint effusion.
In the correct clinical setting, the presence or absence of a new fusion can be highly suggestive of ACL tear. Effusion can usually accurately be assessed on both physical exam and the lateral plain film. The absence of a knee effusion makes acute tear of the ACL unlikely as clinical practice suggests a rapidly developing hemarthrosis. Effusion of the knee may be associated with other entities such as intraarticular fracture or underlying arthritis. Typically, patients with acute ACL tears are young and do not have chronic infusions. Most acute meniscal tears and chondral injuries do not develop acute large effusions due to lack of significant vascularity.
Category: Administration
Keywords: industry sponsored, money, research, PI (PubMed Search)
Posted: 12/27/2025 by Robert Flint, MD
(Updated: 12/31/2025)
Click here to contact Robert Flint, MD
This study looked at industry sponsored payments to EM physician through non-covered entities (ie not directly to physician or through an academic institution). It found a $100 million increase from 2015-23 in this payment model. It appears that private equity is not the only money entering emergency medicine in the past decade.
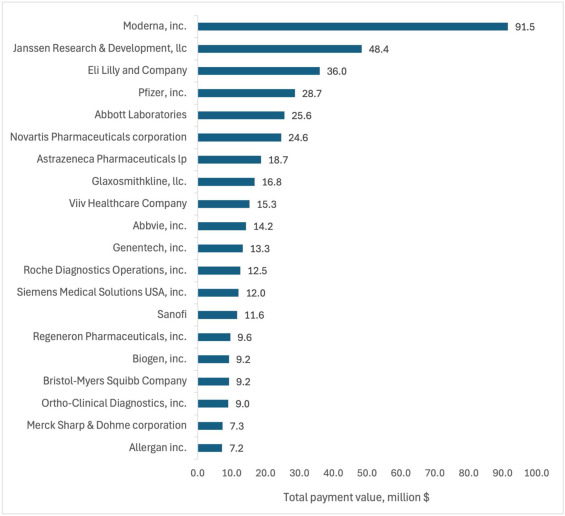
Total value of Industry-Sponsored Research Payments (ISRPs) by company. The 20 companies with highest total ISRPs awarded to emergency physician PIs.
Rizer, Nicholas W et al.
Journal of Emergency Medicine, Volume 79, 21 - 30
Category: Administration
Keywords: holidays, scheduling, daily volumes, behavioral health (PubMed Search)
Posted: 12/18/2025 by Steve Schenkel, MPP, MD
(Updated: 12/24/2025)
Click here to contact Steve Schenkel, MPP, MD
How do ED volumes change around the winter holidays?
The anticipated US pattern is one of lower volumes on the holidays themselves followed by increased volumes on the first weekdays after.
Behavioral health visits show similar patterns – a drop before the holidays and perhaps an increase after the holiday.
Many departments adjust scheduling accordingly, reducing staff on major holidays, which has the added benefit of allowing more people to enjoy the holiday.
This pattern isn’t necessarily what happens everywhere, though. At least one Australian ED reported increased visits over the holidays.
While not perfect, the best guide to future holiday volumes remains past experience thoughtfully applied.
Agoritsas A, et al. Predicting Flow in the Pediatric Emergency Department: Are Holidays Lighter? Annals of Emergency Medicine 2015, Volume 66, Issue 4, S143
Halpern, Scott D. et al. Emergency department patterns in psychiatric visits during the holiday season. Annals of Emergency Medicine 1994, Volume 24, Issue 5, 939 – 943.
Leming, M. et al. Effect of Holidays on the Patient Severity and Census In the Emergency Department. Annals of Emergency Medicine 2010, Volume 56, Issue 3, S128
Silverman M. Holiday Scheduling: Fair and Balanced. EP Monthly, Dec 1, 2010. https://epmonthly.com/article/holiday-scheduling-fair-and-balanced/.
Zheng, W., Muscatello, D.J. and Chan, A.C. (2007), Deck the halls with rows of trolleys … emergency departments are busiest over the Christmas holiday period. Medical Journal of Australia, 187: 630-633. https://doi.org/10.5694/j.1326-5377.2007.tb01451.x
Category: Administration
Keywords: MOUD, racial and sex disparities (PubMed Search)
Posted: 12/11/2025 by Kevin Semelrath, MD
(Updated: 12/20/2025)
Click here to contact Kevin Semelrath, MD
This study looked for differences in prescribing patterns of suboxone for different opioid related complaints- withdrawal, overdose, and other related complaints.
