Category: Visual Diagnosis
Posted: 12/11/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
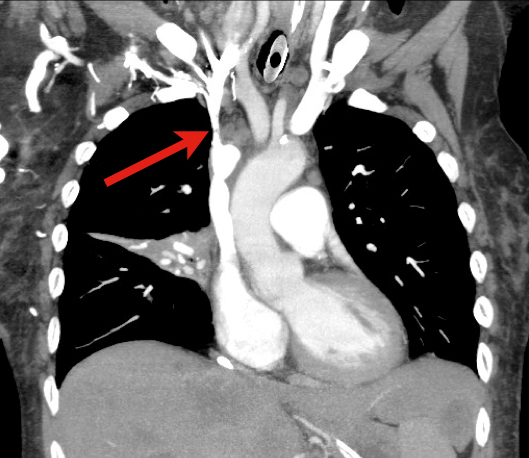
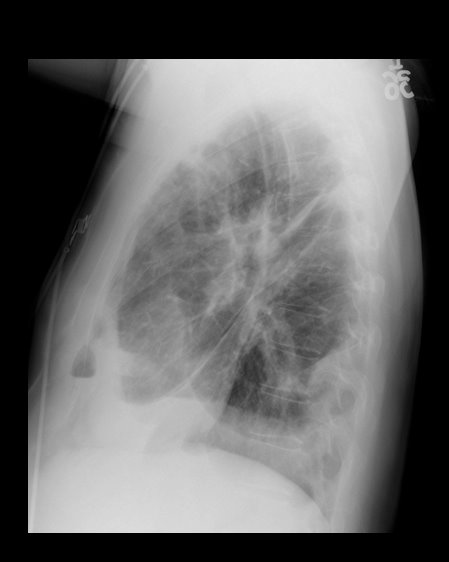
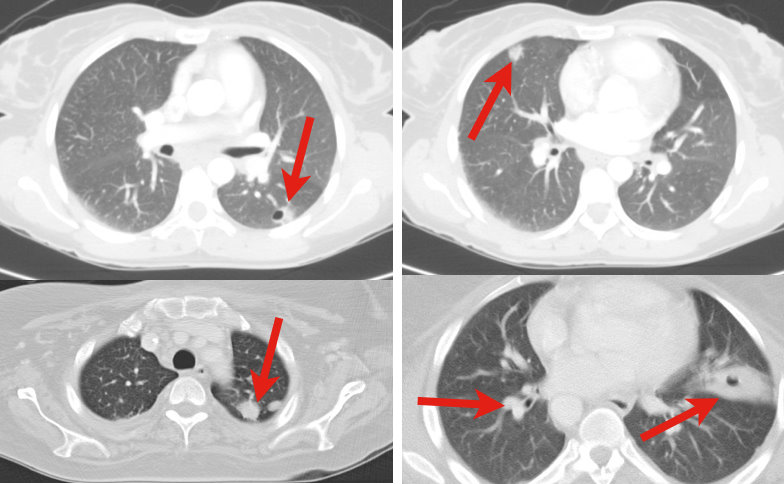
60 year old male with 6 months of weight loss and recent epistaxis. Diagnosis?
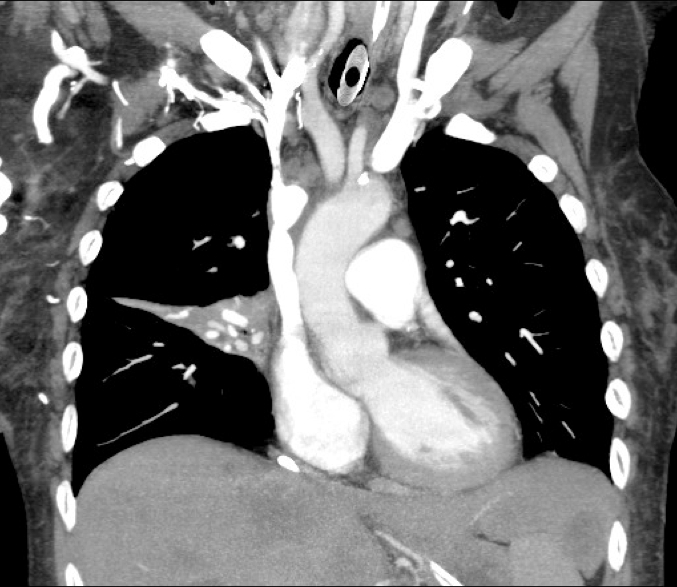
Answer: Partial obstruction of the Superior vena cava (SVC)
SVC Syndrome
SVC syndrome is caused by compression or obstruction of the superior vena cava blocking anterograde flow.
