Category: Visual Diagnosis
Posted: 3/25/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
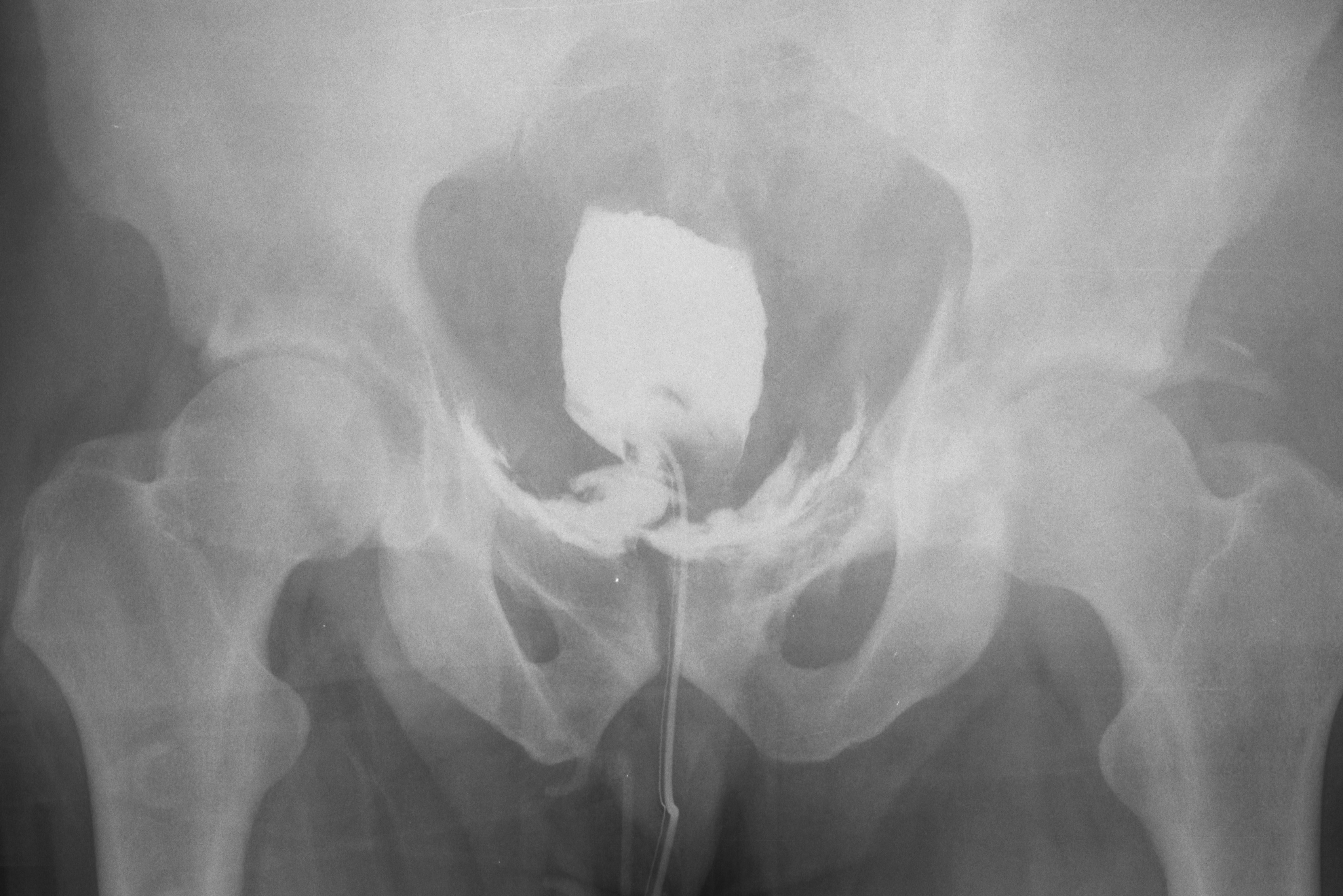
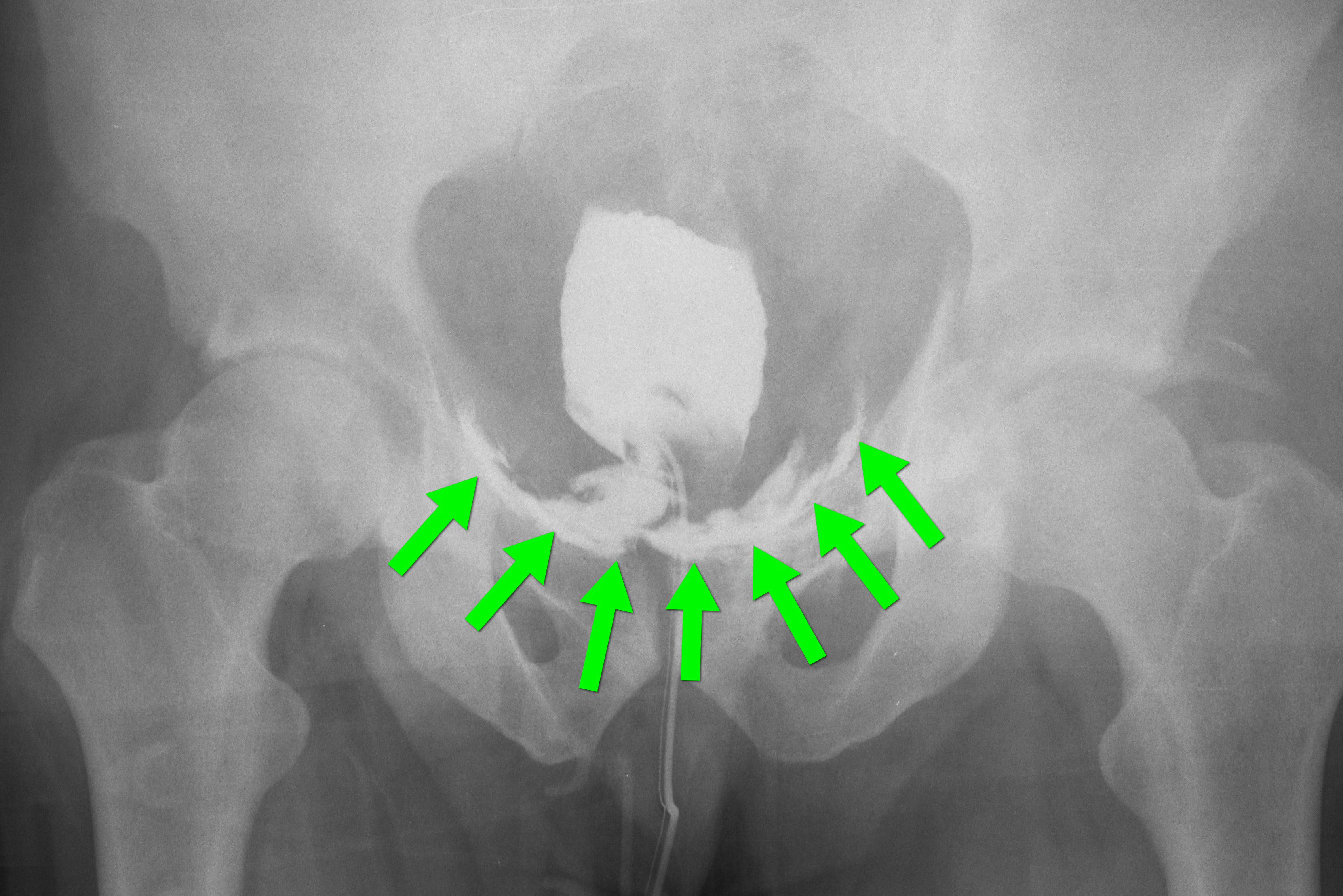
35 year-old male presents after a motor vehicle crash. No blood seen at the meatus of the penis and a Foley catheter is placed (see photo below). What's the next diagnostic step?

