Category: Visual Diagnosis
Posted: 11/19/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Do you like placing ultrasound-guided IV catheters? Check out this trick for covering the probe during the procedure.
http://ultrarounds.com/Ultrarounds/The_Vascular_Probe_Protector.html
or
https://www.youtube.com/watch?v=ZuOq6Ea_FbA&feature=plcp
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/12/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
33 year-old male found unconscious by EMS and complains of right shoulder pain upon waking up in the ED. Diagnosis?
Answer: Posterior shoulder dislocation
Follow me on Twitter (@criticalcarenow) or Google+ (+Haney Mallemat)
Category: Critical Care
Posted: 11/6/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Previous pearls have described the increasing evidence against colloid (e.g., hydroxyethyl starch) use during resuscitation. Now it appears that the crystalloid 0.9% normal saline (NS) may be under fire.
The use of large volumes of NS has been associated with hyperchloremic metabolic acidosis and harm in animal studies. The risk of harm in humans, however, has been less clear.
Bellomo et al. conducted a prospective observational study in which patients being resuscitated in the control group received NS at the clinicians' discretion; i.e., chloride-liberal strategy. The use of NS was restricted in the intervention group, where other less chloride containing fluids were used for resuscitation (e.g., Ringer's Lactate); i.e., a chloride-restrictive strategy.
The authors found that when compared to patients in the chloride-liberal group, the chloride-restrictive group had significantly less rise in baseline creatinine, less overall AKI, and a reduced need for renal replacement therapy.
Bottom line: Although this was only an observational study, the liberal use of normal saline during resuscitation may increase the risk of AKI and renal replacement therapy.
Bellomo, R. et al. Association between a chloride-liberal vs. chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012 Oct 17;308(15):1566-72. doi: 10.1001/jama.2012.13356.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/5/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
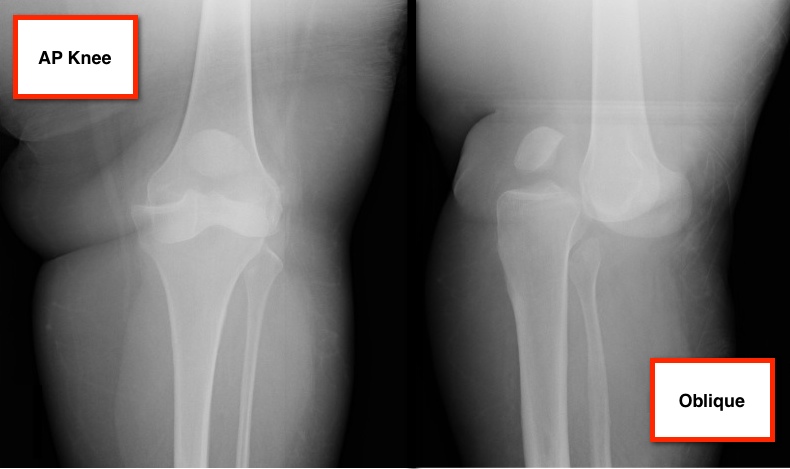
11 year-old male is tackled and falls on his outstretched hand while playing football. X-rays are shown below. What's the diagnosis?