Most cases are secondary to extrinsic compression by malignancy. Other causes are secondary to thrombosis and internal obstruction (e.g., central venous catheter placement).
Symptoms present sub-acutely, worsen with bending over, and are secondary to increased venous pressure in the head and neck (e.g., epistaxis, headache, tinnitus, conjunctival injection, neck swelling, etc.).
Treatment focuses on reversing the underlying cause (e.g., radiation or chemotherapy if due a sensitive tumor) and treatment of symptoms:
Rice TW, Rodriguez RM, Light RW. The superior vena cava syndrome: clinical characteristics and evolving etiology. Medicine (Baltimore). Jan 2006;85(1):37-42.
Nunnelee JD. Superior vena cava syndrome. J Vasc Nurs. Mar 2007;25(1):2-5; quiz 6.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 12/6/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Up until recently, a tight-fitting mask was one of the only ways to deliver non-invasive positive-pressure ventilation.
High-flow nasal cannulas (HFNC) have been adapted from use in neonates to adults to deliver continuous positive airway pressure (CPAP).
HFNC provides continuous, high-flow (up to 60 liters), and humidified-oxygen via nasal cannula providing positive pressure to the pharynx and hypopharynx. Patients tolerate it well and it is less claustrophobic than tight-fitting masks.
HFNC does not generate the same amount of pressure as CPAP so it may be best utilized as an intermediate step between low-flow oxygen (i.e., traditional nasal cannula) and non-invasive positive pressure ventilation with tight-fitting masks.
Check with your respiratory department if these devices are locally available.
Kernick, j. What is the evidence for the use of high flow nasal cannula oxygen in adult patients admitted to critical care units? A systematic review. Aust Crit Care. 2010 May;23(2):53-70. Epub 2010 Mar 5.
Parke, R. A preliminary randomized controlled trial to assess effectiveness of nasal high-flow oxygen in intensive care patients. Respir Care. 2011 Mar;56(3):265-70. Epub 2011 Jan 21.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/27/2011 by Haney Mallemat, MD
(Updated: 11/28/2011)
Click here to contact Haney Mallemat, MD
9 year-old boy with sudden onset of unilateral facial swelling. What’s the diagnosis?

Answer: Acute Parotitis
Bonus Trivia: U.S. President Garfield died from parotitis after becoming dehydrated following abdominal surgery
Shelly J. McQuone MD, Acute Viral and Bacterial Infections of the Salivary Glands, Otolaryngologic Clinics of North America, Volume 32, Issue 5 (October 1999)
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: hypotension, shock, ultrasound, hi map (PubMed Search)
Posted: 11/22/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Determining the exact etiology of hypotension / shock can sometimes be difficult in the Emergency Department.
The Rapid Ultrasound for Shock / Hypotension (RUSH) exam is a sequential, 5 step-protocol (typically requiring less than 2 minutes) that can be used to determine the cause(s) of hypotension.
The mnemonic for the exam is “HI MAP”, and is easy to remember because a "HI MAP" is our goal with hypotensive patients.
H - Heart (parasternal and four-chamber views)
I - Inferior Vena Cava (for volume responsiveness)
M - Morrison’s pouch (i.e., FAST exam) and views of thorax (looking for free fluid)
A - Aortic Aneurysm (ruptured abdominal aneurysm)
P - Pneumothorax (i.e., Tension PTX)
Refer to the link for a more detailed discussion and podcast from the creators of this exam: emcrit.org/rush-exam
Category: Critical Care
Keywords: tamponade, critical care, intubation, positive pressure, PEA arrest (PubMed Search)
Posted: 11/8/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Positive-pressure ventilation (e.g., mechanical ventilation) increases intrathoracic pressure potentially reducing venous return, right-ventricular filling, and cardiac output.