Answer: Retrograde cystogram
Traumatic bladder rupture
Gross or microscopic hematuria (>50 RBCs per high-power field) following blunt trauma requires a retrograde cystogram to evaluate for bladder injury. If blood is present at the meatus, however, urethral injury (not discussed) should be suspected and retrograde urethrogram should be performed before passing a Foley catheter.
A retrograde cystogram is performed by infusing diluted contrast into the bladder (200-400 mL) to gently distend the bladder and allow visualization of potential rupture(s). A CT scan of the abdomen and pelvis is then performed to determine if any contrast has leaked from the bladder; alternatively an AP pelvis can also be used, but is not as sensitive as CT.
Traumatic bladder ruptures are categorized as either intra-peritoneal or extra-peritoneal (note: X-ray below demonstrates extra-peritoneal rupture).
Treatment for bladder rupture:
Prognosis is typically good for either injury.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A 56-year-old woman with a history of psoriasis presents with fever, nausea, and painful pin-point pustules on an erythematous base. Her dermatologist recently reduced her prednisone dose. What's the diagnosis?

Answer: Pustular psoriasis
Pustular psoriasis
Occurs in patients with psoriasis, classically occurring after a decrease in dose or cessation of systemic steroids
Symptoms include:
These lesions can eventually drain and desquamate, leaving large patches of exposed dermis.
Complications include:
Patients may be admitted for supportive care and treatment with disease-modifying antirheumatic drugs (DMARDs) such as cyclophosphamide or methotrexate.
REFERENCE
L Naldi, D Gambini, The clinical spectrum of psoriasis, Clinics in Dermatology, Volume 25, Issue 6, November–December 2007, Pages 510-518
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/11/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
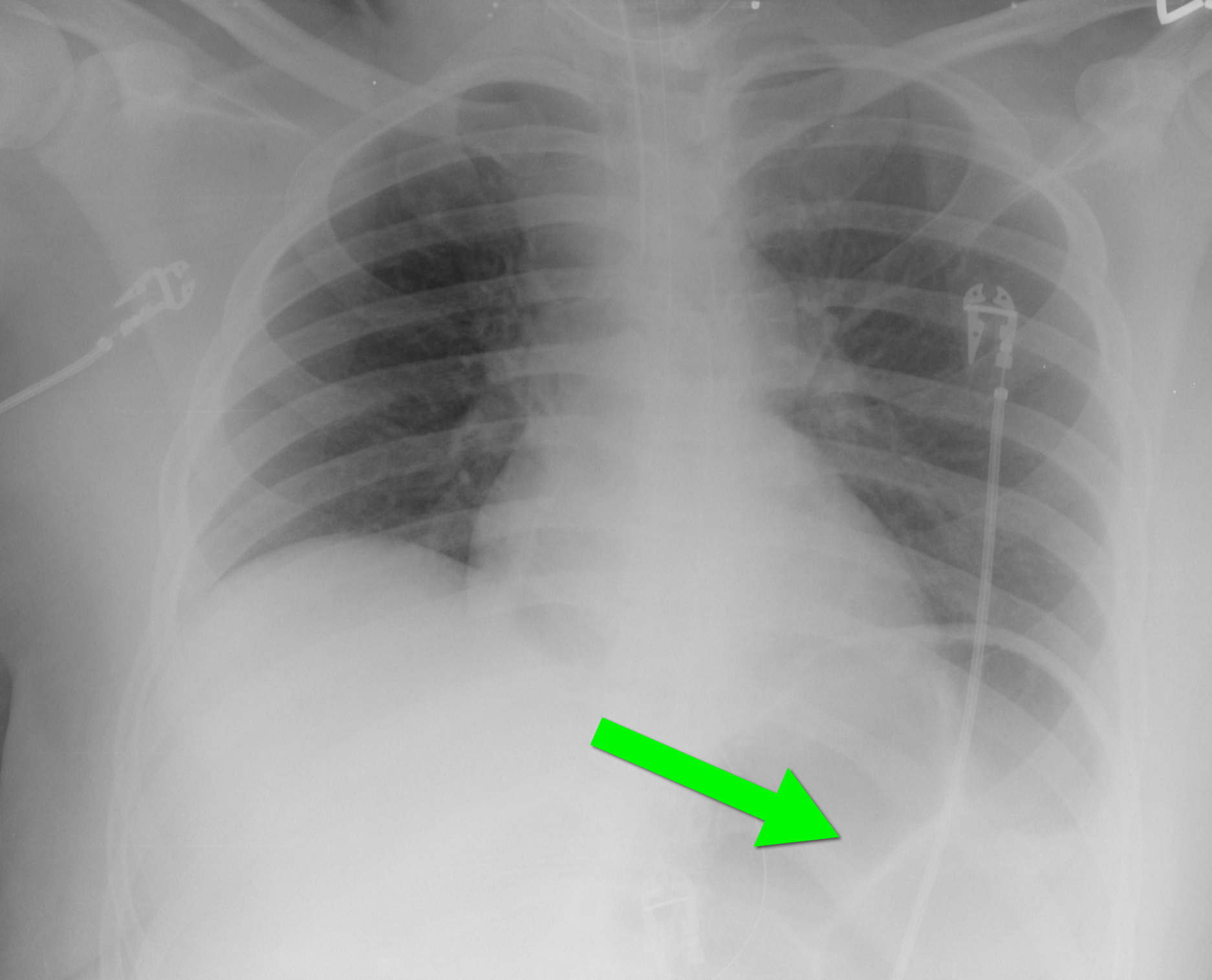
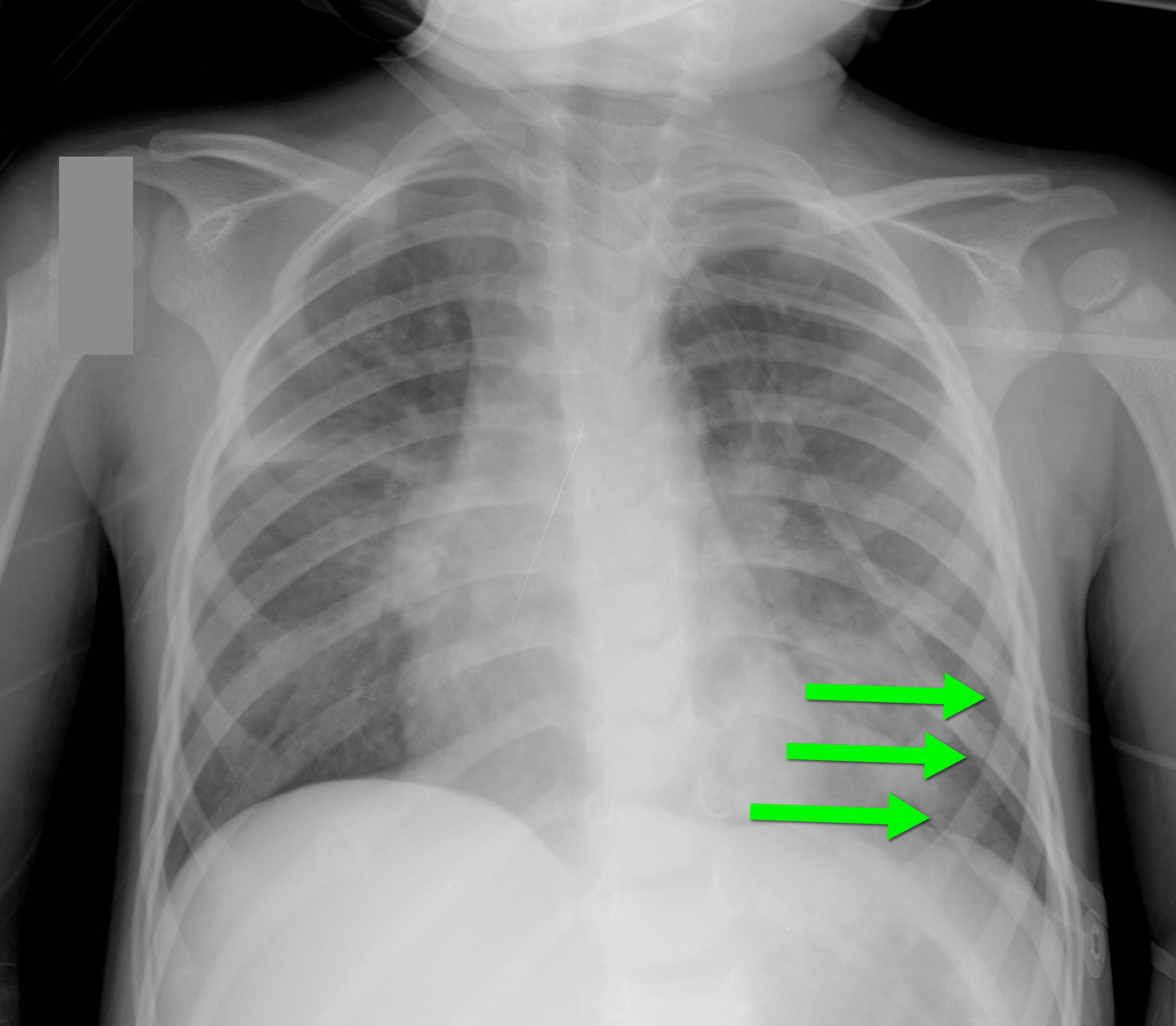
40 year-old female requiring intubation for altered mental status. CXR is below with something under the left diaphragm. What’s the diagnosis?
