Category: Visual Diagnosis
Posted: 6/10/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
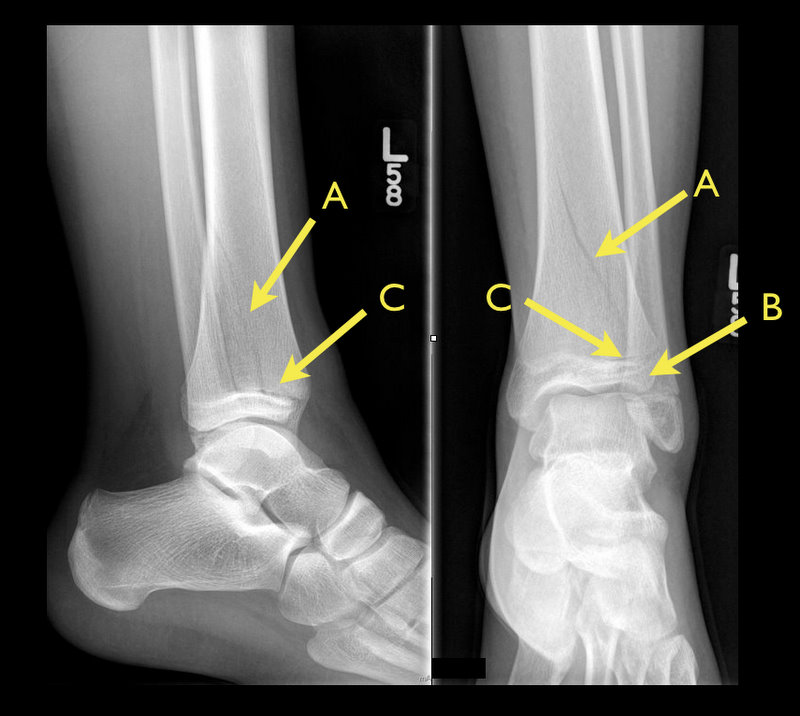
13 year-old female with ankle pain following fall down escalator. What's the diagnosis?

Answer: Tri-plane ankle fracture
Tri-plane Fractures

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 6/4/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Therapeutic hypothermia (TH) following out-of-hospital cardiac arrest (OHCA) has increasingly been utilized since it was first described. TH following in-hospital cardiac arrest (IHCA), on the other hand, is not as commonplace or consistent despite a recommendation by the American Heart Association (AHA).