Pericardial tamponade similarly causes hemodynamic compromise through increased pericardial pressure which reduces right-ventricular filling and cardiac output.
When mechanically ventilating a patient with known or suspected pericardial tamponade the mechanisms above may be additive, causing cardiovascular collapse and possibly PEA arrest.
For the patient with known or suspected pericardial tamponade consider draining the pericardial effusion prior to intubation or delaying intubation until absolutely necessary.
If intubation is unavoidable, consider maintaining the intrathoracic pressure as low as possible (by keeping the PEEP and tidal volumes to a minimum) to ensure adequate cardiac filling and cardiac output.
Ho, A. et. al. Timing of tracheal intubation in traumatic cardiac tamponade: A word of caution. Resuscitation, 80(2), 272–274.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 10/30/2011 by Haney Mallemat, MD
(Updated: 10/31/2011)
Click here to contact Haney Mallemat, MD
72 year-old man, one-week post right fem-pop bypass presents with painful blue and black toe. Diagnosis?

Answer: Blue-Toe Syndrome
Hirschman, J. et al. Blue (or purple) toe syndrome. J Am Acad Dermatol.2009 Jan;60(1):1-20
O'Keeffe S, et al. Blue toe syndrome: Causes and management.Arch Intern Med. 1992 Nov;152(11):2197-202.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: xigris, activated protein C, sepsis, multi-organ failure, resuscitation (PubMed Search)
Posted: 10/25/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
On October 25, 2011, Eli Lilly announced a voluntary-recall of activated drotrecogin alfa (Xigris) following a recent trial (PROWESS-SHOCK), which demonstrated no survival benefit when using the drug when compared to placebo.
Activated drotrecogin alfa is a recombinant form of human activated protein C previously recommended for adults with severe sepsis and a high-risk of death (APACHE II > 25 or multi-organ failure); it is included in the 2008 International Sepsis Guidelines (Grade 2b recommendation).
The PROWESS-SHOCK trial reported an all-cause mortality rate of 26.4% in the drotrecogin alfa group compared with 24.2% in the placebo group; this difference was not statistically significant.
Interestingly, the study also found that severe bleeding (the drug's main side-effect) was found to be 1.2% in the activated drotrecogin alfa group compared to 1.0% for the placebo group (also non-significant) suggesting it does not increase the risk of bleeding as it had previously been reported.
Hospitals should revise their sepsis guidelines based on this recent news.
www.medscape.com/viewarticle/752169?sssdmh=dm1.728719&src=nl_newsalert
Dellinger, R. P., et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Critical Care Medicine, 36(1), 296–327. doi:10.1097/01.CCM.0000298158.12101.41
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 10/17/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
5 year-old male with developmental delay presents with intractable non-bloody and non-bilious vomiting over 10 days; bowel movements are normal. Four weeks ago he was placed in a hip-spica cast following a motor vehicle crash. Abdominal x-ray is below. Diagnosis?

Answer: CAST syndrome (also known as Superior Mesenteric Artery Syndrome)
Wheeless Textbook of Orthopedics. Updated August 29,2011
Lichenstein, R. Radiology Cases in Pediatric Emergency Medicine, Volume 5, Number 16
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: listeria, food borne illness, cns infection (PubMed Search)
Posted: 10/11/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Lisiteria Monocytogenes is typically transmitted from ingestion of contaminated food such as unpasteurized milk or cheese, raw foods, and recently cantaloupes; transmission from veterinary exposure, infected soil and water have also been reported.
Listeria has a predilection for the central nervous system (CNS) causing several infections including meningioencephalitits, brain or spinal abscess, cerebritis (infection of brain parenchyma), and rhomboencephalitis (encephalitis of the brainstem).
Risk factors include immunosuppression, advanced age, newborns, and pregnancy.
There is no clinical way to distinguish CNS infection with Listeria from other pathogens, therefore blood and cerebrospinal fluid (CSF) culture is required.
CSF analysis demonstrates pleocytosis, elevated protein, and low glucose. CSF gram stain has a low sensitivity (~33%), but consider Listeria in the differential if "diptheroid-like" bacteria are reported on gram stain.
