Category: Visual Diagnosis
Posted: 9/8/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
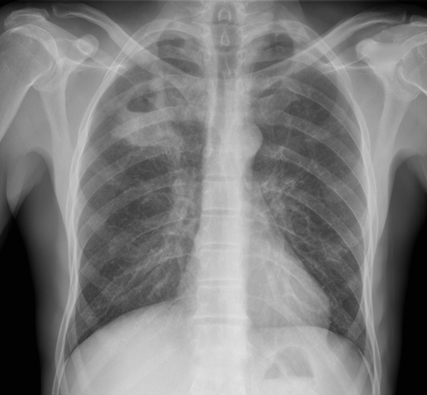
CXR shown below, what's the diagnosis? ...and name 3 differential diagnoses.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 9/2/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
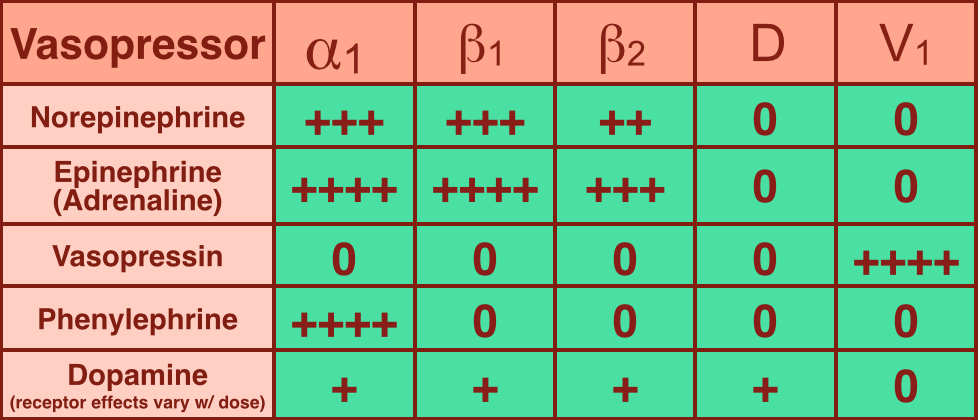
Vasopressors are used in shock-states to increase mean arterial pressure (MAP) and improve distal tissue perfusion. Additionally, some agents have effects on the heart to augment cardiac output.
Receptors that vasopressors work on include:
Norepinephrine (NE): excellent vasopressor for most types of shock and recommended as a first-line agent in the Surviving Sepsis Guidelines.
Epinephrine (a.k.a. Adrenaline): in several countries the first-line agent for shock (including sepsis).
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 9/1/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
You are scaning the liver with ultrasound and you see this. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 8/25/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
50 year-old female with diabetes complains of pain and discharge from a poorly healing wound. XRay below. What's the diagnosis?

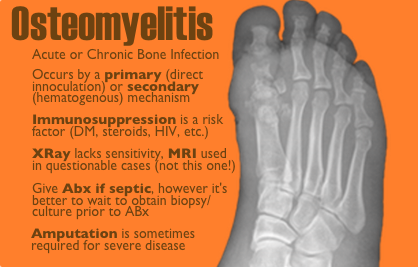
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 8/18/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A critically-ill patient requires fluid resuscitation. Someone hands you a bag of this. What’s the pH of this fluid?