In the overall cohort, all racial minorities, except Native American, and female patients had a lower likelihood of being prescribed suboxone for any opioid related complaint compared to white, male patients.
However, when they did subgroup analysis, patients presented for withdrawal symptoms had increased rates of buprenorphrine administration and prescribing that eliminated the racial disparities, but the gender disparities remained.
MOUD remain a key factor in allowing patients with OUD to achieve long-term sobriety, but there are still persistent barriers to appropriate prescribing
Chhabra N, Smith D, Parde N, Hsing-Smith N, Bianco JM, Taylor RA, D'Onofrio G, Karnik NS. Racial, ethnic, and sex disparities in buprenorphine treatment from emergency departments by discharge diagnosis. Acad Emerg Med. 2025 Sep;32(9):985-993. doi: 10.1111/acem.70035. Epub 2025 Apr 25. PMID: 40277252; PMCID: PMC12353228.
Category: Administration
Keywords: artificial intelligence, emergency department, emergency practice, machine learning (PubMed Search)
Posted: 11/26/2025 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
Food for thought on this Thanksgiving eve…
AI is rapidly being integrated into the practice of emergency medicine, as well as many other medical specialties. Similar to the adage, "you are what you eat," AI is what we feed it. See below for an introduction to the various levels of bias contributing to the machine learning process:
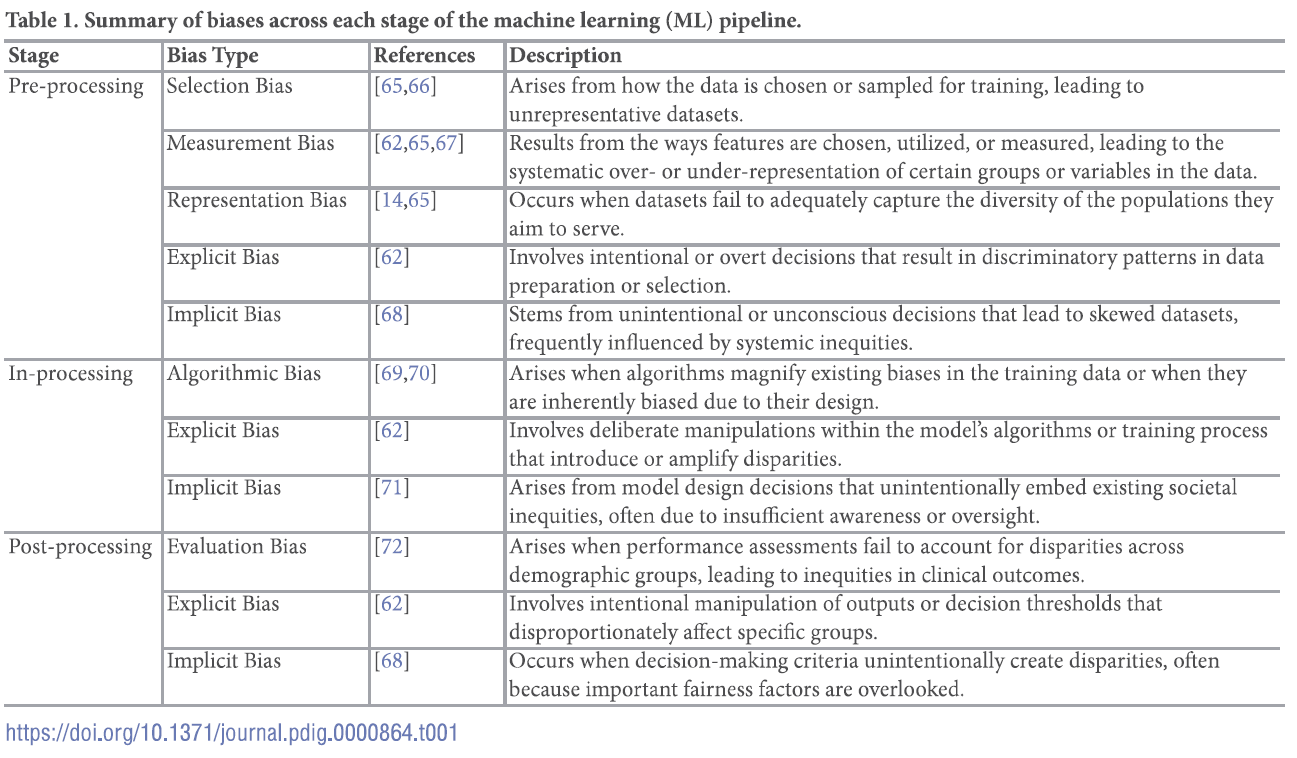
For a deep dive into the world of bias in AI, see referenced article.
