Category: Visual Diagnosis
Posted: 1/19/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
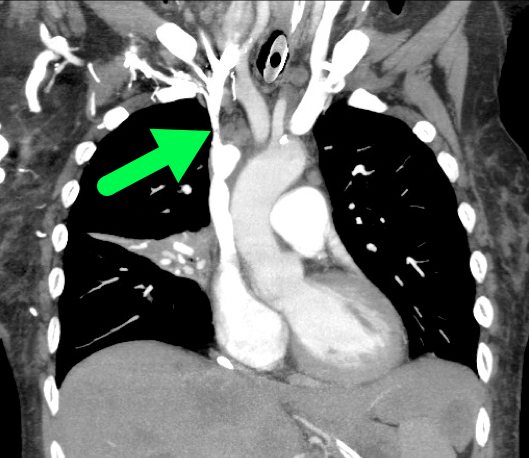
60 year-old male presents with 6 months of weight loss,epistaxis, and increased headache when bending over. What's the diagnosis?
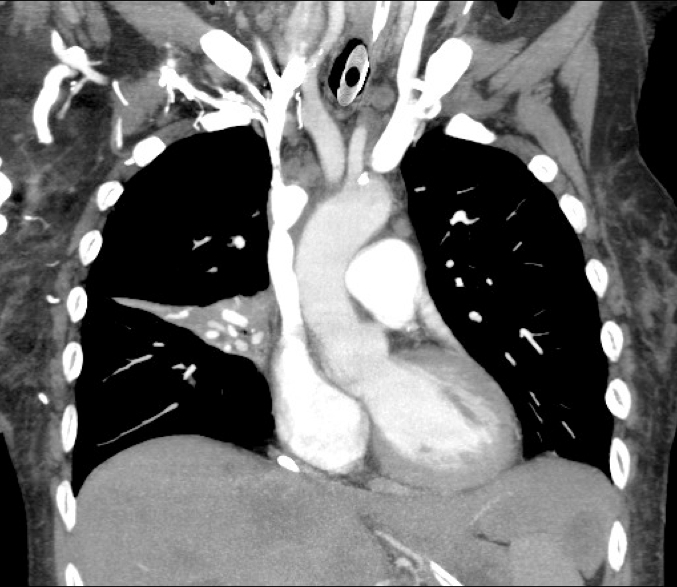
SVC Syndrome
Rice TW, Rodriguez RM, Light RW. The superior vena cava syndrome: clinical characteristics and evolving etiology. Medicine (Baltimore). Jan 2006;85(1):37-42.
Nunnelee JD. Superior vena cava syndrome. J Vasc Nurs. Mar 2007;25(1):2-5
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/12/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
60 year-old male presents with rhinorrhea, body aches, and dry cough for two days. He recently moved here from Kentucky. What’s the diagnosis (please note that there are several differentials based on CXR)?
Answer Histoplasmosis
Histoplasma capsulatum is the fungus that causes histoplamosis, and is endemic to soil in the “Histo belt” of the U.S. (including all of Arkansas, Kentucky, Missouri, Tennessee, and West Virginia and parts Alabama, Illinois, Indiana, Iowa, Kansas, Louisiana, Maryland, Mississippi, Nebraska, Ohio, Oklahoma, Texas, and Virginia); it is found internationally as well.
Outbreaks have occurred following digging up the ground at construction at sites where this yeast lives in the soil, but spores can also become airborne and inoculate people.
Most cases are asymptomatic, but it is associated with a variety of pulmonary syndromes and can have extrapulmonary findings such as splenic calcifications. Disseminated disease typically occurs in immunocompromised patients
Treatment includes itraconazole for mild to moderate disease and amphotericin for disease that is severe or widespread disease.