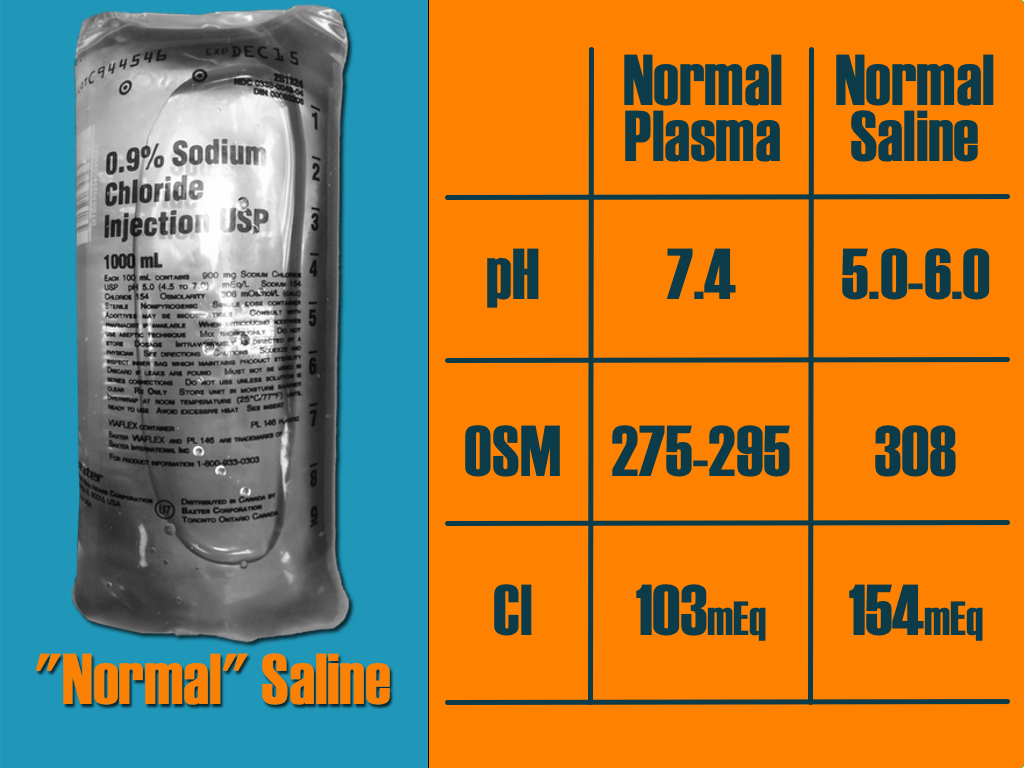
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 8/11/2014 by Haney Mallemat, MD
(Updated: 8/12/2014)
Click here to contact Haney Mallemat, MD
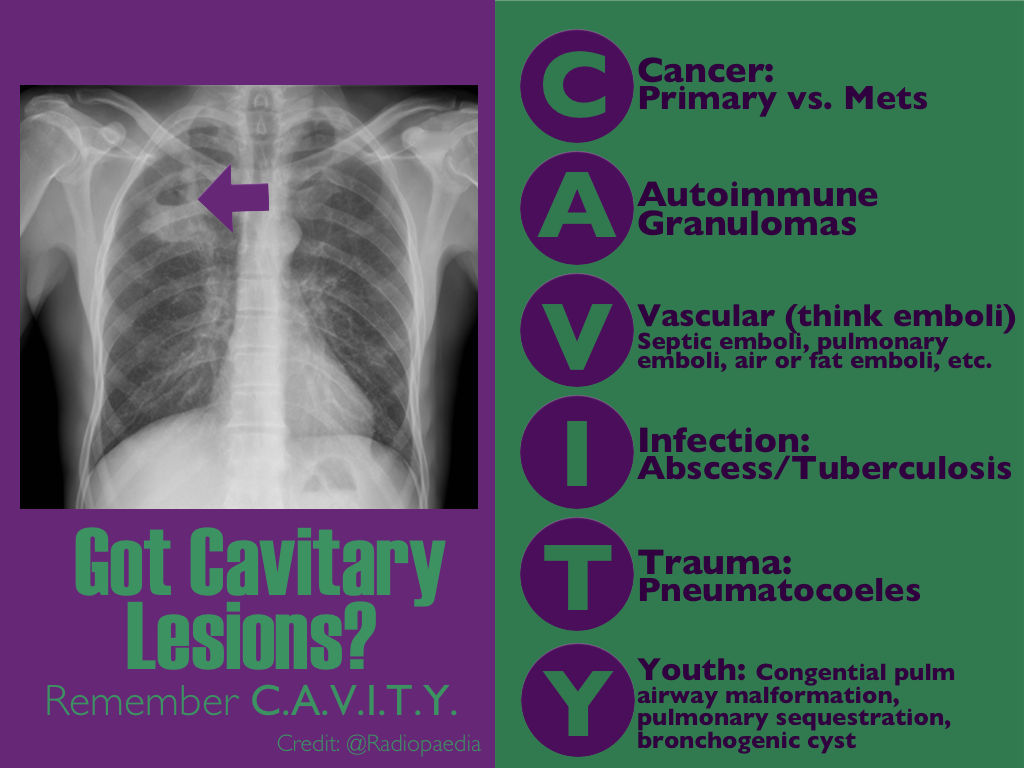
30 year-old female with complains of night sweats and painful lesions on her fingertips. What’s the diagnosis and list some things to have in the differential diagnosis?