A recent prospective multi-center cohort-study demonstrated that of 67,498 patients with return of spontaneous circulation (ROSC) following IHCA only 2.0% of patients had TH initiated; of those 44.3% did not even achieve the target temperature (32-34 Celsius).
The factors found to be most associated with instituting TH were:
Bottom-line: Hospitals should consider instituting and adhering to local TH protocols for in-house cardiac arrests.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/3/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Ever wonder how to place a pigtail catheter?
Check out this video to learn how, click here
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 5/27/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
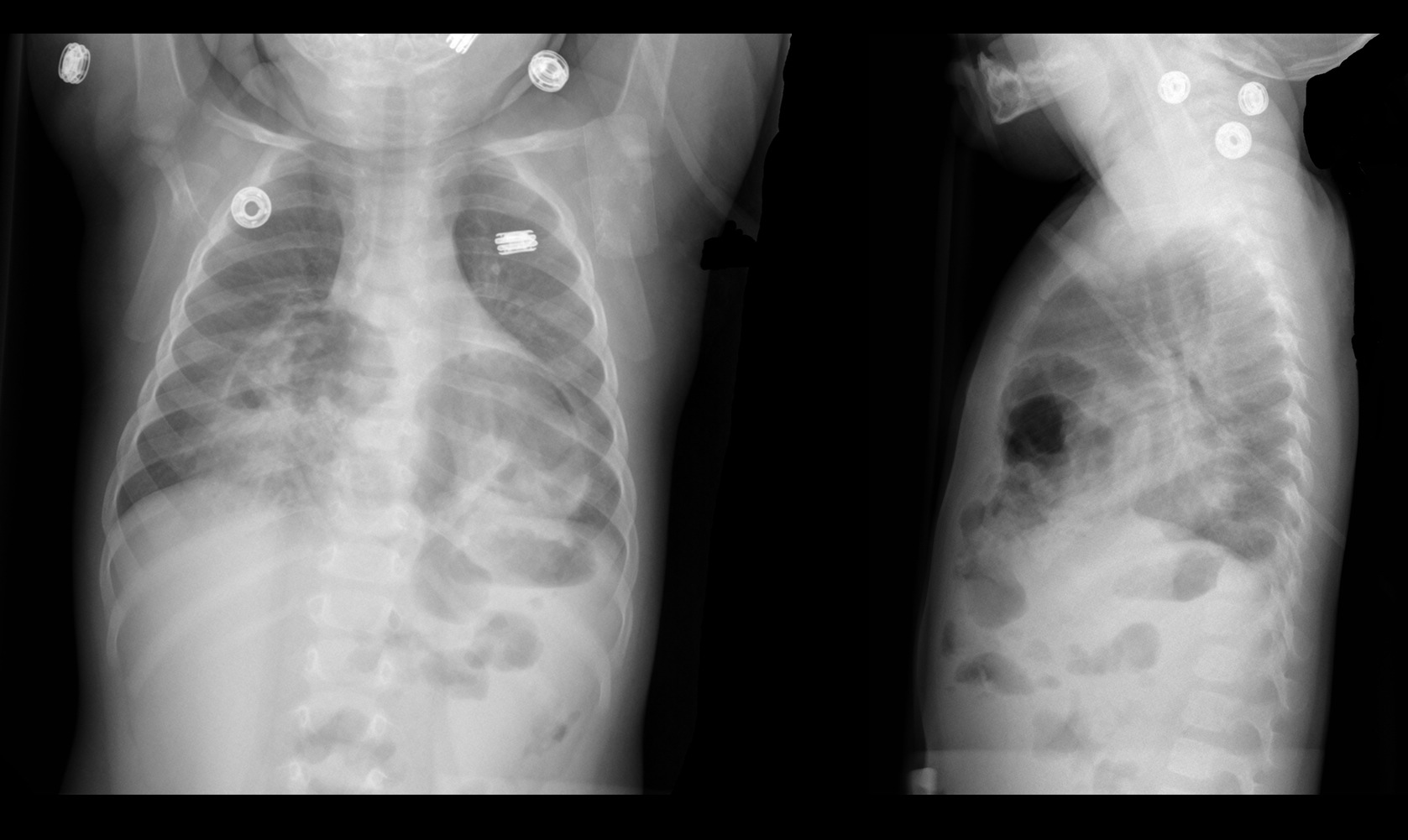
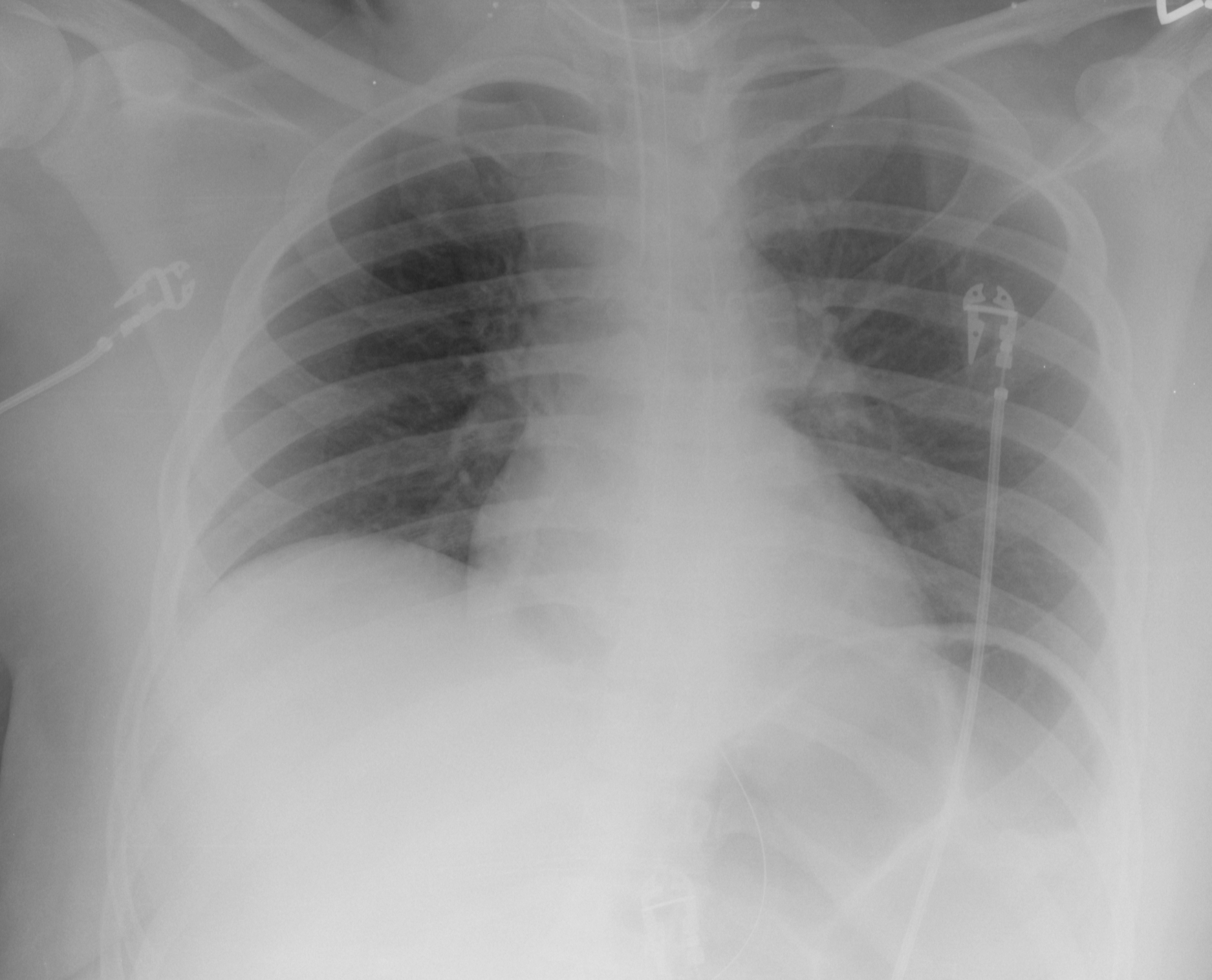
9 month-old presents with wheezing and the CXR is shown below. What's the diagnosis?