Differentials:
- Blastomycosis
- Septic emboli
- Sarcoidosis
- Tuberculosis (milliary)
- Aspergillosis
- Carcinoid lung tumor
- Atypical or viral pneumonias
Category: Visual Diagnosis
Posted: 1/5/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
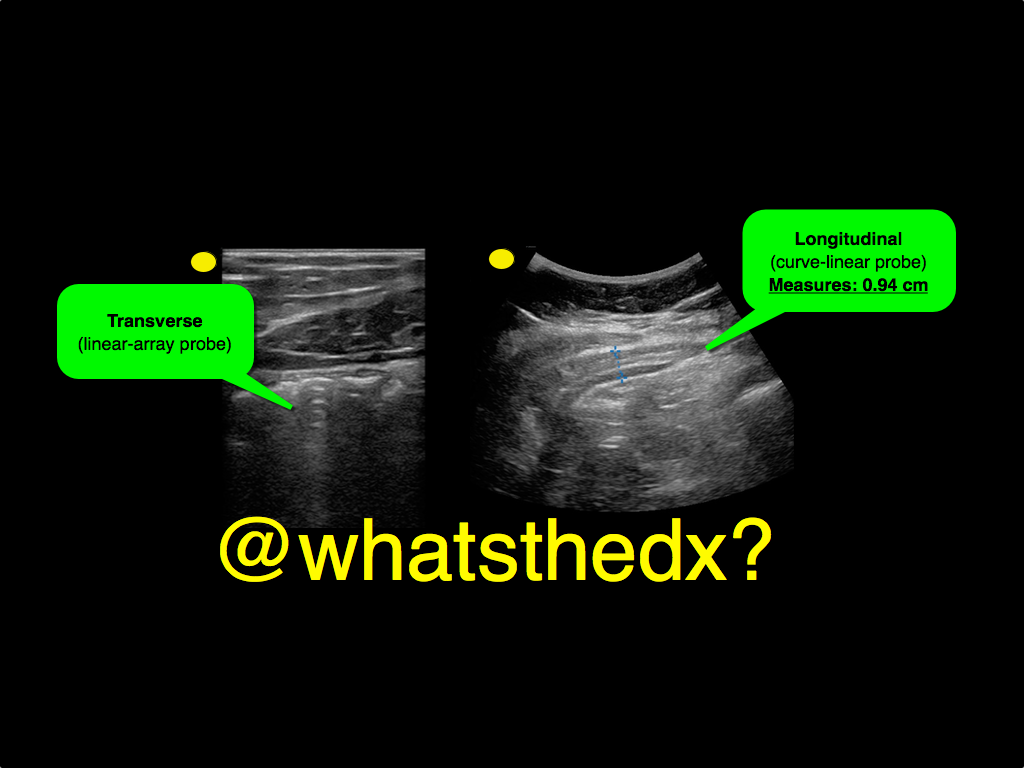
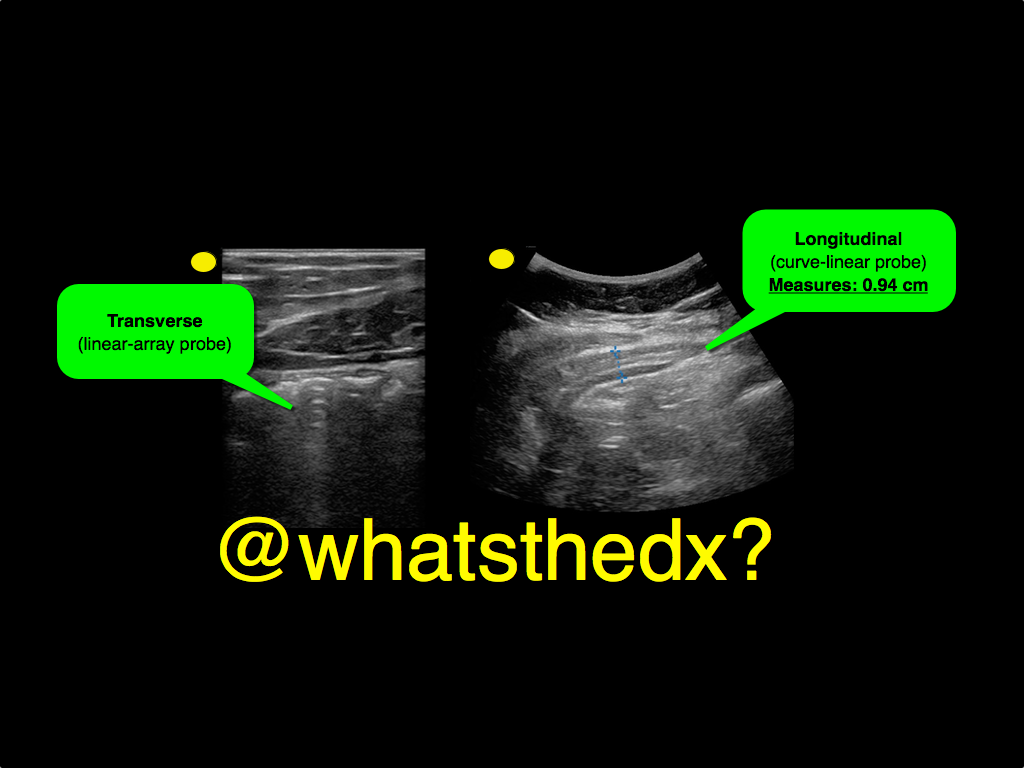
A male patient presents with right lower quadrant pain. The ultrasound is shown at the point of maximal tenderness. The diameter of the structure (image on right) is about 0.94cm. What is this structure and what's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/29/2014 by Haney Mallemat, MD
(Updated: 12/30/2014)
Click here to contact Haney Mallemat, MD
19 year-old male complaining of left arm pain one week after injecting anabolic steroids into his sholder. What's the diagnosis?