Answer: Osler Nodes
Osler notes are painful, palpable, and erythematous lesions secondary to the deposition of immune-complexes within the pads of digits.
Although classically associated with infective endocarditis, some authors claim that it may be seen in only 10-23% of confirmed cases. Therefore the differential diagnosis should also include:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 8/5/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
There are many ventilator modes to choose from, but almost every mode can be distilled down to its basic principles by understanding the “Three T's of Mechanical Ventilation”
Trigger: You must determine whether the vent or patient will trigger a mechanical breath. For example, machine-triggered breaths (a.k.a. control mode of ventilation) are used for paralyzed patients and will deliver a breath after a period of time has elapsed (e.g., if RR is 10/min, then a breath is given every 6 seconds). On the other hand, if a patient’s respiratory drive is intact (a.k.a. assist-mode) than the patient triggers the breath when the vent detects a patient induced change in airflow or airway pressure. These two modes can also be mixed together.
Target: Mechanical breaths must have a specific target, either a target airway pressure or a tidal volume. Because pressure and volume are directly related, pick the variable you want to target and the other parameter will vary depending on the patient’s intrinsic physiology. For example, if you choose to target a specific tidal volume, we may get one plateau pressure in a patient with normal lungs, but a higher plateau pressure in another patient with stiffer lungs.
Terminate: You must decide when the mechanical breath (i.e., inspiration) terminates and expiration begins. Termination occurs: 1) after a set inspiratory time has elapsed in certain pressure-targeted modes, 2) when a predefined target volume has been achieved (i.e., volume-cycled modes), or 3) when airflow has been reduced by a certain percentage (as in pressure-support ventilation; to be discussed separately)
Let’s put this all together by looking at an example: pressure control ventilation (rate = 12/min and target pressure 20cm H20). Trigger: Because this is a “control”, not assist mode, the machine will trigger a breath 12 times per minute or every 5 seconds. Target: Here we chose to have pressure be the target, so when the ventilator triggers a breath it will deliver a constant airway pressure of 20 cmH2O until we tell the vent terminate that breath. Terminate: the constant airway pressure will be turned off after a fixed period of time has elapsed; for this example we will set the inspiratory time as 1 second, then expiration begins. Now, after a few vent breaths we will observe the results of our settings and reassess; if the resulting tidal volume is lower than what we wanted, we will increase the target pressure to increase the tidal volume. If the tidal volume is higher than what we wanted, we will reduce the target pressure to reduce the tidal volume. We can also tweak the inspiratory time to manipulate the tidal volume, but this does so to a lesser degree.
Try to break down your favorite modes of ventilation using the Three T’s and see if this helps you understand vent modes better.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 8/4/2014 by Haney Mallemat, MD
(Updated: 8/12/2014)
Click here to contact Haney Mallemat, MD
40 year-old female presents with painful lesions and ulcers on lower extremities. She has had this before, but never to this extent. She also has a history of DVT. What’s the diagnosis?
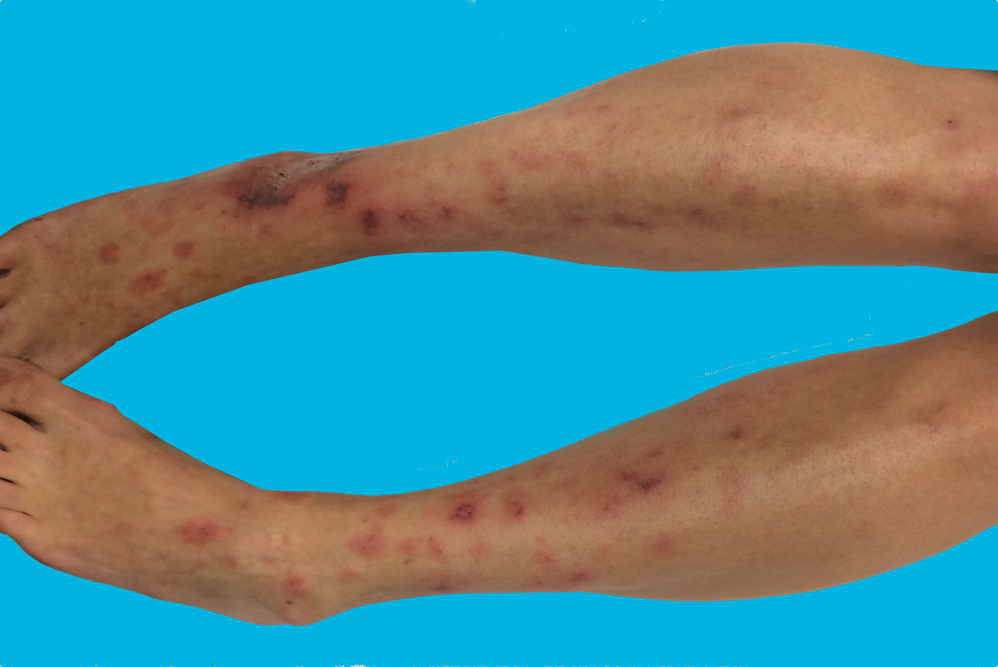
Answer: Livedoid vasculopathy or Livedoid vasculitis (LV)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 7/27/2014 by Haney Mallemat, MD
(Updated: 7/28/2014)
Click here to contact Haney Mallemat, MD
2-day old baby boy presents with forceful vomiting of entire feeds, bloated belly, and has not passed stools since birth. What's the diagnosis?