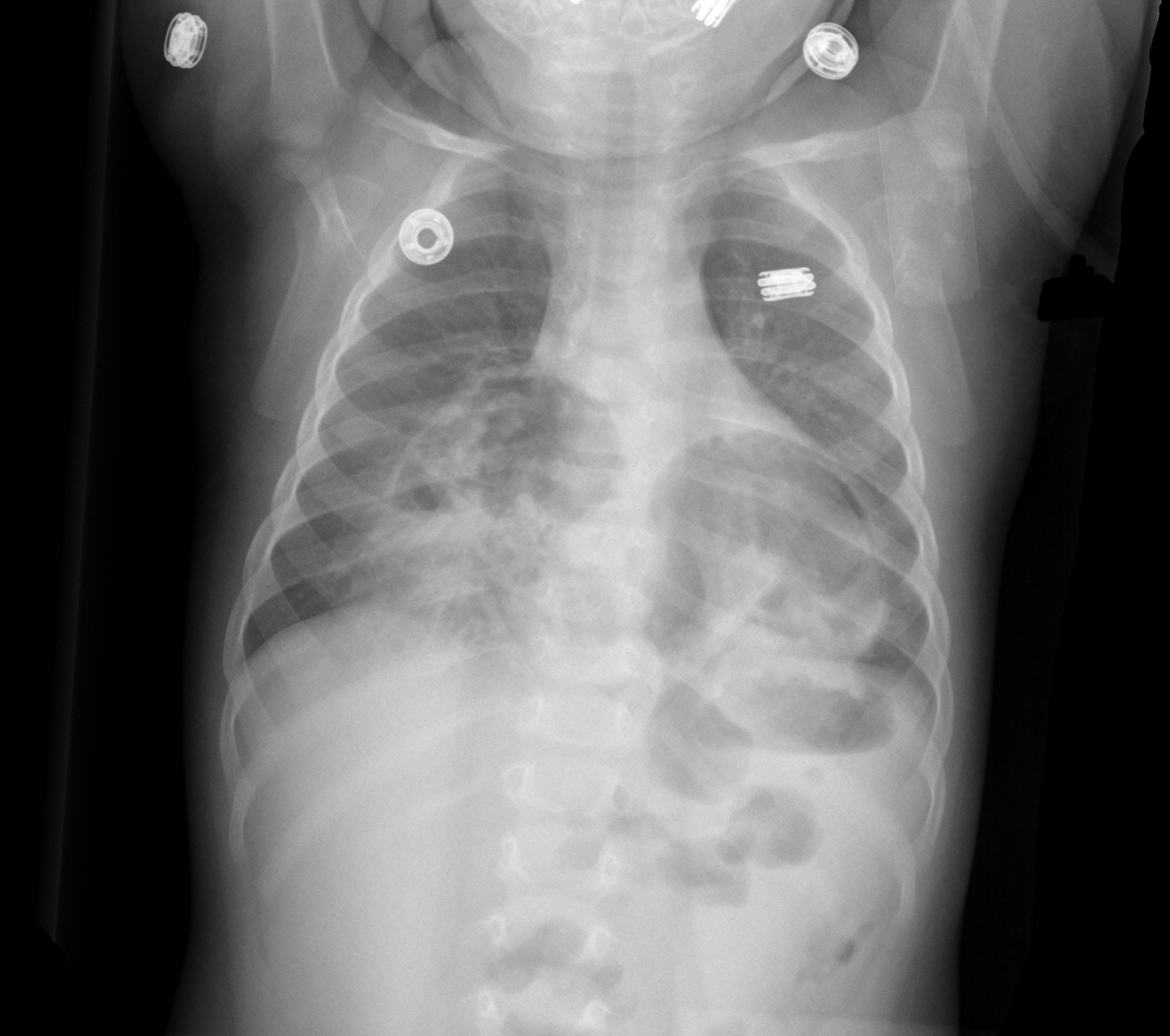
Congenital anterior diaphragmatic defects with herniated bowel.
Follow me on Twiter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 5/21/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The Macklin Effect
Pneumomediastinum (click here for image) may be caused by many things:
The "Macklin Effect" is typically a self-limiting condition leading to spontaneous pneumomediastinum and massive subcutaneous emphysema after the following:
Pneumomediastinum secondary to the Macklin effect frequently leads to an extensive workup to search for other causes of mediastinal air. Although, no consensus exists regarding the appropriate workup, the patient's history should guide the workup to avoid unnecessary imaging, needless dietary restriction, unjustified antibiotic administration, and prolonged hospitalization.