Myositis of the deltoid muscle
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 12/23/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Treating ischemic strokes with interventional therapies (e.g., clot retrievers, stents, intra-arterial tPA, etc.) is nothing new, but there has never been a randomized control trial demonstrating benefit until recently.
The prospective MR CLEAN trial evaluated whether interventional therapies (i.e., either mechanical intervention or intra-arterial tPA) would confer benefit; patients were included if there was an acute occlusion within the proximal intracranial portion of the anterior cerebral circulation.
90% of patients received alteplase prior to randomization; there were 233 patients in the intervention group (alteplase + intraarterial intervention) and 267 patients in the usual care care arm (alteplase only); all patients were treated within 6 hours of symptoms onset
The primary outcome was functional independence at 90 days; an absolute difference of 13.5 percentage points favoring the intervention group was found. There were no significant differences in mortality or symptomatic intracerebral hemorrhage.
Despite these exciting results, we must pause and ask why this was this the first randomized trial demonstrating benefit when previous trials could not? Here are three blogs posts that deep dive this question and raise even more questions:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/21/2014 by Haney Mallemat, MD
(Updated: 12/23/2014)
Click here to contact Haney Mallemat, MD
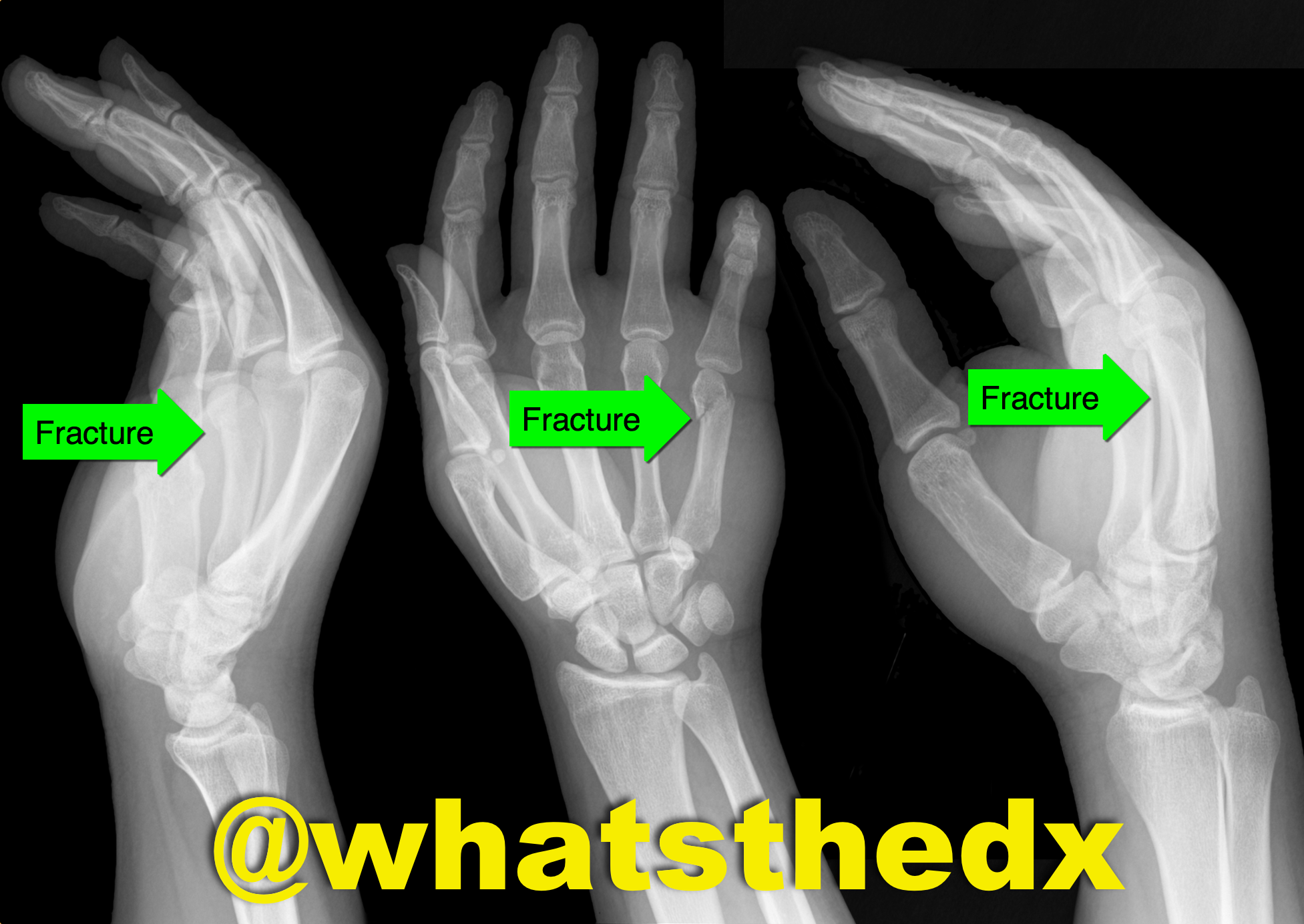
Hand pain following fist versus face. What's the diagnosis and what nerve block would you use?