Chinta SV, Wang Z, Palikhe A, Zhang X Kashif A, Smith MA, et al. (2025) AI-driven healthcare: A review on ensuring fairness and mitigating bias. PLOS Digit Health 4(5): e0000864. https://doi.org/10.1371/journal.pdig.0000864
Category: Administration
Posted: 11/15/2025 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
This abstract from ACEP's most recent research forum looked at the effect a patient's preferred language had on ED LOS, rate of admission, hospital length of stay and resource utilization both in the ED and the hospital.
Overall, those patients who spoke English as their primary language had lower ED LOS, less testing done in the ED, but if they got admitted they had the longest hospital LOS. Patients who preferred Spanish language had the shortest hospital LOS and were most likely to be discharged home with no services. Non-English/non-Spanish languages had the longest ED LOS and highest admission rates and had similar resource use as patients who preferred Spanish
This abstract opens the door for further research into what the underlying cause of these disparities are.
Zimmerman, T. et al.
Annals of Emergency Medicine, Volume 86, Issue 3, S3 - S4
Category: Administration
Keywords: complaint, service recovery, administration (PubMed Search)
Posted: 10/20/2025 by Steve Schenkel, MPP, MD
(Updated: 10/22/2025)
Click here to contact Steve Schenkel, MPP, MD
Do you ever have to manage a complaint? Perhaps a patient complaint?
It can be tough to hear a complaint. Emotions can run high. And then the ability to listen and respond can fade.
It helps to have a shorthand to guide the response.
Customer service literature provides one that often works well: LAST, for Listen, Apologize, Solve, and Thank.
This article gets at the basic idea (while adding one or two additional items): Steinman, HK. A Method for Working with Displeased Patients—Blast. J Clin Aesthet Dermatol. 2013 Mar;6(3):25–28. https://pmc.ncbi.nlm.nih.gov/articles/PMC3613270/.
Category: Administration
Keywords: Operations, Disposition, Decision-Making, Disparities, (PubMed Search)
Posted: 9/24/2025 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
This publication is a retrospective cross-sectional study conducted based on data collected during January 1–December 31, 2019 from a large, academic ED in the Southeastern US with the following research questions and results:
Interesting point regarding how disposition decisions are different from the ample evidence on disparities within triage decisions: The presence of disparities in disposition decisions is noteworthy not only because of their potentially long-term effects on patients’ health, but also because unlike some of the other decisions made in the ED such as triage, they are typically made under relatively less time pressure with deliberation and input from multiple individuals, conditions that are known to make biases less likely.
Authors propose pursing further research to elucidate the factors that contribute to these findings, instituting systems to alert providers in real time to the presence of conditions that could exacerbate disparities in ED care, and including the measurement of disparities along sex, race and ethnicity into health care operations data.
Cheng Q, Argon NT, Evans CS, Lin P, Linthicum B, Liu Y, Mehrotra A, Patel MD and Ziya S (2024) An Investigation into Demographic Disparities in Emergency Department Disposition Decisions. Production and Operations Management 34(4): 688–696.
Category: Administration
Posted: 9/20/2025 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
Systemic racism and institutional bias affect all aspects of medicine. This position paper from 2022 highlights some of the disparities present within the EM Clinical Ultrasound community. The authors identified several areas of concern regarding the make up of the leadership of the CU community, and importantly suggest several ways to create a more equitable specialty.