Treatment of spontaneous pneumomediastinum includes:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 5/20/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
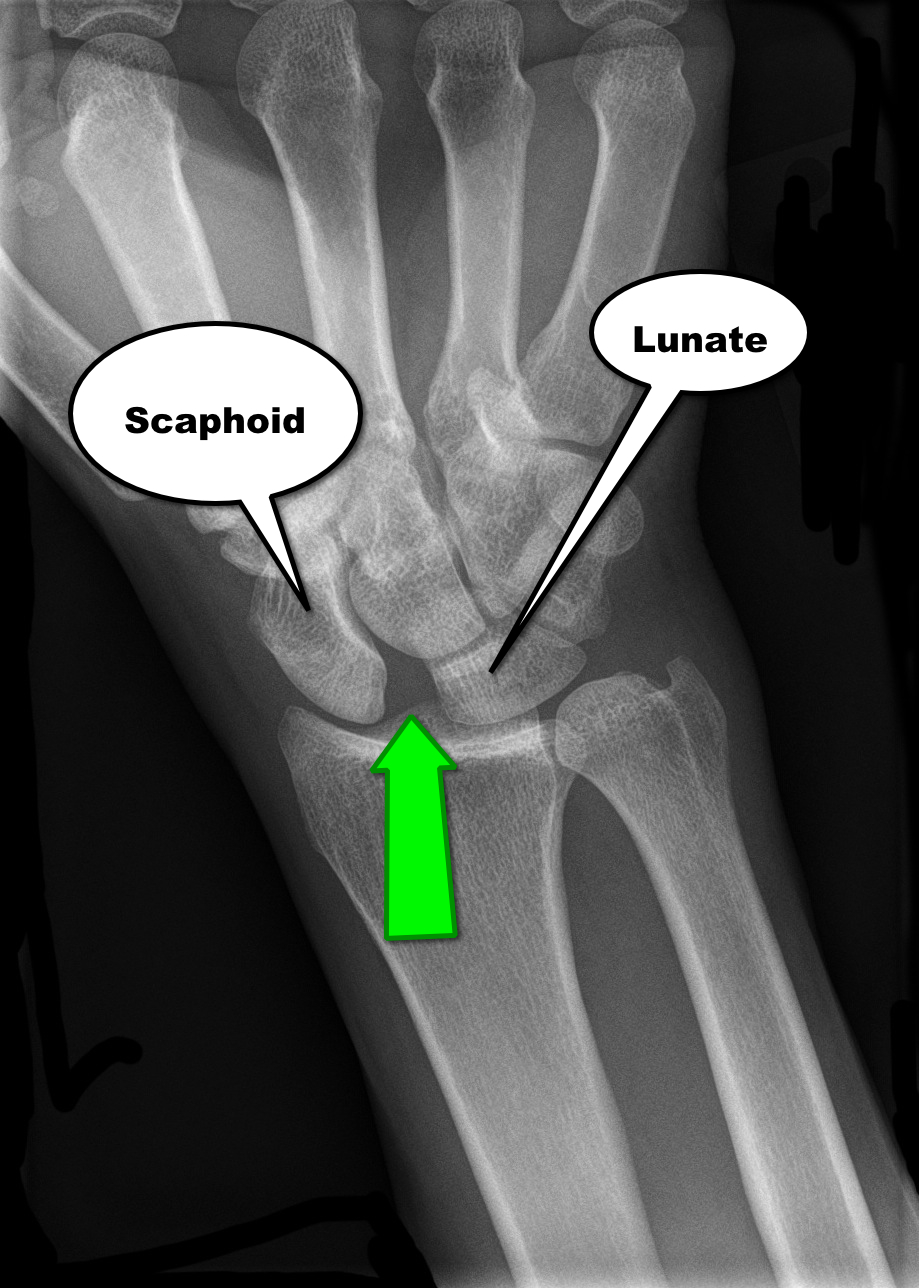
30 year-old male presents with right wrist pain after falling off his bicycle. What's the diagnosis?
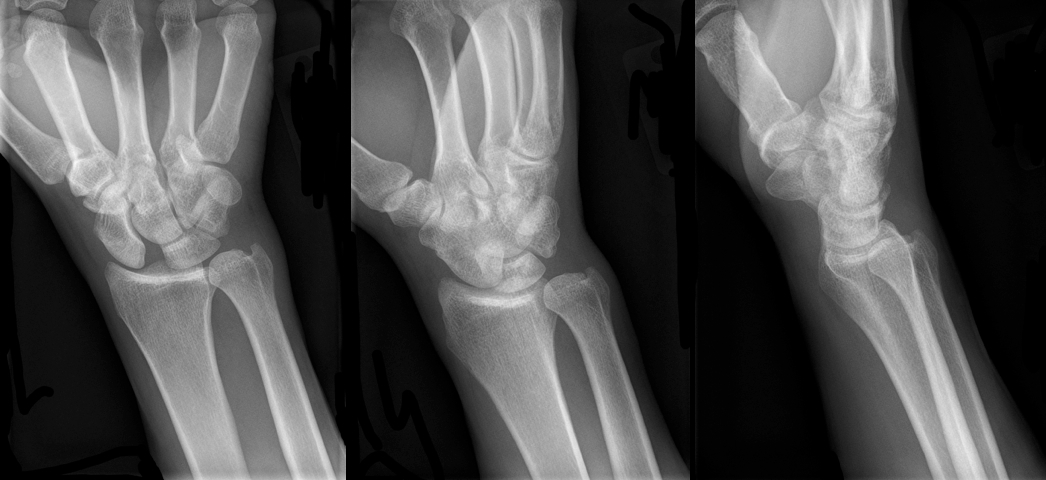
Scapholunate dislocation
Scapholunate Dislocation (a.k.a. “Terry Thomas” or “David Letterman” sign)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 5/13/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
60 year-old male with a history of pulmonary fibrosis presents to the Emergency Department after a lung biopsy. He is complaining of facial swelling and dyspnea. What's the diagnosis?

Answer: Massive subcutaneous emphysema
Click here
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 5/7/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Fluid boluses are often administered to patients in shock as a first-line intervention to increase cardiac output. Previous literature states, however, that only 50% of patients in shock will respond to a fluid bolus.
Several validated techniques exist to distinguish which patients will respond to a fluid bolus and which will not; one method is the passive leg raise (PLR) maneuver (more on PLR here). A drawback to PLR is that it requires direct measurement of cardiac output, either by invasive hemodynamic monitoring or using advanced bedside ultrasound techniques.
Another technique to quantify changes in cardiac output is through measurement of end-tidal CO2 (ETCO2). The benefits of measuring ETCO2 is that it can be continuously measured and can be performed non-invasively on mechanically ventilated patients.