Ampicillin is the drug of choice and should be continued for at least three weeks (sometimes longer). Adding gentamycin is sometimes recommended for synergy in severe infection.
Mylonakis E, Hohmann EL, Calderwood SB. Central nervous system infection with Listeria monocytogenes. 33 years' experience at a general hospital and review of 776 episodes from the literature. Medicine (Baltimore). Sep 1998;77(5):313-36.
http://emedicine.medscape.com/article/220684-overview
http://www.cdc.gov/listeria
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 10/3/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Question: 50-year-old diabetic female s/p foot burn several weeks ago, now presenting with pain and discharge from a poorly healing wound. Diagnosis?

Answer: Osteomyelitis
Osteomyelitis
· Acute or chronic bone infection
· Risk factors: Immunosuppression (diabetes, chronic steroid use, AIDS, and sickle-cell dz.)
· Secondary to direct trauma, contiguous spread from local infection, or hematogenous spread (in children)
· Common bacteria: S. Aureus, Pseudomonas, Salmonellae (classically in Sickle cell dz.)
· X-ray (limited sensitivity):
- 3-5 days post-infection: Soft-tissue swelling
- 14-21 days: Some patients demonstrate bony changes (e.g., periosteal elevation, bone lucencies, etc.)
- >28 days: >90% with Xray findings
· MRI is the imaging gold standard
· Two of the following needed for diagnosis:
- Purulent aspiration
- Positive blood or tissue culture
- Positive imaging
- Tenderness + erythema / edema
· Antibiotic coverage based on culture results. When immediate empiric therapy required (sepsis), cover most likely pathogen plus MRSA.
References
Carek PJ, Dickerson LM, Sack JL. Diagnosis and management of osteomyelitis. Am Fam Physician. 2001 Jun 15;63(12):2413-20.
Pruthi S, Thapa MM. Infectious and inflammatory disorders. Radiol Clin North Am. Nov 2009;47(6):911-26.
Zink BJ, Raukar NP. Bone and Joint Infections. In: Marx JA, Hockberger RS, Walls RM, Adams JG, Barsan WG, Biros MH, Danzl DF, Gausche-Hill M, Ling LJ, Newton EJ, eds. 7th ed. Emergency Medicine: Concepts and Clinical Practice.Volume 2. Philadelphia, PA: Mosby; 2010:1821-1830.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: Epinephrine, adrenaline, cardiac arrest, return of spontaneous circulation, ROSC, critical care, ICU, saline (PubMed Search)
Posted: 9/27/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
· The use of epinephrine in cardiac arrest is currently standard of care.
· Several observational and non-randomized trials have demonstrated the efficacy of epinephrine in cardiac arrest, but there has never been a randomized double-blind placebo-controlled trial in humans.
· A recently published Australian trial randomized cardiac patients (of any type) to receive either 1 mg of epinephrine (n=272) or 0.9% normal saline (n=262); the primary end-point was survival to hospital discharge. Secondary end-points were pre-hospital return of spontaneous circulation (ROSC) and neurological outcomes at hospital discharge.
· Significantly more patients had pre-hospital ROSC in the epinephrine group (regardless of the underlying rhythm), however, there was no statistically significant difference in survival to discharge (the primary outcome) between groups.
· This randomized double-blinded placebo-controlled trial raises many new and interesting questions about epinephrine, but more study is needed before changing current practice.