Javier Rosario, Resa E. Lewiss, Lori A. Stolz, Marina Del Rios, Josie Acuña, Srikar Adhikari, David Amponsah, Almaz S. Dessie, Michael Gottlieb, Robert D. Huang, Jodi Jones, Adaira Landry, Rachel B. Liu, Lorraine Ng, Nova L. Panebianco, Anthony J. Weekes, Starr Knight,
Creating a more racial-ethnic inclusive clinical ultrasound community,
The American Journal of Emergency Medicine,
Volume 54,
2022,
Pages 208-211,
ISSN 0735-6757,
https://doi.org/10.1016/j.ajem.2022.02.015.
(https://www.sciencedirect.com/science/article/pii/S0735675722000985)
Category: Administration
Keywords: AI, LLM, large language model, artificial intelligence, search (PubMed Search)
Posted: 8/27/2025 by Steve Schenkel, MPP, MD
(Updated: 2/8/2026)
Click here to contact Steve Schenkel, MPP, MD
Have you tried using Large Language Model (LLM) driven searches in clinical practice, for example, OpenEvidence, ChatGPT, or Claude?
A recent paper, far from medicine, argues that LLM searching has changed the way we think about search and what we expect from search.
We have moved from searching for sources to searching for the information contained within sources. With this, our expectations have changed – we expect search to provide answers, not documents.
With this shift, the foundations of trust have shifted. Rather than finding a document that provides the answer, and which is supported by the integrity of the authors and publishers – and which the reader can evaluate – LLMs provide an answer, often with little evidentiary base to support that answer.
Some LLMs do a better job of referencing sources in support of their answers than others. This argument suggests how important such transparency can be.
Find the full conversation here, https://publicera.kb.se/ir/article/view/52258, in Sundin O, Theorising notions of searching, (re)sources and evaluation in the light of generative AI, Information Research 2025, vol 30.
Sundin O, Theorising notions of searching, (re)sources and evaluation in the light of generative AI, Information Research 2025, vol 30. https://publicera.kb.se/ir/article/view/52258
Category: Administration
Posted: 8/23/2025 by Hanna Hussein, MD
(Updated: 2/8/2026)
Click here to contact Hanna Hussein, MD
As emergency clinicians, we frequently encounter patients from diverse cultural and religious backgrounds, including a growing Muslim population. This guide outlines key pharmacological considerations when caring for Muslim patients, focusing on the presence of alcohol and porcine-derived gelatin in commonly prescribed medications, two ingredients that may conflict with Islamic beliefs. Drawing from real cases and institutional data at Jefferson Health, the authors highlight how such conflicts can lead to medication refusal, delays in care, and decreased adherence.
The article presents a practical and EM-friendly framework for identifying potentially problematic ingredients using tools like the FDA’s National Drug Code (NDC) and the DailyMed database. It also offers substitution strategies and highlights that alternatives often exist, such as switching from suspensions to tablets or selecting alcohol-free formulations. Importantly, the authors explore the Islamic principles of necessity (darura) and transformation (istihalah), which allow for flexibility in life-saving situations. By integrating cultural awareness into our prescribing habits and leveraging simple EHR strategies, such as tagging “pork” as an allergy to trigger alerts, we can provide more inclusive, respectful, and effective care in the ED without adding significant burden to clinical workflows.
Category: Administration
Keywords: Patient Experience, Patient Satisfaction, CMS Evaluation, ED Evaluation, (PubMed Search)
Posted: 7/22/2025 by Mercedes Torres, MD
(Updated: 7/23/2025)
Click here to contact Mercedes Torres, MD
Shout out to UMEM alum Diane Kuhn, MD, PhD as the first author of this recent publication…
She and her colleagues examined the factors that contribute to ED patient experience scores, uncovering several which are not considered in the current CMS evaluative framework. See the editor's (our very own Stephen Schenkel, MD, MPP) capsule summary below:
What is already known on this topic? Medicare plans nationally standardized Emergency Department (ED) Patient Experience scores (ED
CAHPS) to allow comparison across sites.
What question this study addressed. Are there clinical and operational ED characteristics for which ED patient experience scores ought to be adjusted?
What this study adds to our knowledge. Based on 58,622 ED visits from one system, patients arriving in pain were less satisfied and those receiving radiologic studies had a positive experience.
How this is relevant to clinical practice. Influences on patient satisfaction are multifactorial and many are outside the control of the ED. Comparing EDs based on patient experience is complex and prone to misinterpretation.