Boxer's fracture. Read more here.
Pain control can be achieved with an ulnar nerve block (e.g., reducation if if angulated). A video for the technique using ultrasound can be found here.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/15/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A patient is intubated for respiratory failure and the post-intubation CXR is shown on the left. 30 minutes later the patient desaturates and another CXR is obtained (the one on the right). What’s the diagnosis and what should you do?
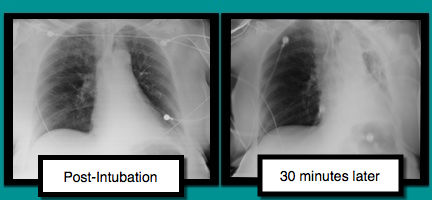
Mucus plug
There are several conditions to consider when patients are having difficultly being ventilated. The approach to such a patient can be remembered with a mnemonic found here.
In this case, conditions to consider are:
Treating mucus plugs can usually be treated as follows:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/8/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient was found in a house fire and was given a certain medication in the Emergency Room. The patient’s urine turned this color (red), what’s the diagnosis?

Hydroxocobalamin (i.e., Cyanokit)
Cyanide toxicity
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/1/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient presents with dyspnea. What's the diagnosis and name three potential causes (can be specific to the case or in general)?

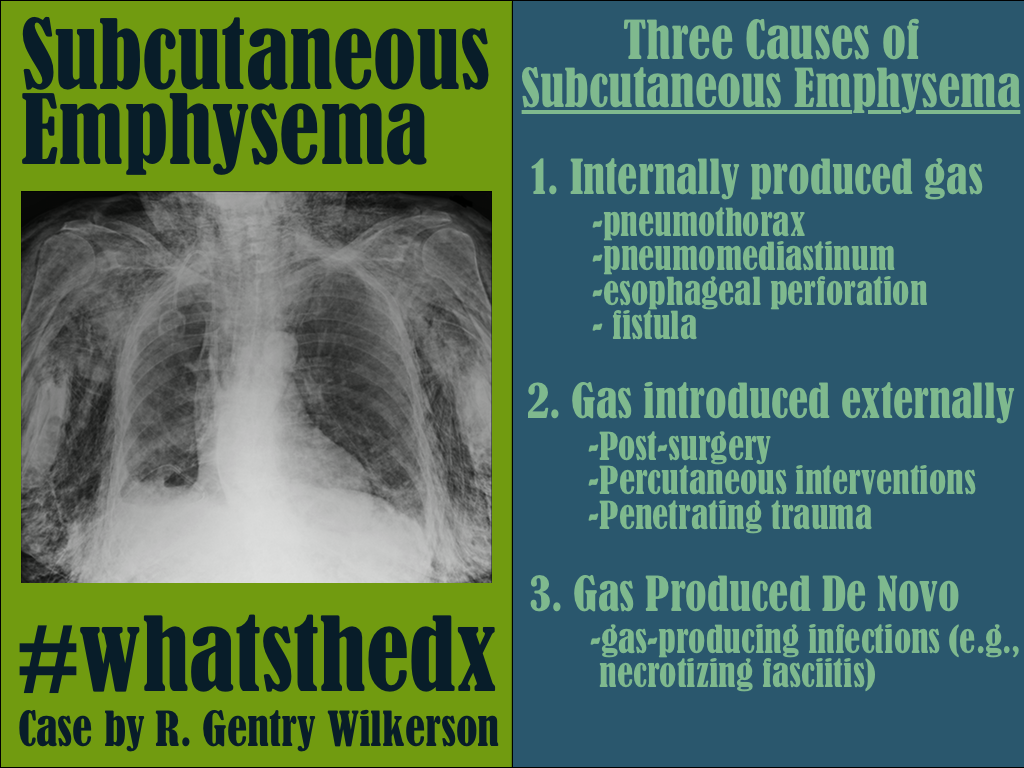
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 11/25/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Running a successful resuscitation not only means doing everything right, but also remembering all the things that can go wrong. A.E.I.O.U. is a simple mnemonic that can help you remember the simple things that are sometimes forgotten during a medical resuscitation.