A 5% or greater increase in end-tidal CO2 (ETCO2) following a PLR maneuver has been found to be a good predictor of fluid responsiveness with reliability similar to invasive measures.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 5/5/2013 by Haney Mallemat, MD
(Updated: 5/6/2013)
Click here to contact Haney Mallemat, MD
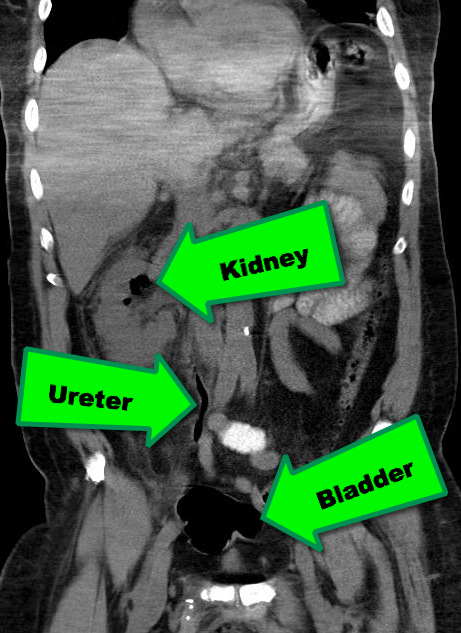
38 year-old male with a past medical history of diabetes presents with back pain and hypotension. CT scan is shown below. What's the diagnosis?
Emphysematous Pyelonephritis (EPN)
EPN is a necrotizing infection of the renal and peri-nephric tissues with accumulation of gas within the tissues and collecting system of the kidney; it is rapidly fatal if not recognized and aggressively treated early.
Risk factors include an immunocompromised host; Diabetics are at particularly increased risk.
The most common etiologic organisms are Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, and Pseudomonas aeruginosa. Infection with anaerobic species is relatively uncommon.
In addition to the classic signs / symptoms of pyelonephritis, (e.g., flank pain, fever, pyuria, etc.), patients presenting with EPN may experience the passage of air in the urine (pneumaturia) or crepitus over their flank.
Abdominal CT scan is the diagnostic test of choice when clinical presentation and laboratory tests are suggestive (see below)
Treatment should include:
Follow me on Twitter (@criticalcarenow) or Google+(criticalcarenow)
Category: Visual Diagnosis
Posted: 4/29/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
57 year old male presents with a cough. The CXR is shown below. What's the diagnosis?
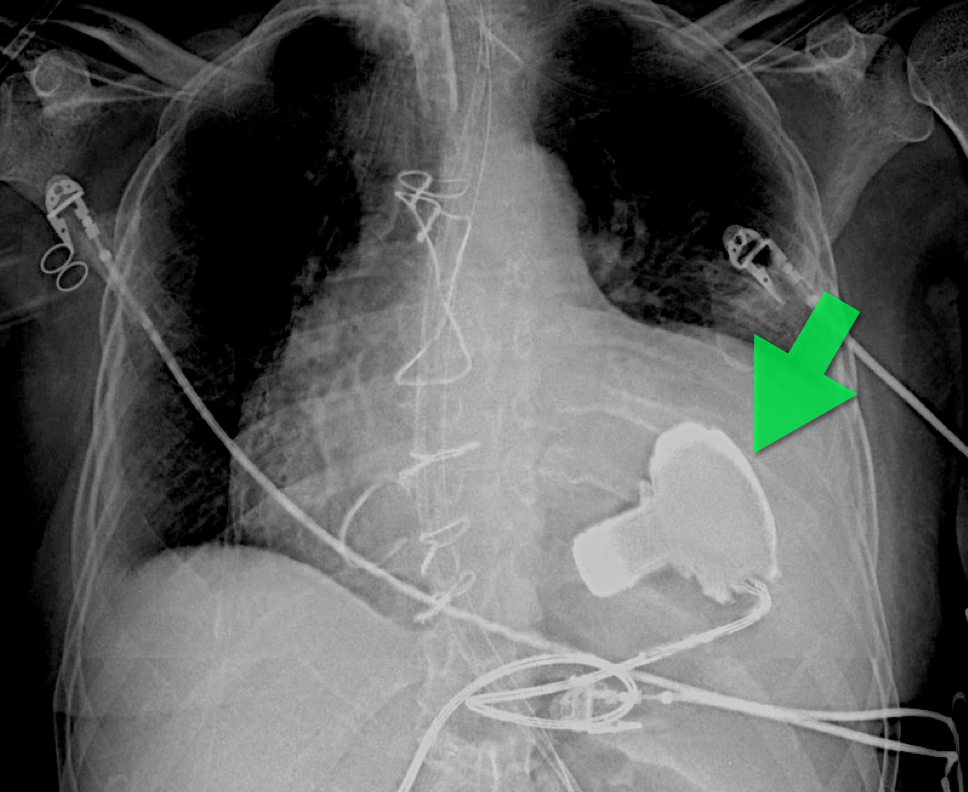
Answer: Left Ventricular Assist Device (LVAD)
An LVAD is a mechanical pump that pulls blood from the left ventricle and pumps it to the ascending aorta for systemic delivery; LVADs are increasingly being placed in patients with heart failure so you must be aware of them.
The three indications for an LVAD are:
There are several models, which have been implanted in people (http://www.mylvad.com/lvad-devices). The main distinction between devices are pulsatile or non-pulsatile (or linear) flow; newer generation devices are non-pulsatile.
Patients with LVAD may develop complications such as infections, arrhythmias, or anemia, but bleeding can be a life-threatening one; bleeding occurs secondary to an acquired von Willebrand factor deficiency, AVMs within the GI tract, or secondary to over anti-coagulation (typically with Warfarin).
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 4/23/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Necrotizing fasciitis (NF) is a rapidly progressive bacterial infection of the fascia with secondary necrosis of the subcutaneous tissue. In severe cases, the underlying muscle (i.e., myositis) may be affected.
Risk factors for NF include immunosuppression (e.g., transplant patients), HIV/AIDS, diabetes, etc.