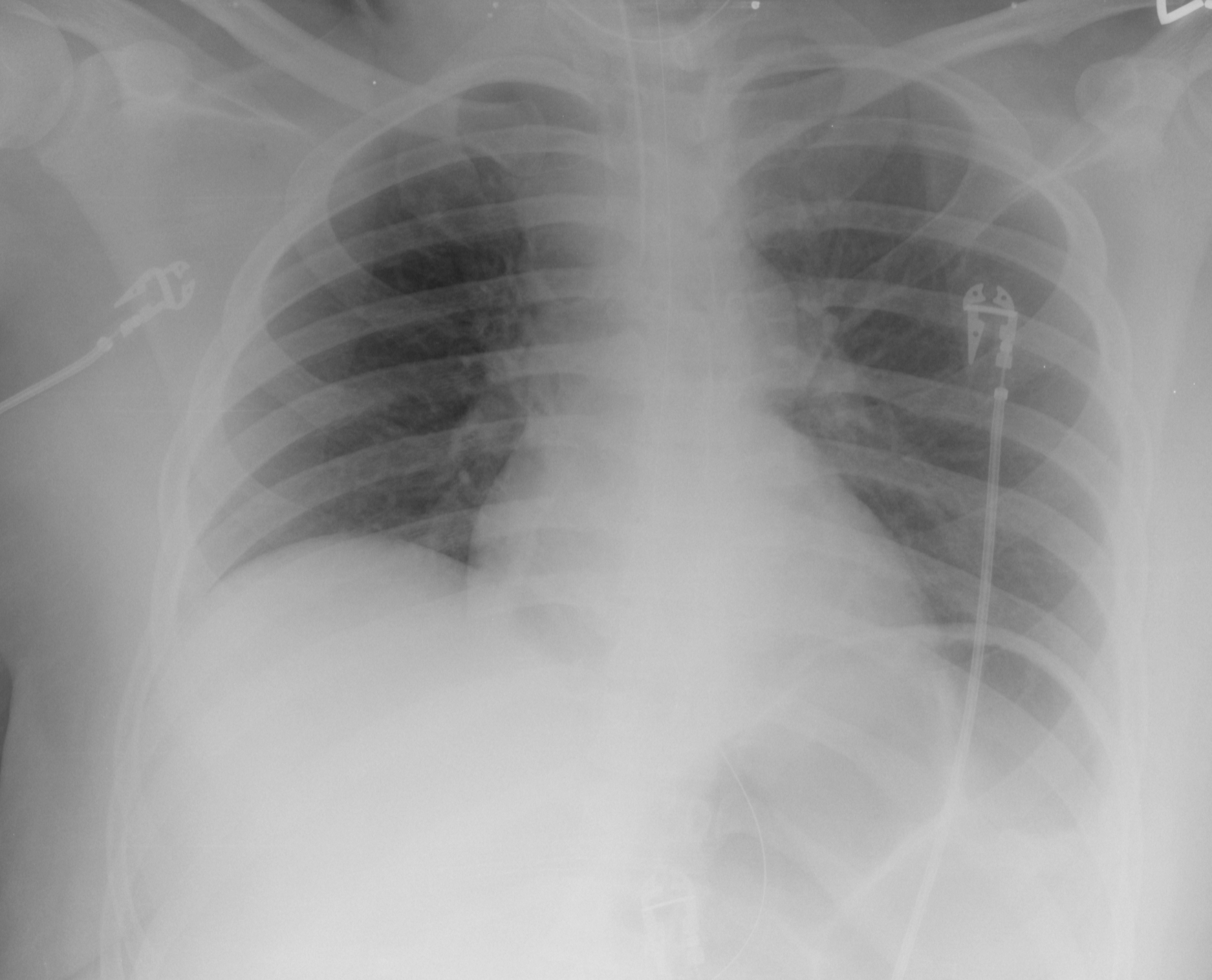
Answer: Loop of colon.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/4/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
65 year-old male with acute pulmonary edema. Ultrasound at the bedside shows this. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+(+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
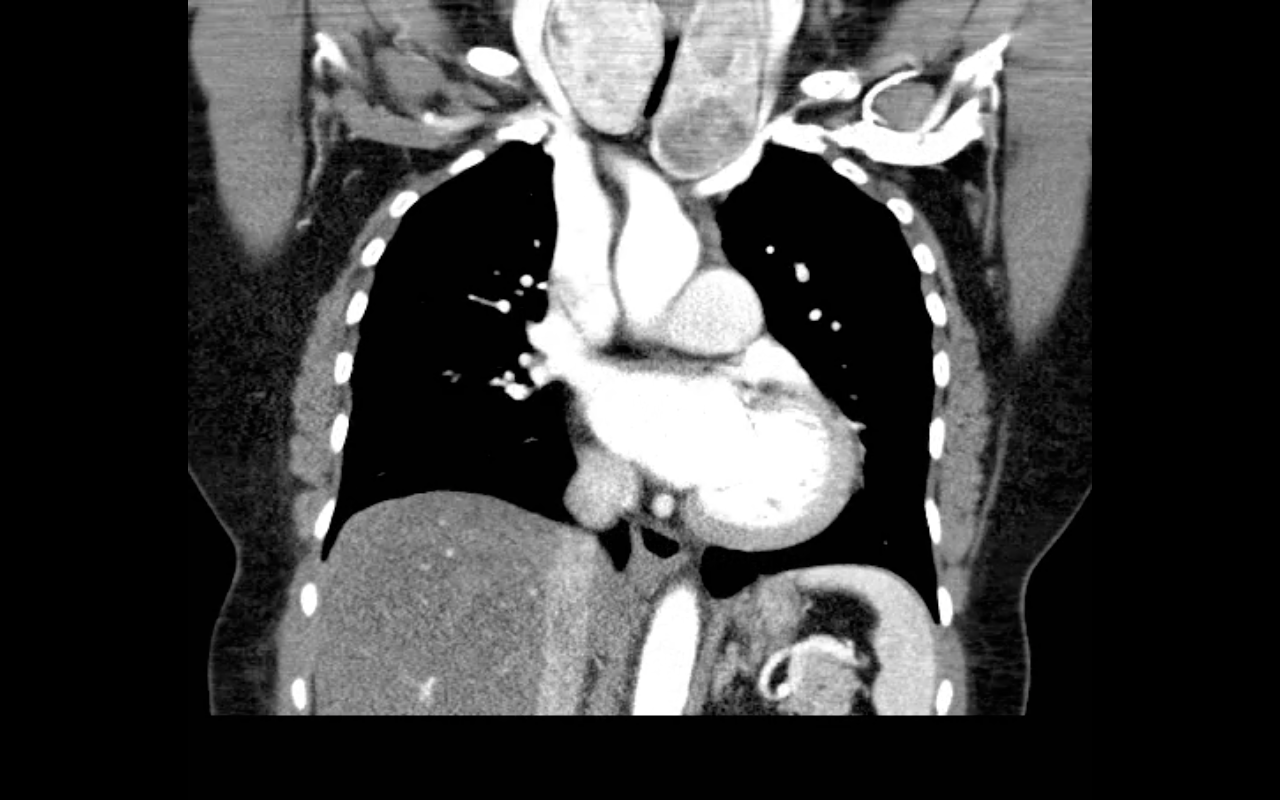
68 year-old female presents with stridor and palpable goiter. Here's a clip from CT of the chest. What's the diagnosis?
Category: Visual Diagnosis
Posted: 2/10/2013 by Haney Mallemat, MD
(Updated: 2/11/2013)
Click here to contact Haney Mallemat, MD
A 25 year-old female presents complaining of a "net-like" rash bilaterally on her medial thighs. She denies any pain but states that the rash looks “pretty scary” What's the diagnosis?