A – Advanced airway equipment to bedside, as well as checking the correct placement of the Airway if a patient is intubated in the field. Also consider adding another A, for Arterial line; early placement can help with pulse checks and an accurate assessment of blood pressure should there be return of spontaneous circulation (ROSC); the femoral site is fast and accurate.
E – End-tidal CO2 (ETCO2) helps detect ROSC. Ask for the ETCO2 monitor to be set up right after you receive notification of an arrest in transit; ETCO2 requires time to set-up / calibrate
I – Intraosseous line(s); compared to peripheral or central venous access, IO’s are faster, safer, and any medication can be administered through it, including vasopressors / inotropes.
O – Order (i.e., “who’s who in the Resus room?); You may be the team leader or you may be assisting, but it is important that you, and everyone else in the room, know their role prior patient arrival. If you are leading the resus, be sure everyone knows who you are, and assign everyone in the room a specific task (e.g., chest compressions, IO placement, etc.). If you are assisting and have not been assigned a task, ask the resus leader what you can do to help. If there is nothing immediate for you to do then take the initiative to de-clutter the room and step outside; be nearby and ready to help, if needed.
U – Ultrasound; can help prognosticate and detect reversible causes (e.g., pericardial tamponade). Have the ultrasound machine in the room prior to patient arrival. It should be powered on, with the proper probe connected, and in the proper mode. The most experienced ultrasonographer should scan the patient during a pulse check; experience is vital because hands-off time should be minimized.
*Tips for the Resuscitationist (#TFTR) is a new series to help you to better manage your critically ill patients. Do you have an idea for a topic or do you have a tip you would like to share? Send it to us via twitter @criticalcarenow (use (#TFTR)). You can also email us here.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/23/2014 by Haney Mallemat, MD
(Updated: 11/25/2014)
Click here to contact Haney Mallemat, MD
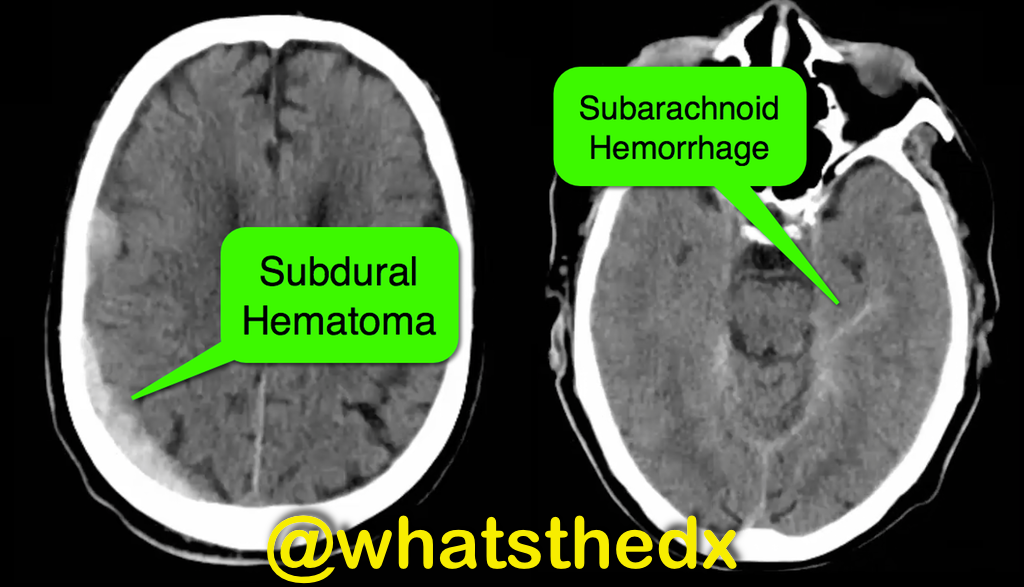
Patient with syncope and then falls down the stairs. What's the diagnosis? (hint: be very,very careful)

Right subdural hematoma and left subarachnoid hemorrhage
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/17/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient presents with dyspnea & hypoxemia (pulse oximeter is 80%). The "stat" CXR is delayed, but ultrasound is not. What's the diagnosis and what are some differential diagnoses?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/10/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Parasternal long-axis of two different patients. What is the:
Answer:
Take home pearl: when there is fluid behind the heart, the parasternal long-axis view of the heart is helpful to distinguish between a pleural effusion and a pericardial effusion.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/4/2014 by Haney Mallemat, MD
(Updated: 11/5/2014)
Click here to contact Haney Mallemat, MD
A patient presents post-motor vehicle crash with chest pain and dyspnea. The lung ultrasound is shown below. What's the diagnosis?