There are three categories of NF:
In the early stage of disease, diagnosis may be difficult; the physical exam sometimes does not reflect the severity of disease. Labs may be non-specific, but CT or MRI is important to diagnose and define the extent of the disease when planning surgical debridement.
Treatment should be aggressive and started as soon as the disease is suspected; this includes:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 4/15/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
35 year-old female presents with fever and hypotension. Bedside ultrasound is performed and is shown here. What's the diagnosis?
Answer: Aortic valve vegetation secondary to infective endocarditis.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 4/8/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
64 year-old female presents with chest pain following an argument with her husband. Her echocardiogram (apical four-chamber view) and ECG are shown. Her initial troponin is 10. What's the diagnosis?
Answer: Takotsubo (a.k.a Stress) cardiomyopathy (TC)
TC is left ventricular dysfunction (hypokinesia, akinesia, or dyskinesia) secondary to catecholamine surge (e.g., physical / emotional stress) causing myocardial stunning; it is not due to acute coronary occlusion. TC disproportionately affects postmenopausal women, occurring in up to 90% of cases.
Patients often present with chest pain or dyspnea; 85% of patients will have an abnormal ECG (e.g., ST elevation or T wave inversions), making diagnosis difficult to differentiate between TC and acute coronary syndrome (ACS). TC has been found to be the diagnosis in 2.5% of patients initially worked up for ACS.
Diagnosis can usually be confirmed with echocardiography but cardiac catheterization (with ventriculogram) is sometimes performed if ACS is strongly suspected. Catheterization demonstrates normal coronary arteries with an abnormal ventriculogram (click for video), typically in mid-to apical portion of the left ventricle.
Treatment is symptomatic and similar to congestive heart failure (e.g., diuretics, beta-blockers, etc.); 95% of patients have full recovery within one month.
Refer to this prior PEARL by Dr. Tewelde for additional information