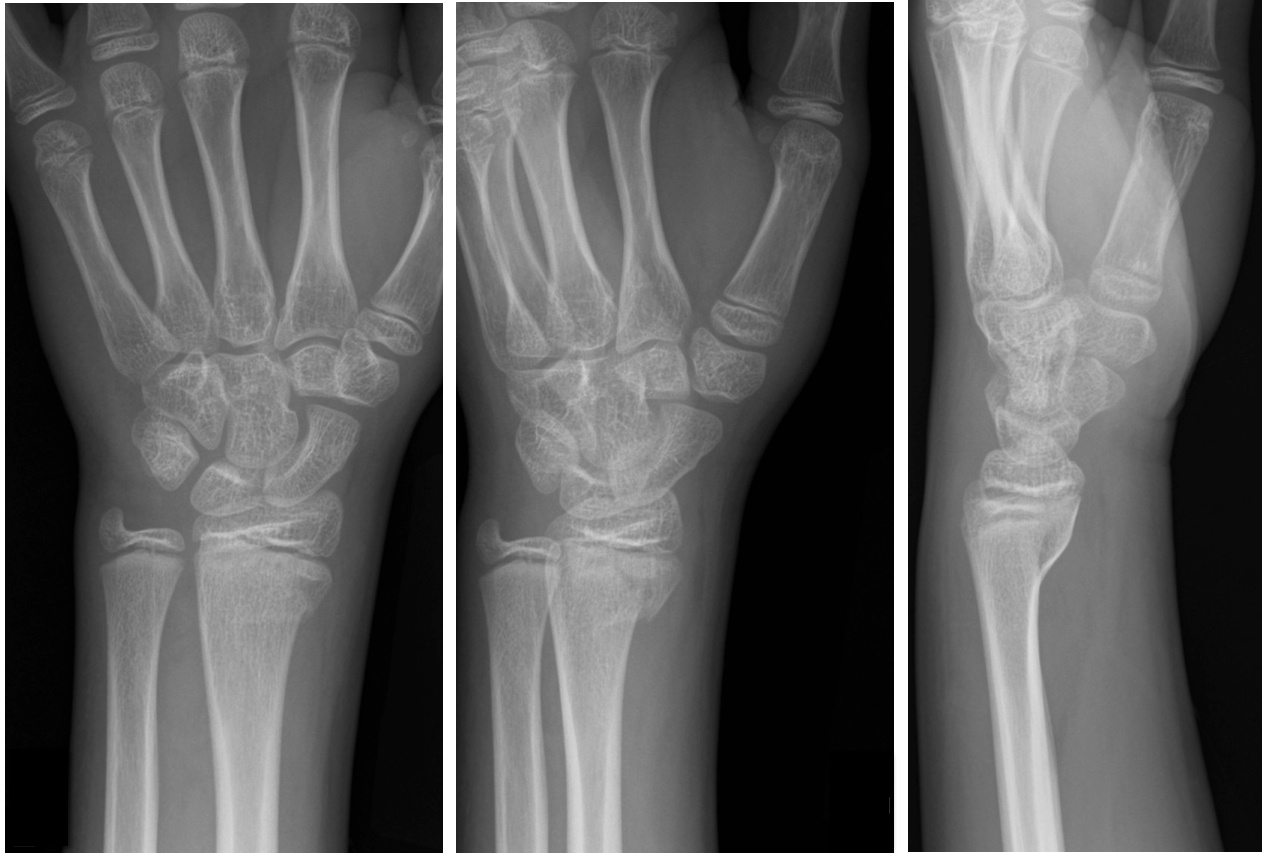
Answer: Salter-Harris Fracture - Type II
Salter-Harris Fracture (SHF)
SHF are fractures through the growth plate (a.k.a. the physis), therefore are unique to pediatric patients.
Fractures are categorized according to involvement of the physis, metaphysis, and epiphysis. Proper injury classification is important because it affects both the treatment and potential long-term complications. Radiographic findings can sometimes be subtle; especially Type 1 SHF.
Occult SHF should be suspected when there is tenderness or swelling over an epiphyseal surface with X-rays negative for fracture. In this case, children should be splinted and urgently followed up.
SHF classification
Bonus Pearl:
Use mnemonic SALTR to remember fracture type (Type I-Slipped, II-Above physis, III-Lower physis, IV-Through physis, V-Rammed)
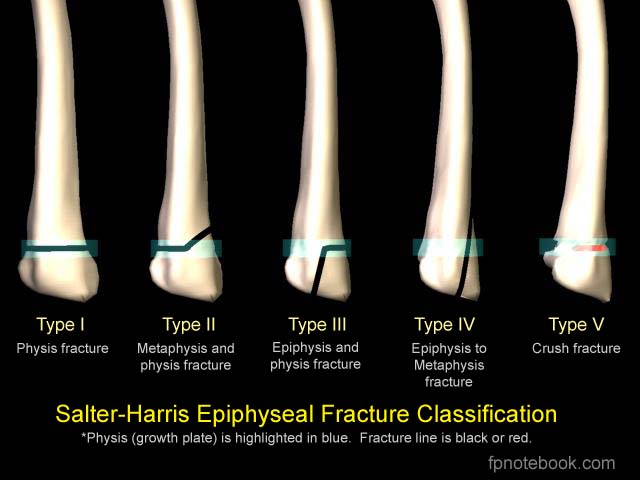
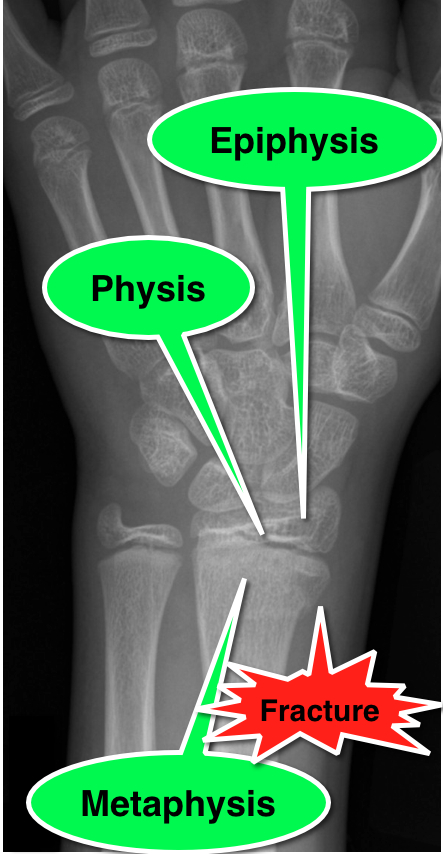
emedicine.medscape.com/article/412956-overview
Salter, R and Harris R. Injuries involving the Epiphyseal Plate. Journal of Bone and Joint Surgery. Vol 45-A. Issue 3, April 1963.