Answer: Erythema ab igne (a.k.a. "toasted-skin syndrome")
Erythema ab igne
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/4/2013 by Haney Mallemat, MD
(Updated: 3/20/2013)
Click here to contact Haney Mallemat, MD
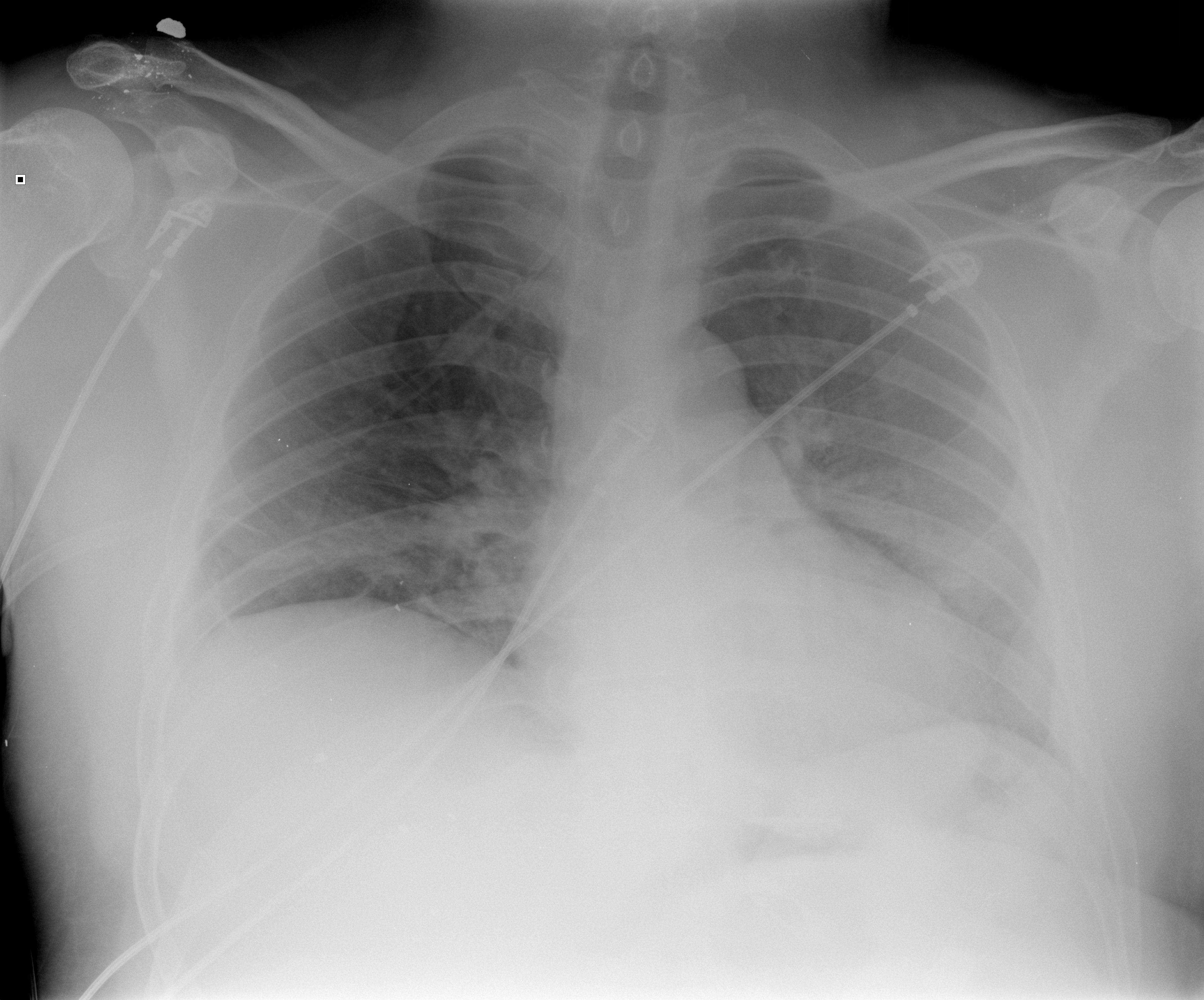
40 year-old male presents with fever, chills, & cough. What’s the diagnosis and the MOST likely cause?
Answer: Pneumatocele from MRSA pneumonia
Pneumatocele
Pneumatoceles are thin-walled, air-filled cysts with lung parenchyma; they may be solitary or multiple
Most commonly a sequellae to pneumonia secondary to Staphylococcus aureus (up to 85% of cases), although other etiologic agents have been found (Streptococcus pneumonia, E. coli, Klebsiella, Adenovirus and Tuberculosis). Non-infectious causes include trauma, hydrocarbon ingestion, and positive pressure ventilation.
Pneumatoceles are typically asymptomatic and require treatment of the inciting etiology (e.g., antibiotics for pneumonia), but complications may occur including tension pneumatocele, pneumothorax, and secondary infection of the pneumatocele.
Surgical resection is typically not needed but percutaneous catheter drainage may be required if the pneumatocele involves >50% of the hemithorax
Advise patients against exposure to high altitudes, skydiving and scuba diving until pneumatocele(s) resolve, to avoid progression to pneumothorax.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/28/2013 by Haney Mallemat, MD
(Updated: 1/29/2013)
Click here to contact Haney Mallemat, MD
40 year-old female drove into a ditch. Right sided chest pain and stable vitals. Here's the CT but what do you think the initial CXR showed (Hint: it's a trick)?
Here's the initial CXR. Click here for the video presentation.

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/21/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
45 year-old male complains of chest pain and cough. He also tells you, "...oh, and by the way doc, I just smoked something." What's the diagnosis?
Visual pearls is two years old!!! I want to take this time to thank you all for your support....and now, your answer.
Restrepo, C. et al. Pulmonary complications from cocaine and cocaine-based substances: imaging manifestations. Radiographics. Jul-Aug 2007; 27(4): 941-56
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Keywords: spinal, international, tuberculosis, scoliosis, kyphosis, pulmonary, neurologic (PubMed Search)
Posted: 1/9/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
These two Ethiopian boys present with “back problems”. What are the diagnoses and what do you need to worry about with each of them?
The boy on the left has spinal tuberculosis (Pott's Disease) while the one on the right has severe scoliosis.
Pott's Disease:
Severe Scoliosis:
Bottom Line:
Spinal tuberculosis most commonly causes anterioposterior (AP) deformity and can cause severe neurologic deficits. Anti-TB medication is needed for treatment.
Severe scoliosis involves lateral as well as AP deformity and can cause severe pulmonary dysfunction.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Center for Disease Control and Prevention. Guidelines for Preventing the Transmission of Mycobacerium tuberculosis in Health-Care Settings. MMWR 2005;54(No. RR-17):1-144.
Koumbourlis AC. Scoliosis and the respiratory System. Paediatric Respiratory Reviews 2006;7:152-160.
Turgut M. Spinal tuberculosis (Pott’s disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev 2001;24:8-13.