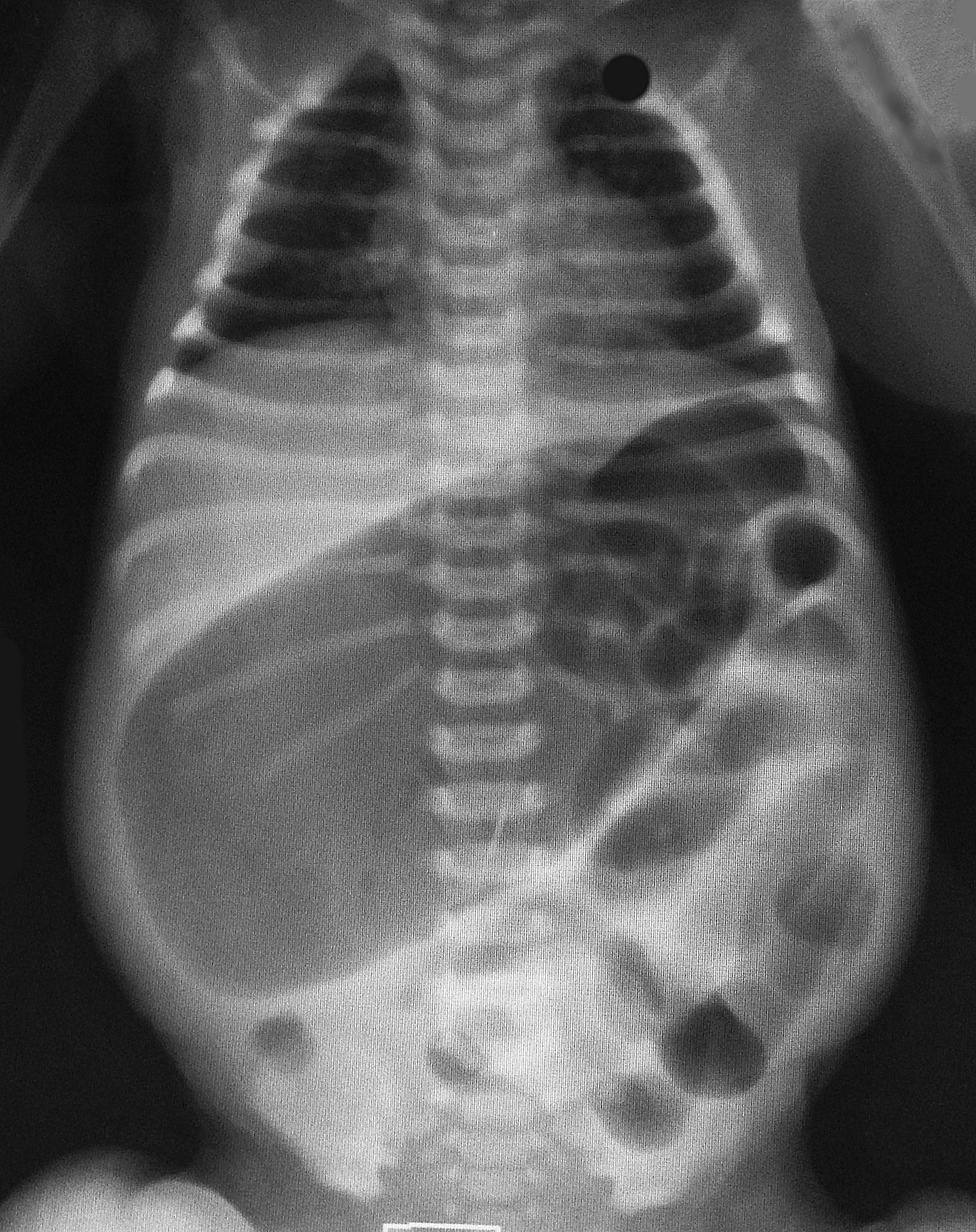
Colonic atresia
Colonic Atresia
Small bowel atresia
Meconium plug syndrome
Hirschsprung's disease
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
http://emedicine.medscape.com/article/934014-overview
Category: Visual Diagnosis
Posted: 7/21/2014 by Haney Mallemat, MD
(Updated: 7/22/2014)
Click here to contact Haney Mallemat, MD
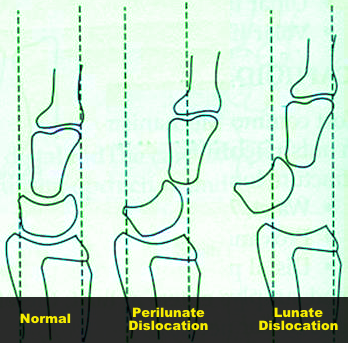
45 year-old right-hand dominant patient presents with right hand pain from a prior injury to hand. Patient has also been injecting subcutaneous heroin into hand for relief. What's the diagnosis?

Perilunate dislocation (volar displacement)...and severe hand cellulitis.
Perilunate and Lunate dislocations
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 7/14/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
30 year-old presents with cough & fever. CXR shows mild right lower lobe pneumonia. The lung ultrasound of the right lower lobe is shown below. What's the diagnosis?
Answer: Pulmonary abscess
Bottom-line: Not only is ultrasound faster than a CXR in diagnosing pneumonia, unexpected diagnoses may be found that change management
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 7/8/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Editors note: The new Back 2 Basic series will review essential critical care concepts on the first Tuesday of each month. Want a specific topic reviewed? Contact us by email or Twitter.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 7/6/2014 by Haney Mallemat, MD
(Updated: 7/7/2014)
Click here to contact Haney Mallemat, MD
10 year-old male complains of fever and rash (shown below); no other complaints. He went camping 10-days ago. What’s the diagnosis...and what medication(s) should he receive?