Jacobs IG, et al. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomized double-blind placebo-controlled trial. Resuscitation 2011;82:1138-1143.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 9/19/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
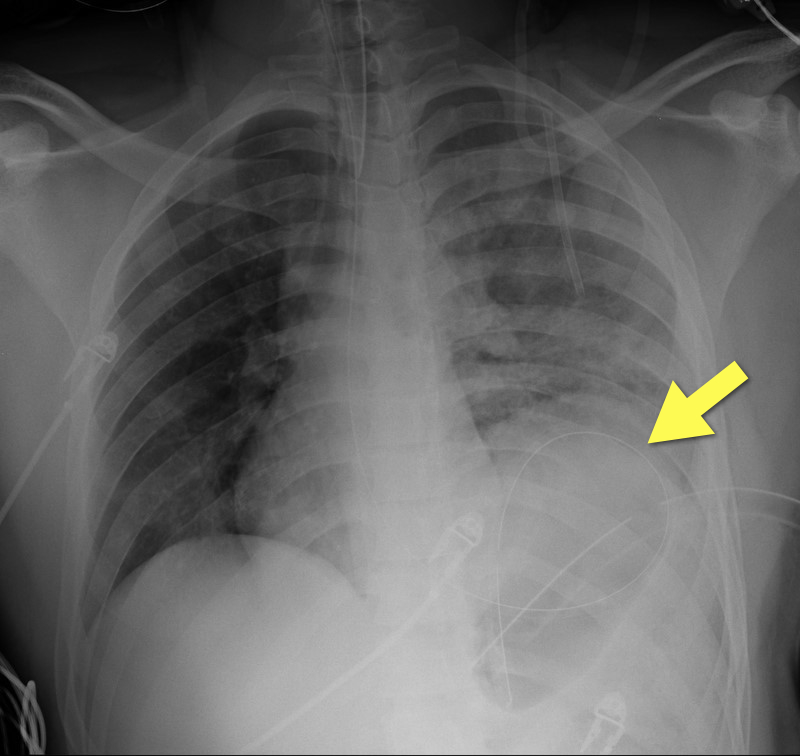
19 year-old male s/p high-speed MVC with hypotension and diminished breath sounds on left. Diagnosis?
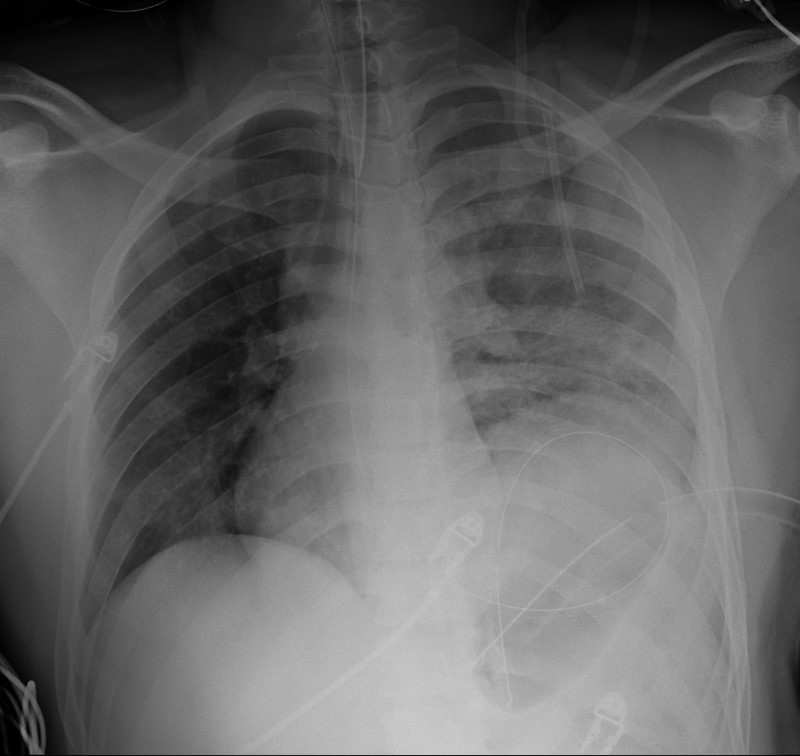
Answer: Diaphragmatic rupture (Note position of NG tube on image below).
·Uncommon; less than 1% of all traumatic injuries
·Diagnosis may be obvious on CXR (as in example) or subtle (e.g., diaphragmatic elevation, basilar atelectasis, etc.)
·Requires a high-index of suspicion because delayed diagnosis increases the risk of abdominal organ herniation or strangulation.
·Mortality depends on the mechanism and presence of associated injuries; mortality is highest for blunt injuries.
Bhavnagri S, et al. When and how to image a suspected broken rib. Cleveland Clinic J Med. 2009;76(5):309.