As the authors point out, If patients placed in a hallway bed have a more negative experience simply due to the location in the department, or patients arriving in pain have a more negative experience regardless of ED care, then some EDs will face more challenges than others in achieving optimal patient experiences.
The current CMS evaluative framework may inherently disadvantage certain EDs, including those with limited physical space relative to their patient volumes, such as safety-net hospitals, or those that care for a high proportion of patients experiencing chronic pain. Is this fair? Does it reflect what CMS is trying to evaluate? Are there alternatives?
Kudos to Dr. Kuhn on her insightful publication and Dr. Schenkel for his expert editing!
Kuhn, Diane et al. Use of Hallway Beds, Radiology Studies, and Patients in Pain on Arrival to the Emergency Department Are Associated With Patient Experience, Annals of Emergency Medicine, Volume 86, Issue 2, 150 - 157. https://doi.org/10.1016/j.annemergmed.2024.11.020
Category: Administration
Keywords: insurance, malpractice, claims-made, occurrence, lawsuit (PubMed Search)
Posted: 6/25/2025 by Steve Schenkel, MPP, MD
(Updated: 2/8/2026)
Click here to contact Steve Schenkel, MPP, MD
Malpractice Insurance comes in two varieties: Occurrence and Claims-made.
Occurrence covers lawsuits for which the event occurs while the insurance is active.
Claims-made only covers lawsuits for which the insurance is active both during the event and when the lawsuit is announced. It’s less expensive because the coverage period is both shorter and more definitive.
This is an important distinction when an event and a lawsuit may be separated by years, as happens with medical malpractice.
Occurrence is the “good” kind.
Claims-made requires a tail to cover any claims brought after the insured period ends.
Read how this can go awry in Emergency Medicine at Leon Adelman’s April post here, https://substack.com/home/post/p-161044772.
Category: Administration
Posted: 6/19/2025 by Kevin Semelrath, MD
(Updated: 6/21/2025)
Click here to contact Kevin Semelrath, MD
Despite ongoing attacks against the principles of DEI, most medical organizations know and have acknowledged the necessary role of creating a more diverse, equitable and inclusive environment. Doing so requires both a bottom up and a top down approach, with engaged leadership supporting active efforts to increase diversity
This author, published just this month in Annals, details a unique and exciting way to engage resident leadership in the DEI efforts of an emergency department, with the creation of a Chief Resident for DEI role. They detail the creation of the role, and describe some of the roles and responsibilities and thoughfully discuss some of the limitations. It's an exciting and thought provoking read.
Ali, Fahad et al.
Annals of Emergency Medicine, Volume 85, Issue 6, 491 - 497
Category: Administration
Keywords: Artificial intelligence, Emergency department, emergency practice (PubMed Search)
Posted: 5/27/2025 by Mercedes Torres, MD
(Updated: 5/28/2025)
Click here to contact Mercedes Torres, MD
AI is probably already being used in your ED, like it or not…
This article is an excellent review of the ways that AI can be used in emergency medicine. (See blue boxes in the figure below for a visual representation of opportunities for AI to augment emergency care from start to finish.) The authors note that there will always be a role for human physicians in EDs; AI can serve as an adjunct rather than a replacement for physician care. Physicians should strive to be informed leaders in AI development to ensure it is performed in a cautious, thoughtful, patient-centered manner.
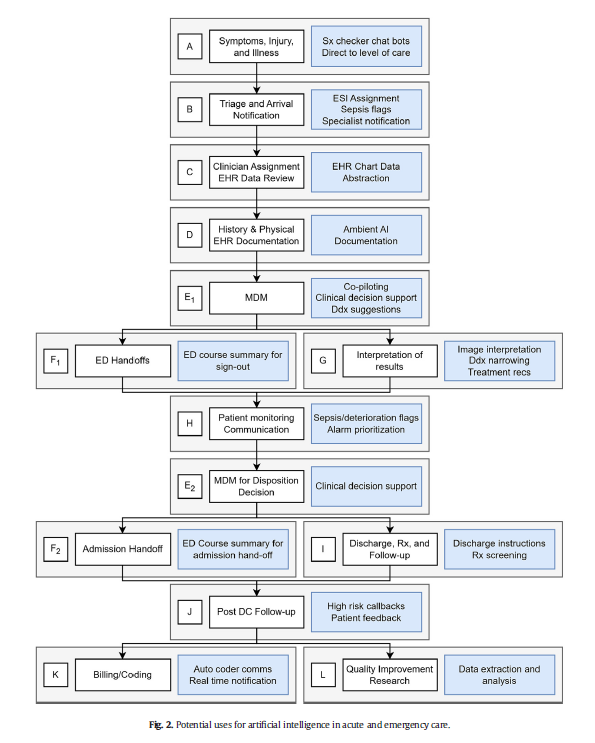
Marika M. Kachman, Irina Brennan, Jonathan J. Oskvarek, Tayab Waseem, Jesse M. Pines. How artificial intelligence could transform emergency care. The American Journal of Emergency Medicine, Volume 81, 2024, Pages 40-46, https://doi.org/10.1016/j.ajem.2024.04.024.