Category: Visual Diagnosis
Posted: 1/7/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
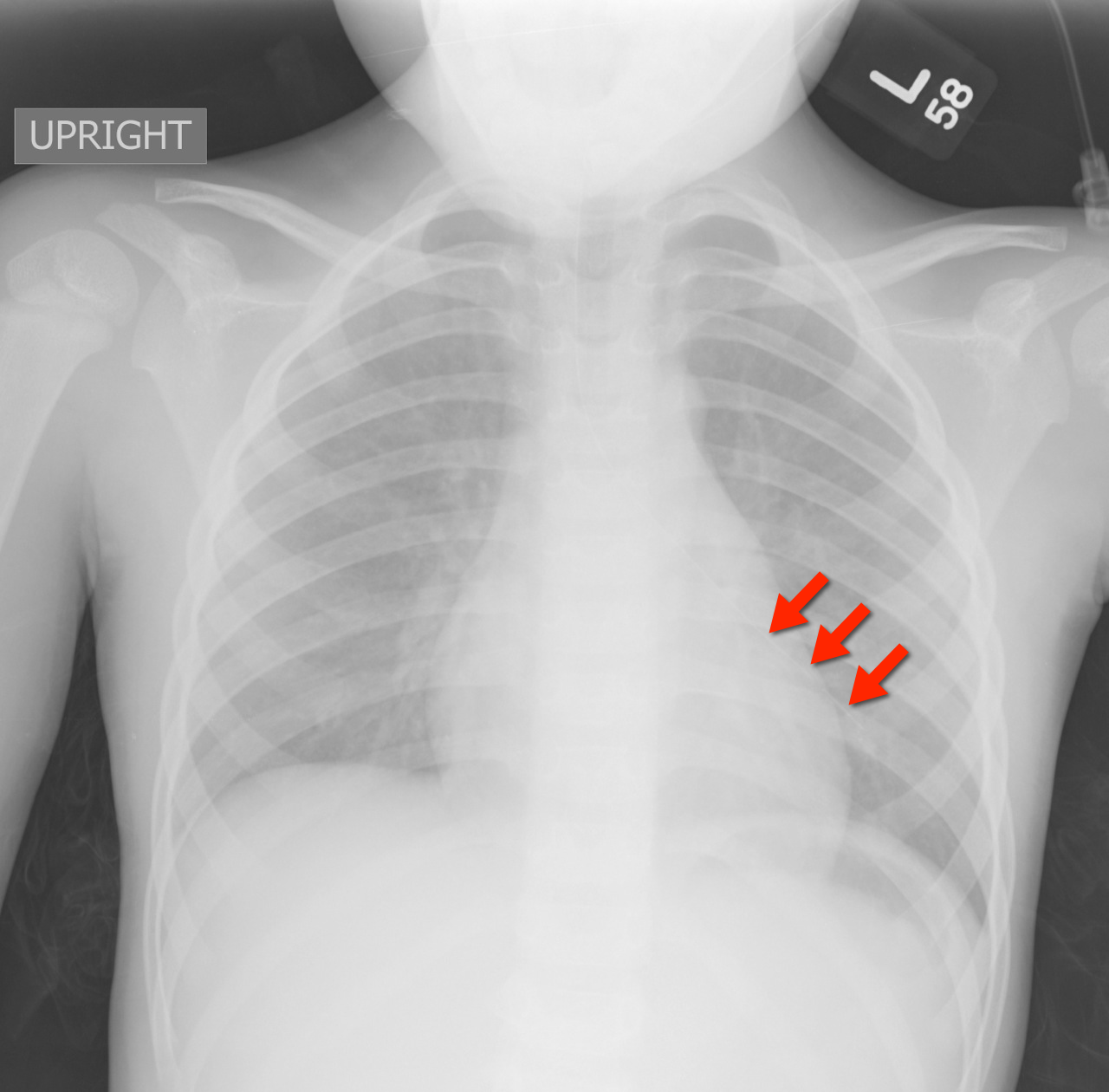
4 year-old female with the post-procedural CXR shown below. What's the diagnosis? (Hint: use the zoom...this one is tricky)
Answer: Nasogastric tube in the left mainstem bronchus. Patient was asymptomatic but ironically bubbling was heard when air was injected into the NG tube.
Nasogastric tube (NGT) pearls
The risk of NGT misplacement is 4% in adults, but is 21-43% in children.
Risk factors for misplacement are:
The ability to aspirate gastric contents, pH testing of the aspirated fluid, and the auscultation of “bubbling” over the epigastrium have all been suggested as reliable methods to confirm proper placement; unfortunately, they are often unreliable.
Visualization of the NGT by X-ray is the only way to be 100% certain of placement.
The risks of misplacement include pneumonia and pneumothorax.
Farrington et al. Nasogastric tube placement verification in pediatric and neonatal patients. Pediatric Nursing. Jan-Feb 2009. Vol 35. Issue 1.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/31/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
31 year-old male with recently diagnosed hypertension presents with rapid lip swelling. He started taking an unknown medication for his hypertension last week. Further history reveals that he has had prior, although milder, episodes previously. Name two medications that may help treat him.

Answer: The patient has hereditary angioedema with an episode triggered by an ACE inhibitor. Treatment includes the usual cocktail of histamine blockers and steroids plus:
The precipitant cause is unknown in most cases, but common etiologies include drugs (e.g. ACE inhibitors), infections, dental work, or stress.
Serum C4 level may assist in the diagnosis, but are rarely helpful acutely.
Fifty percent of patients will have laryngeal swelling at one point in their lives and asphyxiation is the leading cause of death; mortality is ~14-33%
The airway must be emergently evaluated to determine the need for intubation. If required, the most skilled person should take the first look.
If access to the oropharynx is limited (secondary to lip and tongue swelling) fiberoptic nasolaryngoscopy may be considered however, always be prepared to perform an emergent surgical airway.
Bonus Pearl: Check out this months V-Cast hosted by Dr. Amal Mattu. Dr. Jim Roberts (of Roberts and Hedges fame) reviews angioedema. Check out this great review here: http://cmedownload.com/lecture/angioedema-v-cast
References
Joseph J. Moellman, and Jonathan A. Bernstein. Diagnosis and Management of Hereditary Angioedema: An Emergency Medicine Perspective. Journal of Emergency Medicine 2012 http://www.jem-journal.com/article/S0736-4679(11)01116-4/abstract
Follow me on Twitter (@criticalcarenow) or on Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/24/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
52 year-old male with diabetes complains of severe left foot pain for one month and now inability to ambulate. Vital signs are normal and X-rays are shown below. What's the diagnosis and why should you get a biopsy early?