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 10/20/2014 by Haney Mallemat, MD
(Updated: 11/4/2014)
Click here to contact Haney Mallemat, MD
13 year-old right-hand dominant following assault with blunt object. What’s the diagnosis?

Monteggia Fracture
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 10/13/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A neck ultrasound is performed during endotracheal intubation. What is labeled "A", what is labeled "B" and what's the diagnosis?
Answer:
A: Trachea
B: Esophagus
This is an esophageal intubation! Take out the tube and try again. Check out this podcast for more on the technique from my good friends at the ultrasound podcast
Here's a summary:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 10/6/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
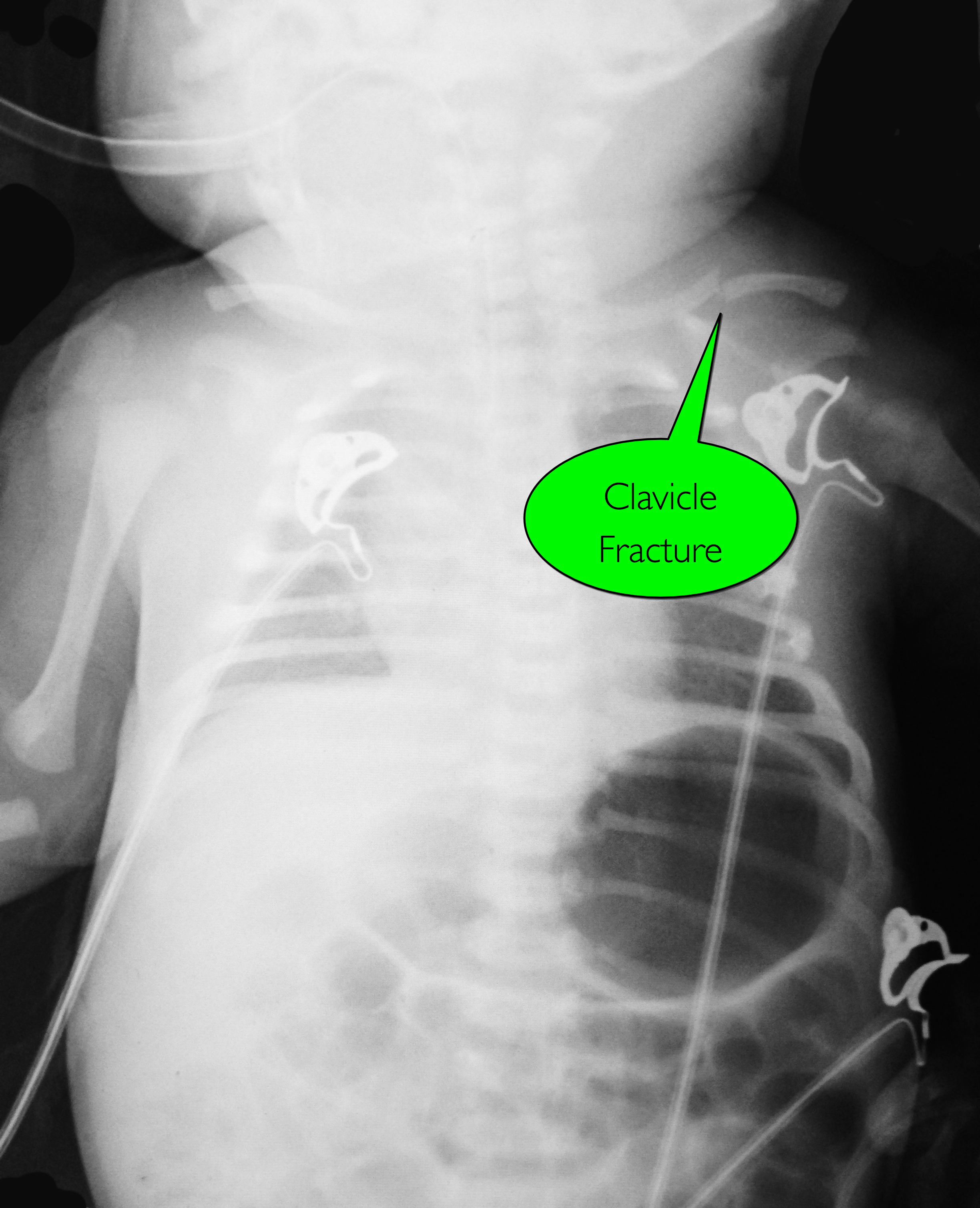
7d old child presents with difficulty feeding,vomiting one time, and now with intermittent apneic episodes. What's the diagnosis? (Careful....this one is tricky!)