Williams M, et al. Predictors of mortality in patients with traumatic diaphragmatic rupture and associated thoracic and/or abdominal injuries. Am Surg. 2004;70(2):157.
National Trauma Data Base. American College of Surgeons 2000-2004.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: Procedures, Arterial lines, Axillary, hemodynamic monitoring (PubMed Search)
Posted: 9/13/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Radial and femoral arteries are common sites for arterial-line placement, but are not without complications (e.g., Radial artery: malfunction with positioning and Femoral artery: contamination and infection); an alternative site to consider is the axillary artery.
The axillary artery's superficial location and large size make it a desirable choice for cannulation.
The "anatomical-landmark" and "palpation" methods have been the traditional techniques of axillary arterial cannulation, however these methods may be difficult for to a variety of reasons (e.g., obesity, anasarca, arterial disease, etc.)
Ultrasound allows visualization of the axillary artery and avoids unintended injury to structures in close proximity (e.g., brachial plexus, pleura, axillary vein, etc.); please see figures 1 and 2 in the referenced Sandhu article and http://www.youtube.com/watch?v=Z31YiyV7cNQ.
A recent study (Killu, 2011) found that ultrasound increases success rates when compared to the traditional landmark approach.
Killu, K. et al. Utility of Ultrasound Versus Landmark-Guided Axillary Artery Cannulation for Hemodynamic Monitoring in the Intensive Care Unit. ICU Director; 2011. 2(3), 54–59.
Sandhu, N. The Use of Ultrasound for Axillary Artery Catheterization Through Pectoral Muscles: A New Anterior Approach. Anesthesia and analgesia. 2004; 562–565.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 9/4/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
26 year old male presents s/p basketball dunk. Diagnosis?

Answer: Talar dislocation
Below, a post-reduction Xray, as well as a link to a video demonstrating a few ankle reductions (the video's background music makes all the difference): http://www.youtube.com/watch?v=AzqCsLX1K1E

Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: ultrasound, tracheal intubation, esophageal intubation, critical care, airway (PubMed Search)
Posted: 8/30/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Multiple methods of confirming endotracheal tube placement exist, however quantitative waveform capnography is the most reliable method. Unfortunately this may not be immediately available at all medical centers.
Recent studies demonstrate that bedside ultrasound may assist in the detection of proper endotracheal tube placement.
The T.R.U.E. (Tracheal Rapid Ultrasound Exam) was demonstrated to be 99% sensitive, 94% specific, 99% PPV, and 94% NPV during intubation.
The basic exam involves placing a high-frequency linear-array probe on the anterior neck above the sternal notch and identifying the trachea and esophagus during intubation.
The following video is an example of what you DO NOT want to see during an intubation: http://www.youtube.com/watch?v=LvfThxhQ93A
Chou, H. et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. Jun 2011
Werner SL,et al. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med 2007;49:75–80.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 8/22/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
79 y.o. male lung cancer patient with tachypnea, tachycardia, and normal blood pressure. Click here: http://vimeo.com/27973006
Possible diagnosis?
Answer: Right ventricular (RV) dysfunction secondary to submassive pulmonary embolism (PE).
Ultrasound for suspected PE
Consider bedside echo with PE and elevated troponin or BNP.
Recall the classes of PE:
Ultrasound “clues” of submassive / massive PE:
Lodato JA, Parker Ward RP, Lang RM. Echocardiographic Predictors of Pulmonary Embolism in Patients Referred for Helical CT. Echocardiography 2008;25:584-590.
McConnell MV, Solomon SD, Rayan ME, et. al. Regional Right Ventricular Dysfunction Detected by Echocardiography in Acute Pulmonary Embolism. Am J Cardiol. 1996; 78: 469-473.
ACEP. Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department With Suspected Pulmonary Embolism. http://www.acep.org/content.aspx?id=30060. [July 24, 2011].
John Griffiths. Respiratory: Management of small, submassive and massive pulmonary embolism. http://www.frca.co.uk/article.aspx?articleid=100750. [July 24, 2011].
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: bougie, cricothyrotomy, trauma, critical care, intubation, failed airway (PubMed Search)
Posted: 8/16/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The open cricothyrotomy technique is taught as the trauma airway standard when one “cannot intubate and cannot ventilate” however, it is not without difficulty and limitations. The B.A.C.T. (Bougie-Assisted Cricothyrotomy Technique) may improve the procedure by using a bougie to assist.