Reference
T Pilgrima, T Wyss, Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: A systematic review, Int J Card 2008 Mar 14;124(3):283-92
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 4/1/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
What's the Diagnosis?

Answer: Normal CXR...April Fool's Day ;)
Our international friends can learn more about April Fool'sDay here
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 3/26/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
There are several reasons why a mechanically ventilated patient may decompensate post-intubation. Immediate action is often needed to reverse the problem, but it can be difficult to remember where to start as the vent alarm is sounding and the patient is decompensating.
Consider using the mnemonic “D.O.P.E.S. like D.O.T.T.S.” to assist you in first diagnosing the problem (D.O.P.E.S.) and then fixing the problem (D.O.T.T.S.). You can view an entire lecture on the Crashing Ventilated Patient here.
Step 1: Could this decompensation be secondary to D.O.P.E.S.?
Step 2: Fix the problem with D.O.T.T.S.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/25/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
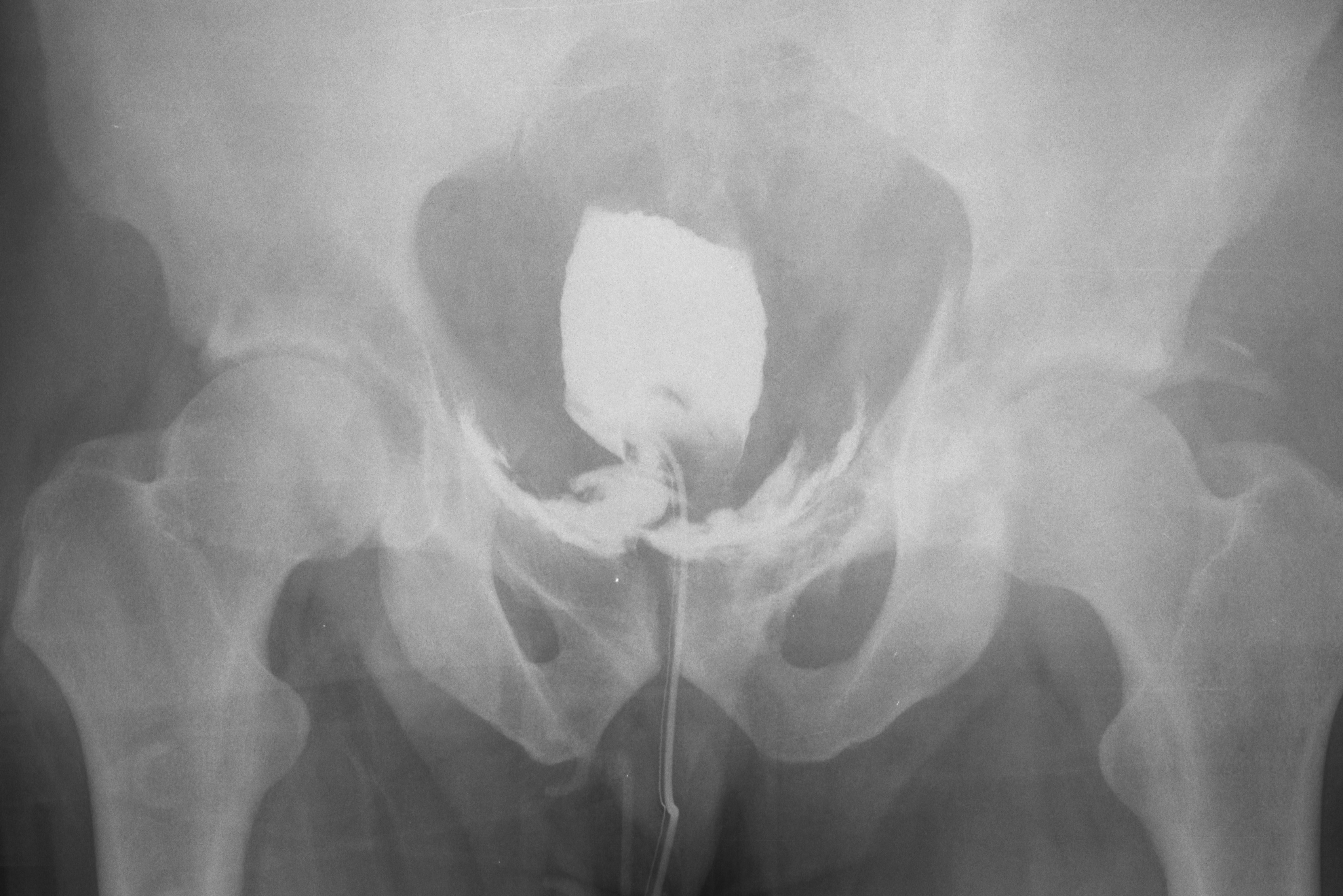
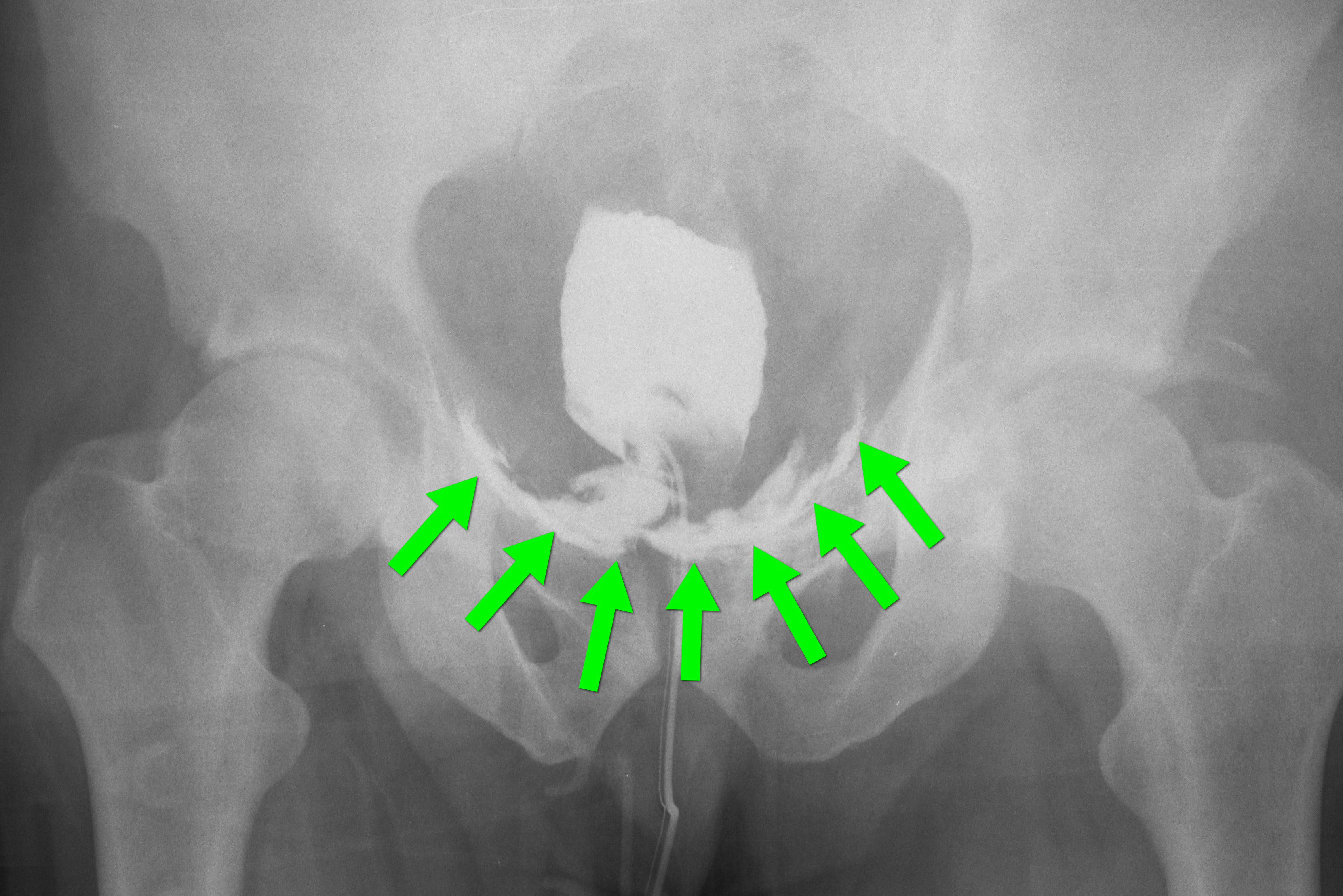
35 year-old male presents after a motor vehicle crash. No blood seen at the meatus of the penis and a Foley catheter is placed (see photo below). What's the next diagnostic step?

Answer: Retrograde cystogram
Traumatic bladder rupture
Gross or microscopic hematuria (>50 RBCs per high-power field) following blunt trauma requires a retrograde cystogram to evaluate for bladder injury. If blood is present at the meatus, however, urethral injury (not discussed) should be suspected and retrograde urethrogram should be performed before passing a Foley catheter.
A retrograde cystogram is performed by infusing diluted contrast into the bladder (200-400 mL) to gently distend the bladder and allow visualization of potential rupture(s). A CT scan of the abdomen and pelvis is then performed to determine if any contrast has leaked from the bladder; alternatively an AP pelvis can also be used, but is not as sensitive as CT.