Rocky Mountain spotted fever (RMSF)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/30/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
49 year-old female on trimethoprim/sulfamethoxazole presents with a rash & lesions on her oral mucus membranes. What's the diagnosis?

Answer: Steven-Johnson Syndrome (SJS)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/22/2014 by Haney Mallemat, MD
(Updated: 6/23/2014)
Click here to contact Haney Mallemat, MD
35 year-old female presents with nausea and vomiting 1 week post-op for an abdominal surgery. Abdominal ultrasound is below; what's the diagnosis?
Small bowel obstruction (SBO)
Ultrasound for Small bowel obstruction (SBO)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/15/2014 by Haney Mallemat, MD
(Updated: 6/16/2014)
Click here to contact Haney Mallemat, MD
41year-old male without past medical history presents with the image below. What's the diagnosis and what's the most likely causative organism?

Gram-Negative web-space infection; most common etiologic organism is Pseudomonas
Gram Negative Web-space Infections
Gram-negative infections may occur in toe web-spaces of healthy patients, especially in areas with hyperhidrosis (excessive perspiration) and macerated skin.
Common organisms include Pseudomonas; others include Corynebacterium minutissimum (causes erythrasma, chronic superficial infection of the intertriginous areas of the skin), and other gram-negative bacteria
Woods-light examination may be clinically helpful if Pseudomonas is suspected (fluoresce green) and erythrasma will fluoresce coral red. KOH direct examination for fungal elements may show the presence of dermatophytes or Candida.