fpnotebook.com/_media/OrthoFractureSalterHarris.jpg
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 10/29/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
33 year-old male in respiratory distress. What's the diagnosis?
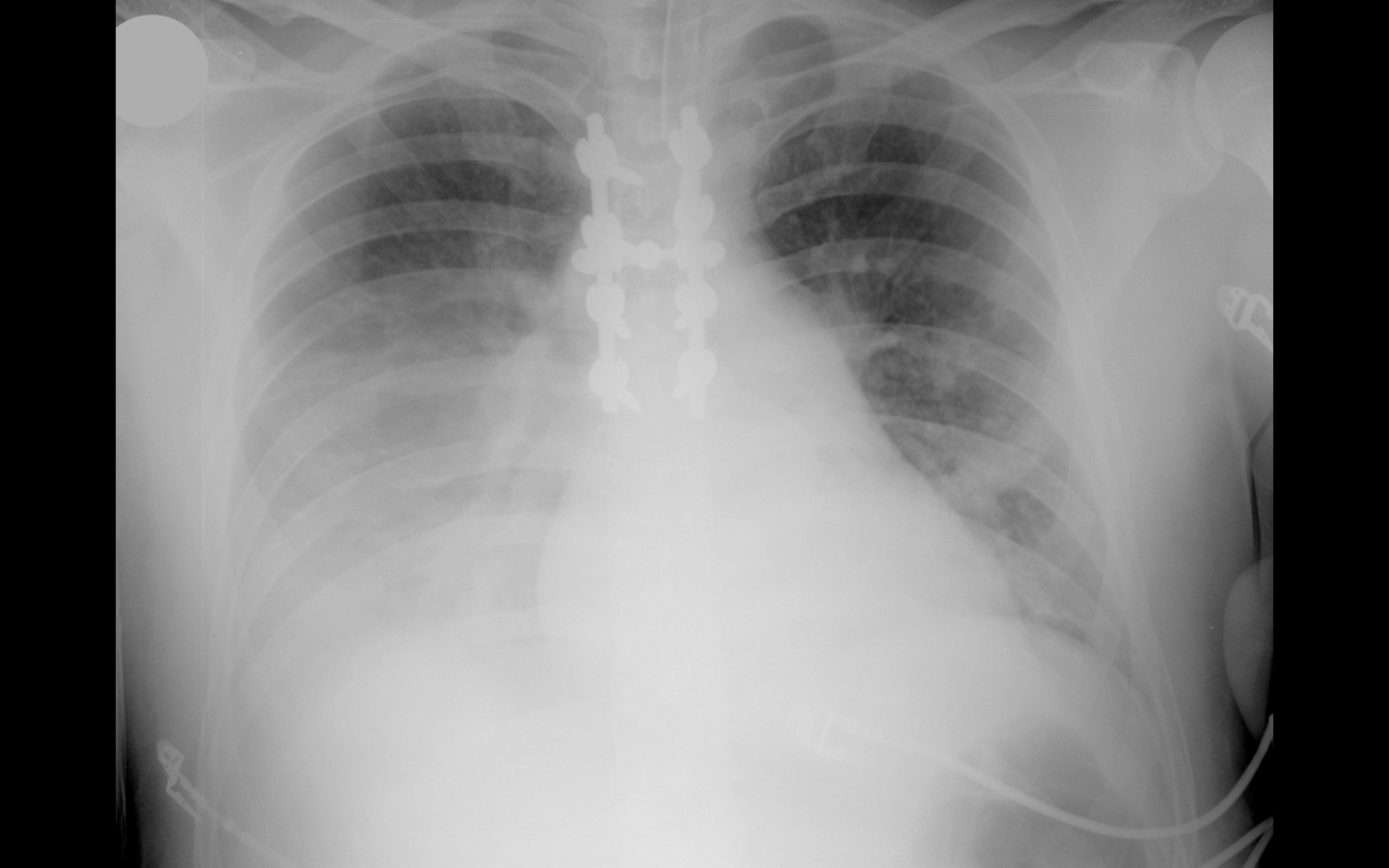
Answer: Click here or here
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 10/22/2012 by Haney Mallemat, MD
(Updated: 10/24/2012)
Click here to contact Haney Mallemat, MD
Perner A., et al. Hydroxyethyl Starch 130/0.4 versus Ringer's Acetate in Severe Sepsis. NEJM. 2012 Jun 27.