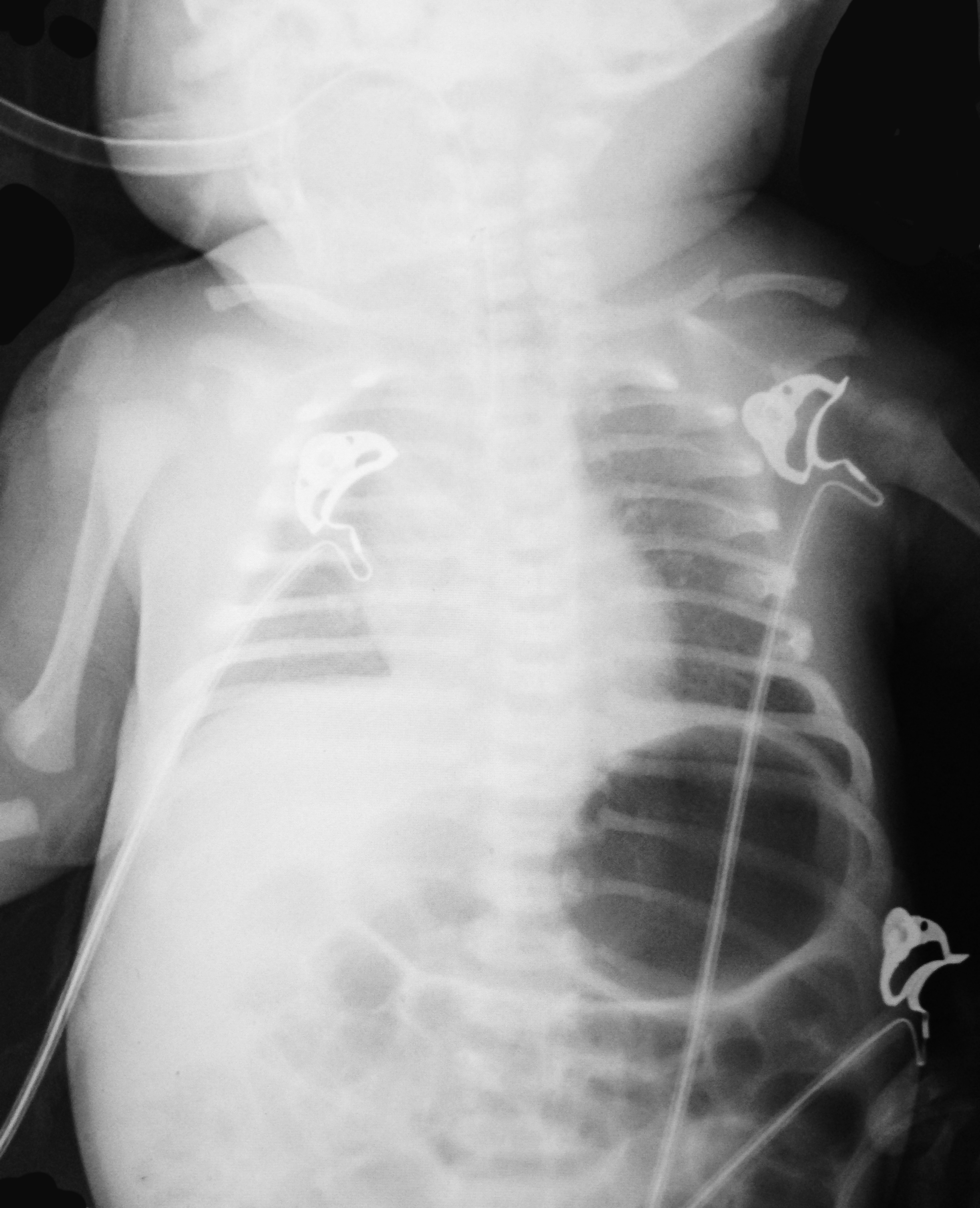
Answer: Workup should include an ALTE and sepsis evaluation PLUS evaluation for non-accidental trauma
Non-accidental trauma (NAT)
NAT is most prevalent in children 0-3 months of age.