Treatment:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Wolff, K., & Johnson, R. J. (2009). Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology. (6th ed., pp. 662-664;698). McGraw-Hill.
http://www.aafp.org/afp/2005/0901/p833.html
http://emedicine.medscape.com/article/1055306-overview
Category: Critical Care
Posted: 6/10/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/8/2014 by Haney Mallemat, MD
(Updated: 6/9/2014)
Click here to contact Haney Mallemat, MD
28 year-old female with history of chronic back pain presents with right-foot numbness and inability to move her foot at the ankle joint. What’s the diagnosis and what neurologic finding would you expect to find?

Large disc bulge at L5-S1
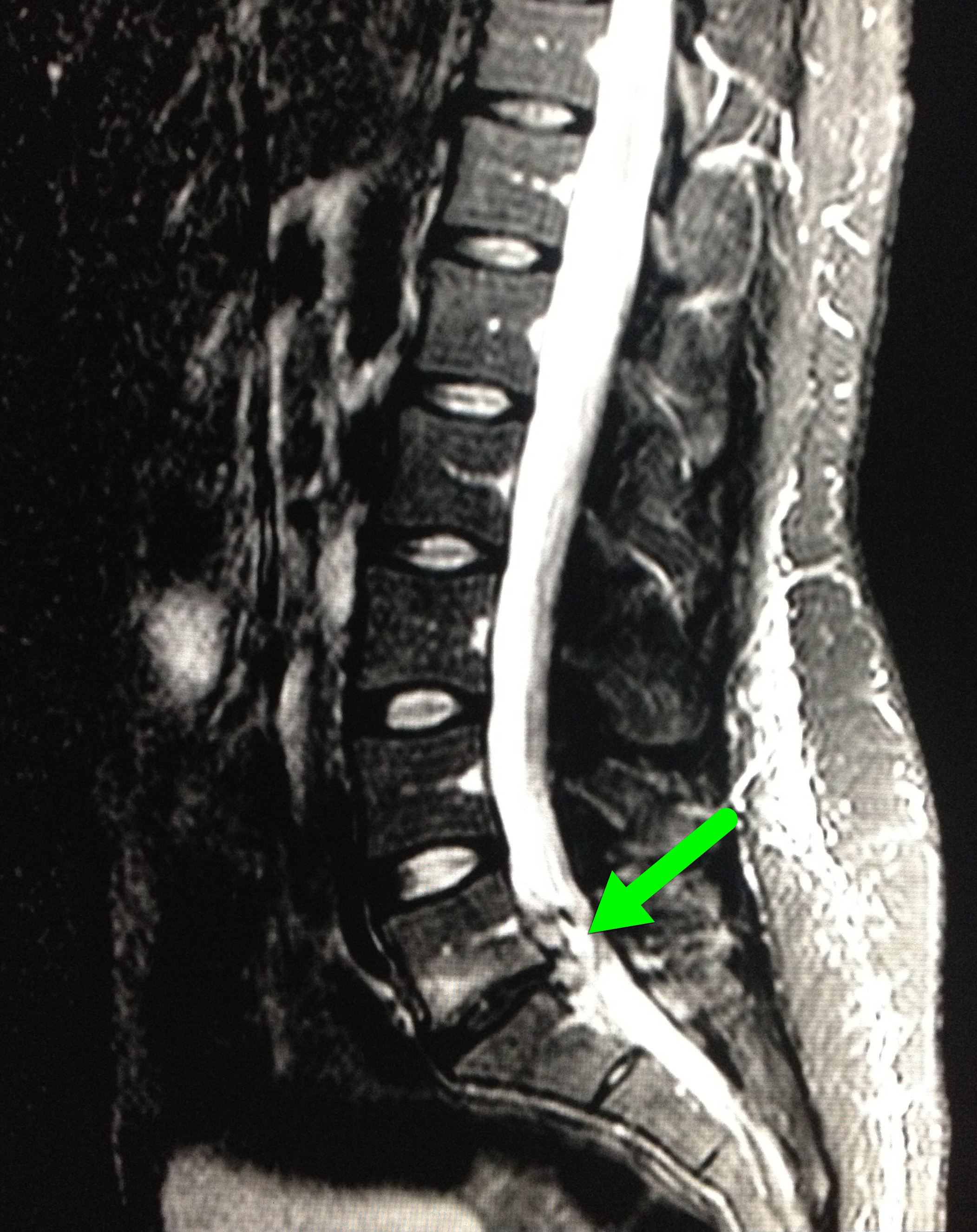