Traumatic bladder ruptures are categorized as either intra-peritoneal or extra-peritoneal (note: X-ray below demonstrates extra-peritoneal rupture).
Treatment for bladder rupture:
Prognosis is typically good for either injury.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A 56-year-old woman with a history of psoriasis presents with fever, nausea, and painful pin-point pustules on an erythematous base. Her dermatologist recently reduced her prednisone dose. What's the diagnosis?

Answer: Pustular psoriasis
Pustular psoriasis
Occurs in patients with psoriasis, classically occurring after a decrease in dose or cessation of systemic steroids
Symptoms include:
These lesions can eventually drain and desquamate, leaving large patches of exposed dermis.
Complications include:
Patients may be admitted for supportive care and treatment with disease-modifying antirheumatic drugs (DMARDs) such as cyclophosphamide or methotrexate.
REFERENCE
L Naldi, D Gambini, The clinical spectrum of psoriasis, Clinics in Dermatology, Volume 25, Issue 6, November–December 2007, Pages 510-518
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 3/12/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Mechanically ventilated patients can develop a condition in which air becomes trapped within the alveoli at end-expiration; this is called auto-PEEP.
Auto-peep has several adverse effects:
Auto-PEEP classically occurs in intubated patients with asthma or emphysema, but it may also occur in the absence of such disease. The risk of auto-PEEP is increased in patients with:
Auto-PEEP may be treated by:
Patients may need to be heavily sedated to accomplish the above ventilator maneuvers.
Follow me on Twtitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/11/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
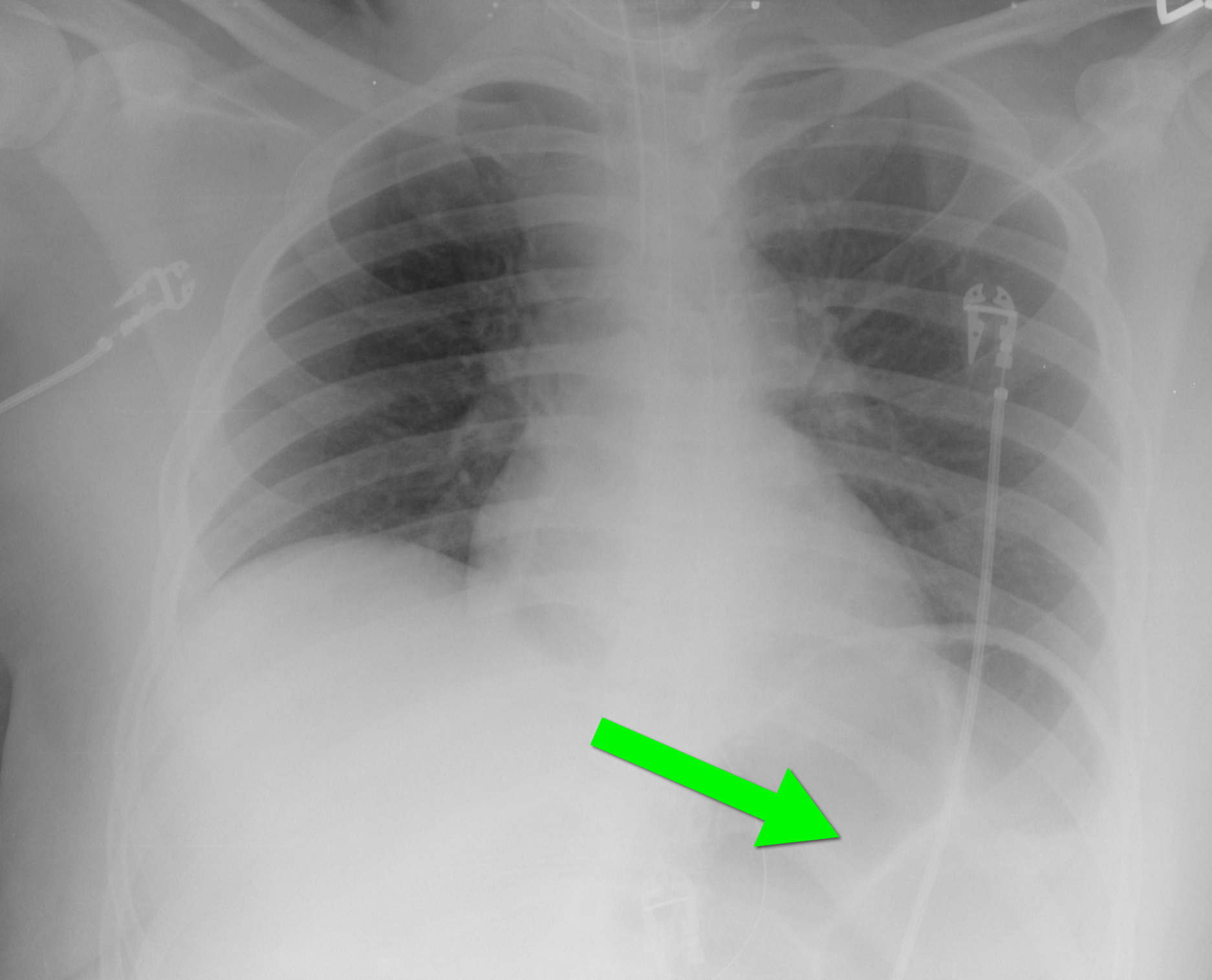
40 year-old female requiring intubation for altered mental status. CXR is below with something under the left diaphragm. What’s the diagnosis?
Answer: Loop of colon.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/4/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
65 year-old male with acute pulmonary edema. Ultrasound at the bedside shows this. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+(+criticalcarenow)