Category: Visual Diagnosis
Posted: 10/22/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Trauma patient (...yes, that's the only history you're given). Diagnosis?
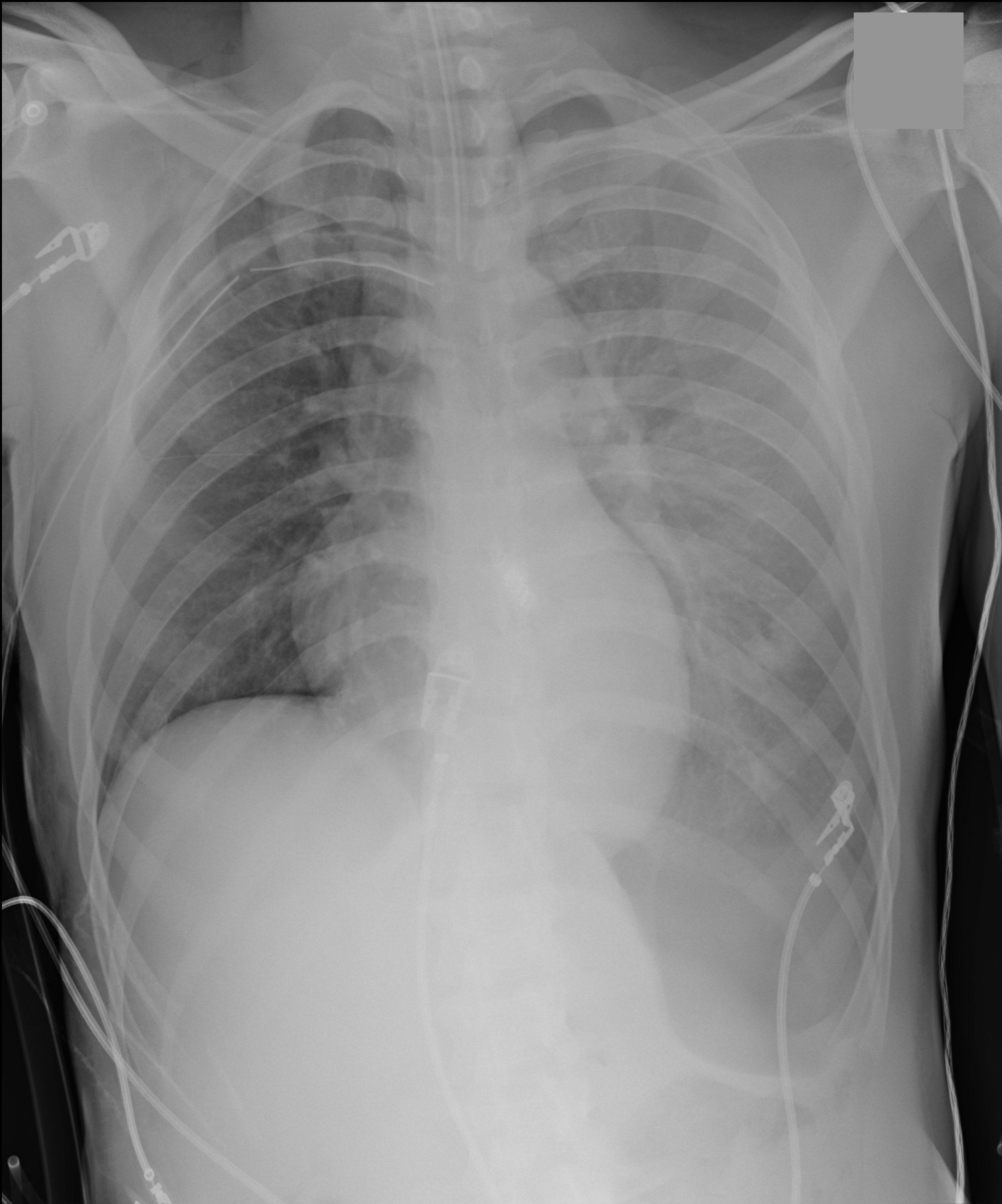
Answer: Inverted left hemidiaphragm (or