Category: Administration
Posted: 5/16/2025 by Kevin Semelrath, MD
(Updated: 5/17/2025)
Click here to contact Kevin Semelrath, MD
We talk a lot about the efforts within our profession at increasing diversity, inclusion and equity, but this study grants a unique perspective on that by surveying our patients on their experience of DEI in the ED.
The authors surveyed about 1700 patients, with 800 responding, at a large ED in Detroit. The population was majority black, and had a wide degree of variability in socioeconomic status.
Overall the patients felt that the staff had no biased or prejudiced interactions with people of different races. However, they felt that people from lower socioeconomic levels, transgender patients, and those that had mental health issues were treated unfairly. They also noted (about17% of respondents) harassment of ED staff by another patient.
Kavya Davuluri 1,?, Nikhil Goyal 2,3, Harold Gomez Acevedo 4, Jason Folt 2, Namita Jayaprakash 2,5, Michelle Slezak 2, Martina T Caldwell 2
PMCID: PMC9482342 PMID: 36176501
Category: Administration
Keywords: CT scanning, cancer risk, administration, EMR, diagnostic algorithms (PubMed Search)
Posted: 4/23/2025 by Steve Schenkel, MPP, MD
(Updated: 2/8/2026)
Click here to contact Steve Schenkel, MPP, MD
You may have seen the headline.
93 million CT examinations conducted on 62 million US patients in 2023 projected to lead to 103000 new cancer diagnoses accounting for 5% of new cancers.
The details of the modeling can be found here, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2832778.
What does this have to do with administration?
The solutions rely on administrative involvement:
There’s an editorial here, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2832782 and a commentary with interviews that put the findings nicely in context here https://arstechnica.com/health/2025/04/ct-scans-could-cause-5-of-cancers-study-finds-experts-note-uncertainty/ (including pointing out that lifetime risk of cancer in the US is 40% and the increase from CT scanning on the order of 0.1% / scan).
Smith-Bindman R, Chu PW, Firdaus HA, et al. Projected lifetime cancer risks from current computed tomography imaging. JAMA Intern Med 2025; doi:10.1001/jamainternmed.2025.0505.
Category: Administration
Posted: 4/19/2025 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
This study was the first look at the author's experiences with racial disparities in head and neck trauma in children. It looked at community EDs, and found that white children were more likely to be diagnosed with concussion compared to black children. White children were more likely to be seen as a result of sports or motor vehicle accidents, while black children were more likely to be seen as a result of an assault.
This study revealed the need for further research into the cause of the disparities in care that they identified.
Wallace, Jessica et al.
Journal of Emergency Medicine, Volume 59, Issue 6, 783 - 794
Category: Administration
Posted: 3/29/2025 by Brian Corwell, MD
(Updated: 3/30/2025)
Click here to contact Brian Corwell, MD
A recent cohort study performed by the NCAA and US Department of Defense looked at NCAA athletes and military cadets who had suffered a concussion.
The study included 1661 NCAA athletes and military cadets, mean age was about 18 years, and 45% were women.
In these groupings, 813 people took over-the-counter pain relievers after their concussion and 848 people did not take any pain relievers.
Analgesics used included medications such as acetaminophen or NSAIDs such as ibuprofen.
Acetaminophen (n = 600), NSAIDs (n = 75), and those taking both (n = 78).
1) 50% recovery