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/2/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
30 year-old female with elbow pain following a fall. What's the diagnosis? (bonus points if you name the fracture with an associated radio-ulnar joint dislocation)

Radial Head Fracture
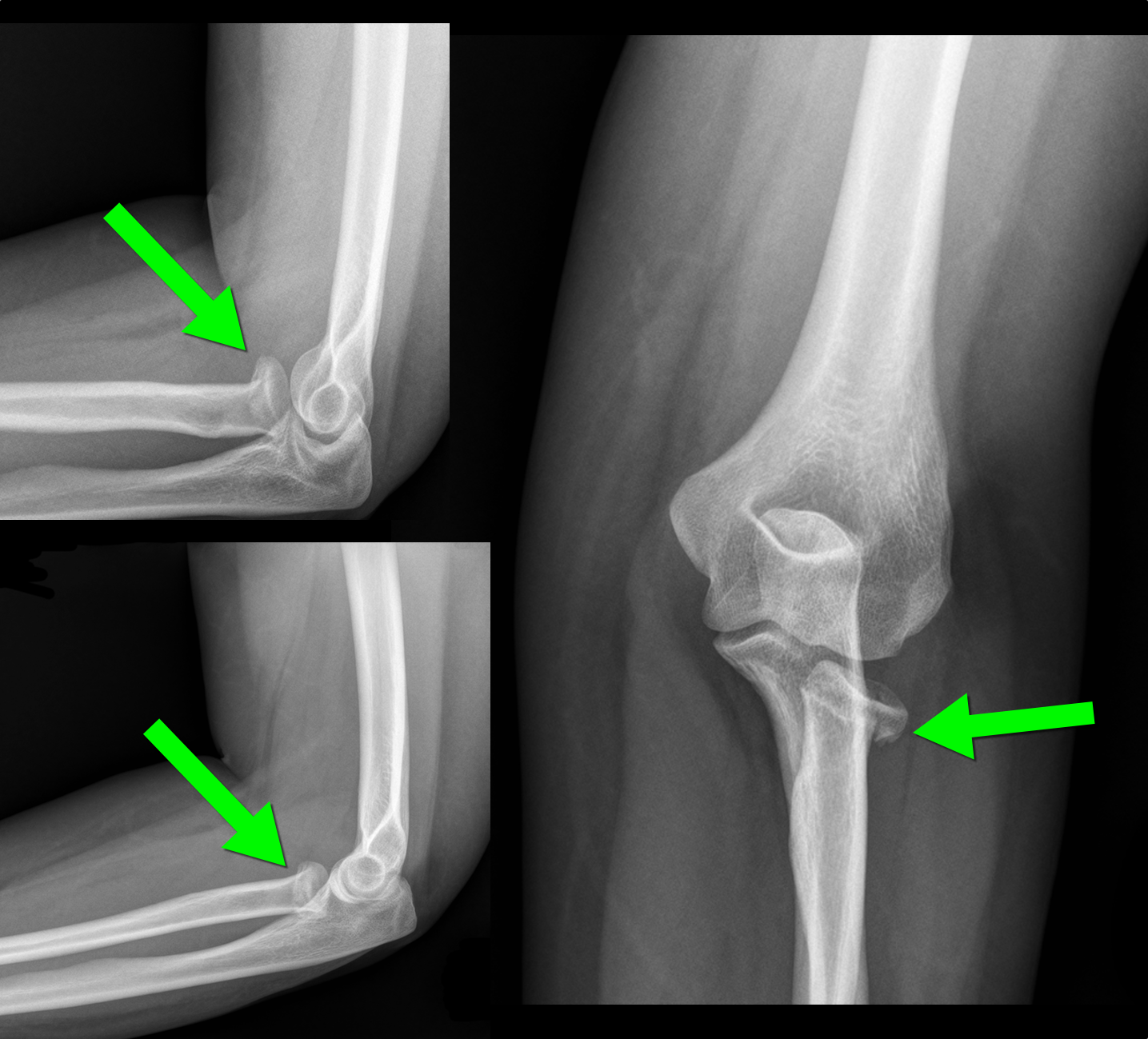
 d
d
http://www.wheelessonline.com/ortho/radial_head_frx
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 5/26/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Diabetic patient with active intravenous drug use presents with hypotension, fever, and tenderness of right arm. What's the diagnosis and what antibiotic(s) would you start?
Right arm with necrotizing fasciitis
http://lifeinthefastlane.com/education/ccc/necrotising-fasciitis/
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