Steps for the B.A.C.T. (as described in the paper):
1. Stabilize the larynx with the thumb and middle finger, then identify the cricothyroid membrane.
2. Make a transverse stabbing incision with a scalpel through both skin and cricothyroid membrane.
3. Insert tracheal hook at the inferior margin of the incision and pull up on the trachea.
4. Insert a bougie through the incision with curved tip directed towards the feet
5. Pass 6-0 endotracheal tube or Shiley over bougie into trachea.
Advantages of a bougie:
1. Thin and easy to insert into incision
2. Tactile feedback from tracheal rings confirms proper placement
3. Ensures that stoma will not be lost during procedure
EMRAP.tv has a great video of Dr. Darren Braude demonstrating the procedure;
http://bit.ly/nB3BMG
Hill, C., et al. Cricothyrotomy Technique Using Gum Elastic Bougie Is Faster Than Standard Technique: A Study of Emergency Medicine Residents and Medical Students in an Animal Lab. Academic Emergency Medicine17(6), 666–669.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 8/7/2011 by Haney Mallemat, MD
(Updated: 8/8/2011)
Click here to contact Haney Mallemat, MD
13 year-old right-hand dominant male following assault with blunt object. Diagnosis?
Answer: Monteggia fracture
Monteggia Fracture
Bruce H.E., Harvey J.P., Wilson J.C. Monteggia Fractures. J Bone Joint Surg Am. 1974;56:1563.
Reckling F.W. Unstable fracture-dislocation of the forearm (Monteggia and Galeazzi lesions). J Bone Joint Surg Am. 1982;64:857.
http://emedicine.medscape.com/article/1231438-overview
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: trauma, resuscitaiton, pregnancy, IVC, supine hypoventilation, edema, intubation, RSI, desaturaiton (PubMed Search)
Posted: 8/2/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Pregnancy causes many physiologic changes, which may be challenging during trauma resuscitations. A few pearls on the ABC’s:
Airway
Breathing
Circulation
Chesnutt, A. Physiology of normal pregnancy. Crit Care Clinics 2004 Oct;20(4):609-15.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/25/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
34 y.o. male with history of IVDA (intravenous drug abuse) complains of fever, chills and cough. Diagnosis?
Answer: Lung Abscess (from septic pulmonary emboli)
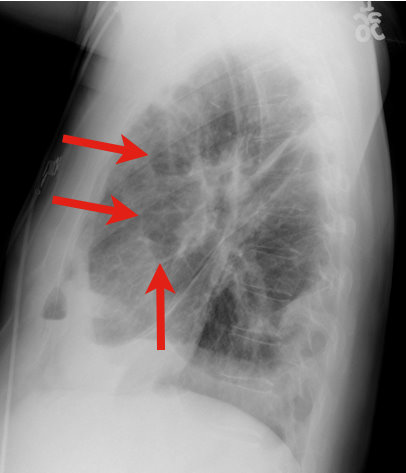
Lung Abscess
Necrosis of lung parenchyma with pus and debris-filled cavities
Caused by direct injury (e.g., aspiration pneumonia) or secondary causes (e.g., tricuspid endocarditis, bacteremia, etc.)
Suspect with:
Loss of airway reflexes (e.g., CVA, seizures, alcohol / narcotic abuse, etc)
Poor dentition
Immunosuppression
IVDA
Gram positives, negatives and anaerobic bacteria have all been implicated.
CXR may suggest diagnosis, but CT scan better identifies abscess, necrotic tissue, empyema, or other pathology (see image below).
After drawing blood cultures, broad-spectrum antibiotics should be started and narrowed once culture data is available; address underlying cause (e.g., valve replacement for endocarditis).
Prognosis is generally good with normal immune function and antibiotics, but mortality sharply increases with immunocompromise and treatment delay.
Mansharamani N, et al. Lung abscess in adults: clinical comparison of immunocompromised to non-immunocompromised patients. Respiratory Medicine. Mar 2002;96(3):178-85
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