Answer: Osteomyelitis and a bone biopsy (with culture) should be obtained early and before starting antibiotics.
Osteomyelitis is inflammation of a bone secondary to an infecting organism.
Risk factors include:
Causative bacteria typically include S. Aureus, Pseudomonas, Salmonella (classically with Sickle cell)
Diagnosis
Early and long-term antibiotic treatment (4-6 weeks) is required, but should be done AFTER obtaining bone biopsy and culture; long-term antibiotics are the rule and the most narrow spectrum antibiotic should be determined.
Operative management is sometimes required; especially if secondary to infected prosthetics.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
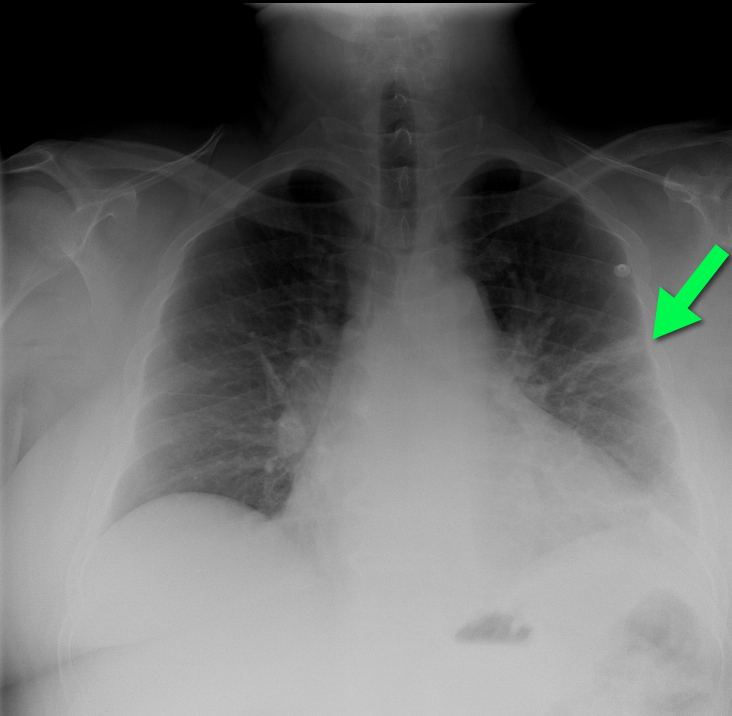
50 year-old man with presents with acute-onset sharp left-sided chest pain and dyspnea. What's the diagnosis and the name of the abnormality on chest x-ray?
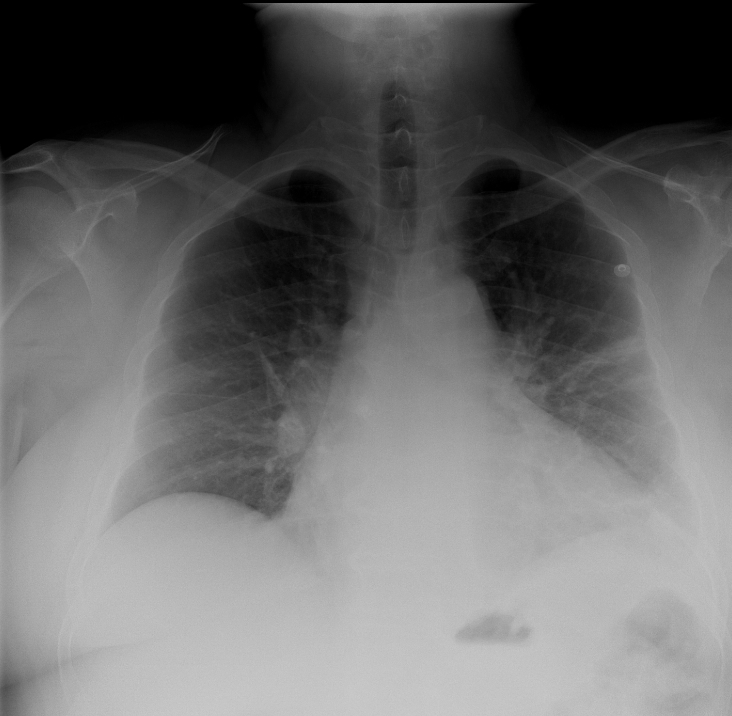
Answer: Pulmonary embolism with CXR demonstrating "Hampton Hump".
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/10/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
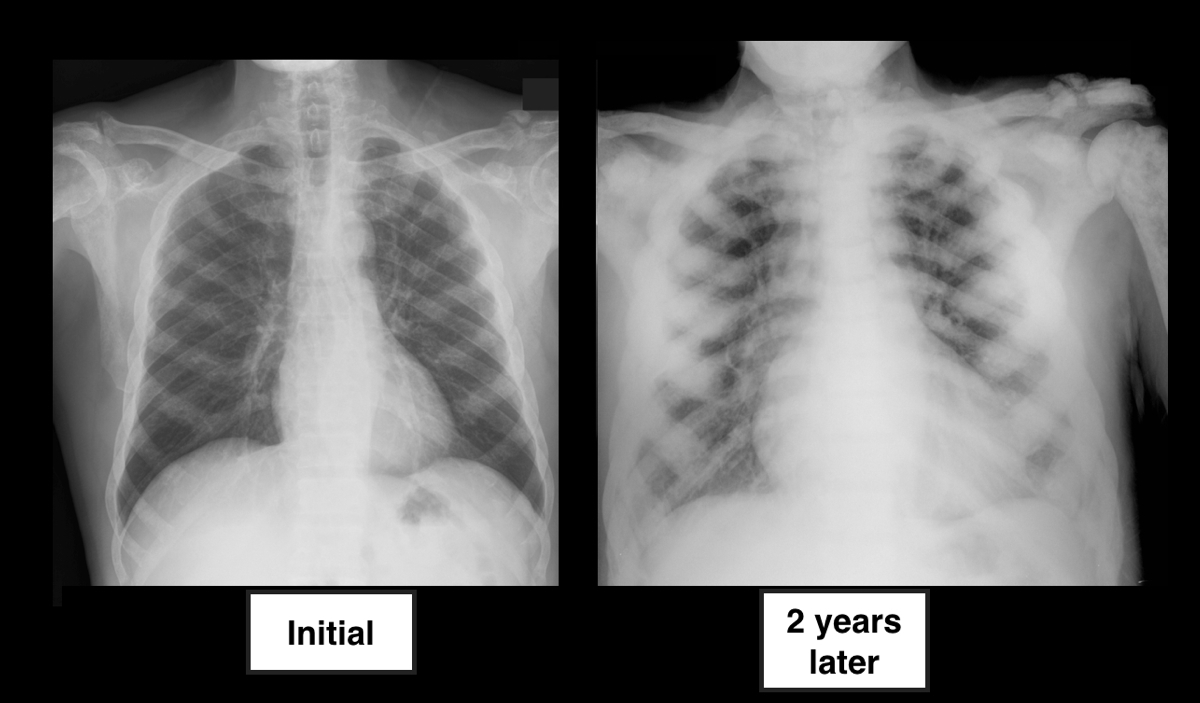
64 year-old male with no past medical history presents complaining of chronic weight-loss and diffuse chest pain; CXR is shown below. What's the diagnosis, and what other disease(s) may present this way?