Classic metaphyseal lesions, rib fractures, and fractures in various stages of healing are most commonly described in children.
How do we know this is not just birth trauma from a shoulder dystocia, large for gestational age, or difficult vaginal delivery?
Subperiosteal new bone formation appears as a:
NAT Work-up:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 9/30/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
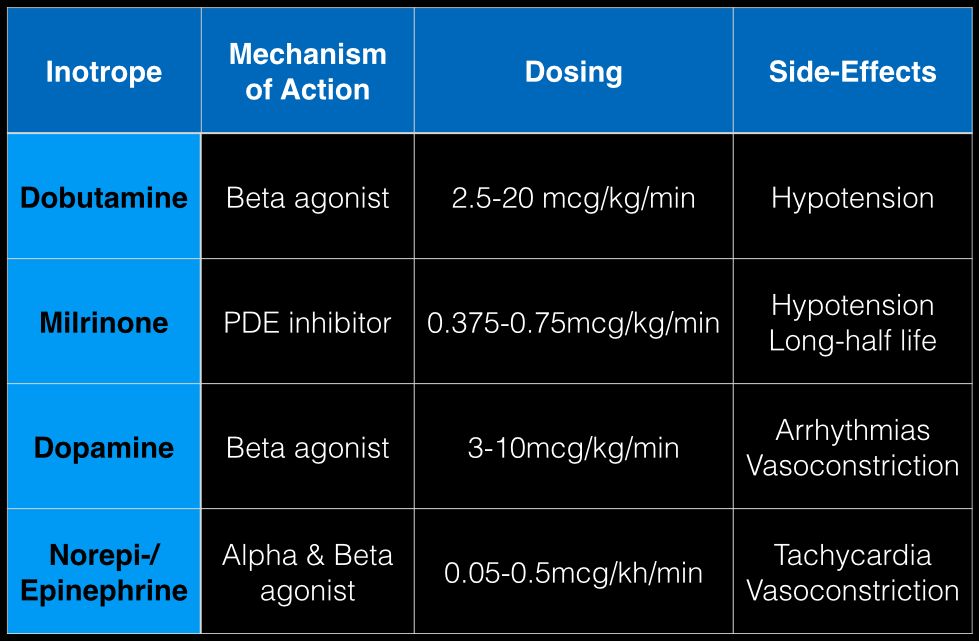
The last Back to the Basics post discussed the use of vasopressors to improve hemodynamics by increasing arterial (and venous) tone. This time we’ll discuss the use of agents to increase inotropy for patients with severe systolic dysfunction / failure.
Dobutamine: a direct b1 and b2-receptors agonist. It has no peripheral vasoconstrictor properties, so if blood pressure increases it occurs secondary to increased cardiac output. Unfortunately, blood pressure may be decreased in some patients due to its peripheral vasodilatory effects; in these cases it may need to be used with a vasopressor.
Milrinone: augments contractility by increasing intracellular Ca levels via cellular phosphodiesterase inhibition. Because it does not work on beta-receptors, it might be preferred for patients taking beta-blockers requiring inotropic support. It may cause peripheral vasodilation and hypotension, but this may be a benefit if pulmonary artery pressure is elevated as reductions in pulmonary artery pressure lead to improvements in right ventricular function. It has a long-half life and should be avoided in patients with renal impairment.
Dopamine: chemical precursor to norepinephrine and technically a vasopressor. At moderate doses (3-10 mcg/kg/min) it works on beta-receptors to increase myocyte contractility. At higher doses works primarily as a vasopressor, which may reduce cardiac output due to higher afterload.
Norepinephrine/epinephrine: has alpha and beta properties that lead to increased peripheral vasoconstriction, but also increases inotropy and chronotropy (faster heart rate)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)a
Category: Visual Diagnosis
Posted: 9/28/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
Person presents with painless vision loss after seeing flashes of light. Ultrasound is below. What's the diagnosis?
Answer: Vitreous hemorrhage with retinal detachment
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 9/15/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
Football player complains of sudden foot pain after begin tackled. What’s the diagnosis?

Lisfranc fracture-dislocation
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