Answer: Sclerotic bone (osteoblastic) metastasis secondary to prostate cancer. The patient's CXR from 2 years prior is shown below for comparison.
Other malignancies associated with osteoblastic metastasis:
Follow me on Twitter (@criticalcarenow) or on Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/4/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
An 86 year-old nursing home resident presents to the ED with a urinary tract infection, four days after discharge from the inpatient service for the same diagnosis. She was discharged from the inpatient service with a prescription for ciprofloxacin to be given through her gastric feeding tube (she does not take anything orally). Could her tube feeds be playing a role in the relapse of her urinary tract infection?
Answer: Ciprofloxacin was not being properly absorbed secondary to enteral tube feeding.
Fluoroquinolones administered via enteral feeding tubes may have reduced efficacy and patient outcomes when given to patients simultaneously receiving tube feeds (e.g., PEG tube feeding).
The reduction in antimicrobial efficacy may be due to improper peak drug concentrations and variability in time to peak serum levels. Studies have demonstrated the bioavailability of Ciprofloxacin varies from 31-82% in patients receiving continuous enteral feeds.
The exact mechanism(s) responsible for the altered pharmokinetics are not completely understood but may involve the binding of divalent cations in the enteral feeds by fluoroquinolones, reducing its absorption and efficacy.
Clinicians should properly educate people who will be administering fluoroquinolones to the patient (e.g., nursing home staff, family, etc.). It is recommended that fluoroquinolones be given:
Perhaps easiest of all, is to consider discharging patients with a prescription for parenterally administered antibiotics for the duration of the infection.
Beckwith MF, Feddema SS, Barton RG, Graves C. A guide to drug therapy in patients with enteral feeding tubes: Dosage form selection and administration methods. Hosp Pharm. 2004;39:225–37
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/2/2012 by Haney Mallemat, MD
(Updated: 12/3/2012)
Click here to contact Haney Mallemat, MD
11 year-old boy presents with right knee pain and swelling after falling off of his bicycle. What's the diagnosis?
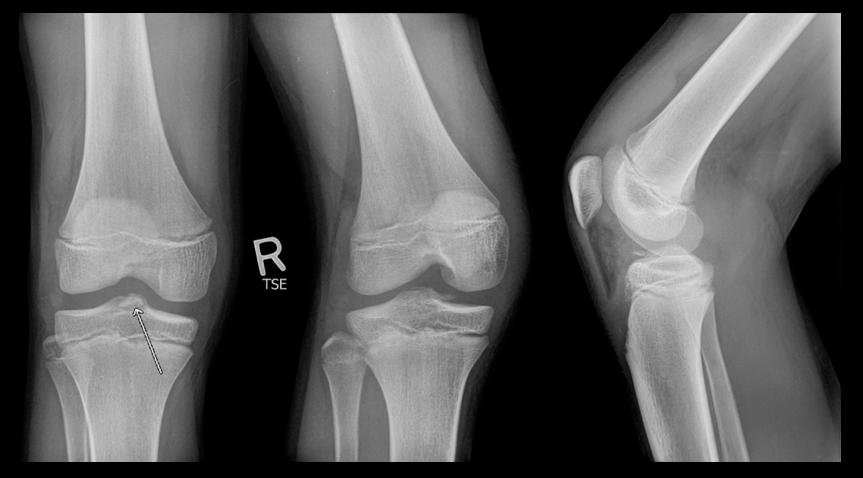
Answer: Fracture of the intercondylar eminence of the tibia; Meyers & McKeever Grade II (grading system described below)
Intercondylar Eminence Fracture
Reference: Tudisco, C., et al Intercondylar eminence avulsion fracture in children: long-term follow-up of 14 cases at the end of skeletal growth, J Pediatr Orthop B 19:403–408 c 2010
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/25/2012 by Haney Mallemat, MD
(Updated: 11/26/2012)
Click here to contact Haney Mallemat, MD
2 year-old male with past medical history of asthma presents with fever and respiratory distress. CXR is shown below. What’s the diagnosis? (Hint: ...look beyond the obvious)

Answer #1: Multifocal opacities predominantly in left lower lobe representing pneumonia
Answer #2 Healing left-sided rib fractures involving the lateral aspects of ribs 8 through 10th suspicious for non-accidental trauma (see X-ray below)
Pediatric CXR pearls
Bottom line: Screen patients for the above risk factors when rib fractures have been identified, but always think of abuse and the child’s safety first….and don’t forget to thoroughly examine radiology despite finding one abnormal finding.
Reference: Cosway et al. Diagnostic indicators for NAI in children with rib fractures: A retrospective study. Arch Dis Child 2011; 96 (supplement)
Follow me on Twitter (@criticalcarenow) or Google+ (+Haney Mallemat)
Category: Visual Diagnosis
Posted: 11/19/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Do you like placing ultrasound-guided IV catheters? Check out this trick for covering the probe during the procedure.
http://ultrarounds.com/Ultrarounds/The_Vascular_Probe_Protector.html
or
https://www.youtube.com/watch?v=ZuOq6Ea_FbA&feature=plcp
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/12/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
33 year-old male found unconscious by EMS and complains of right shoulder pain upon waking up in the ED. Diagnosis?
Answer: Posterior shoulder dislocation
Follow me on Twitter (@criticalcarenow) or Google+ (+Haney Mallemat)