deep sulcus sign) secondary to a tension pneumothorax. There is also a superimposed hemothorax.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 10/15/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
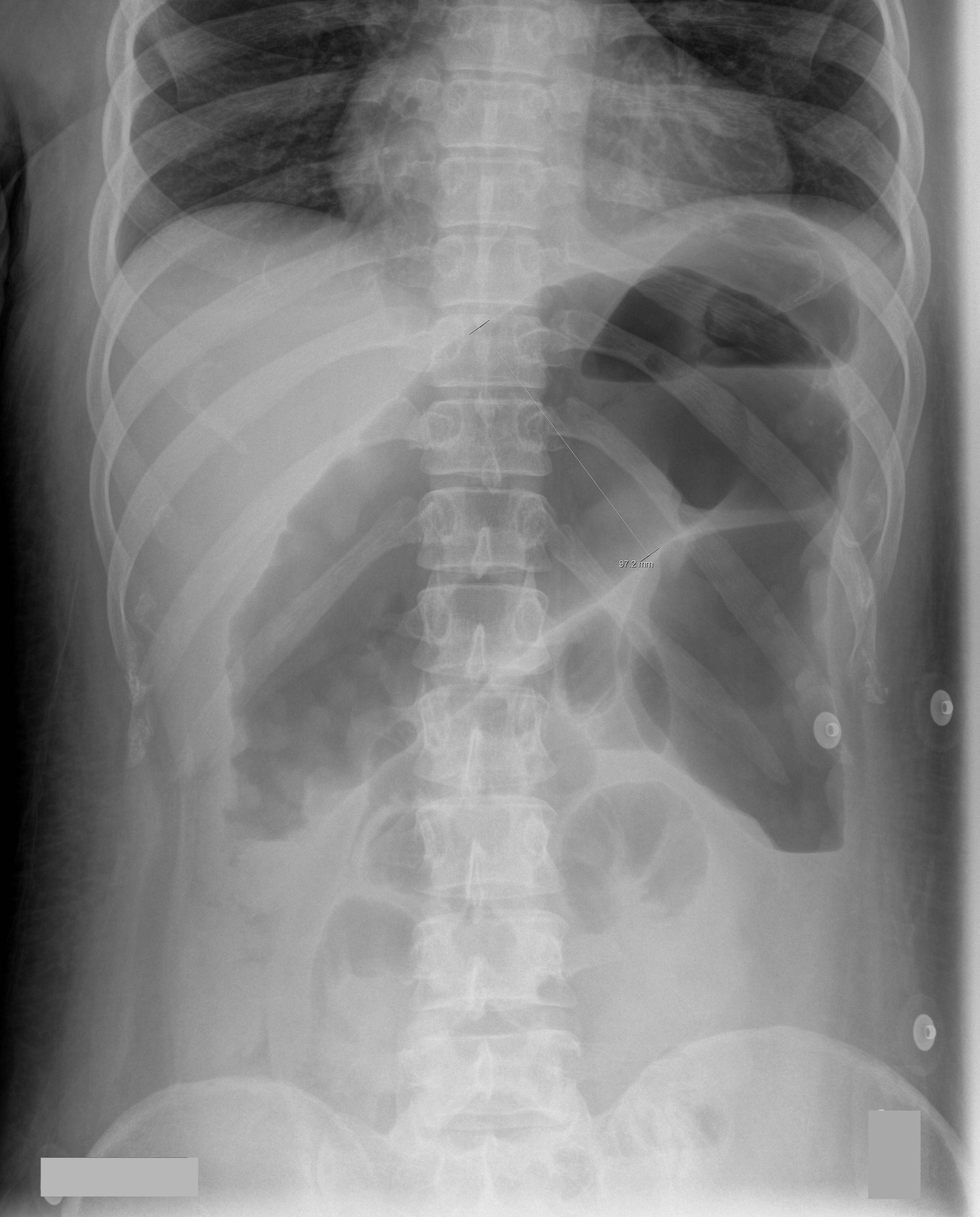
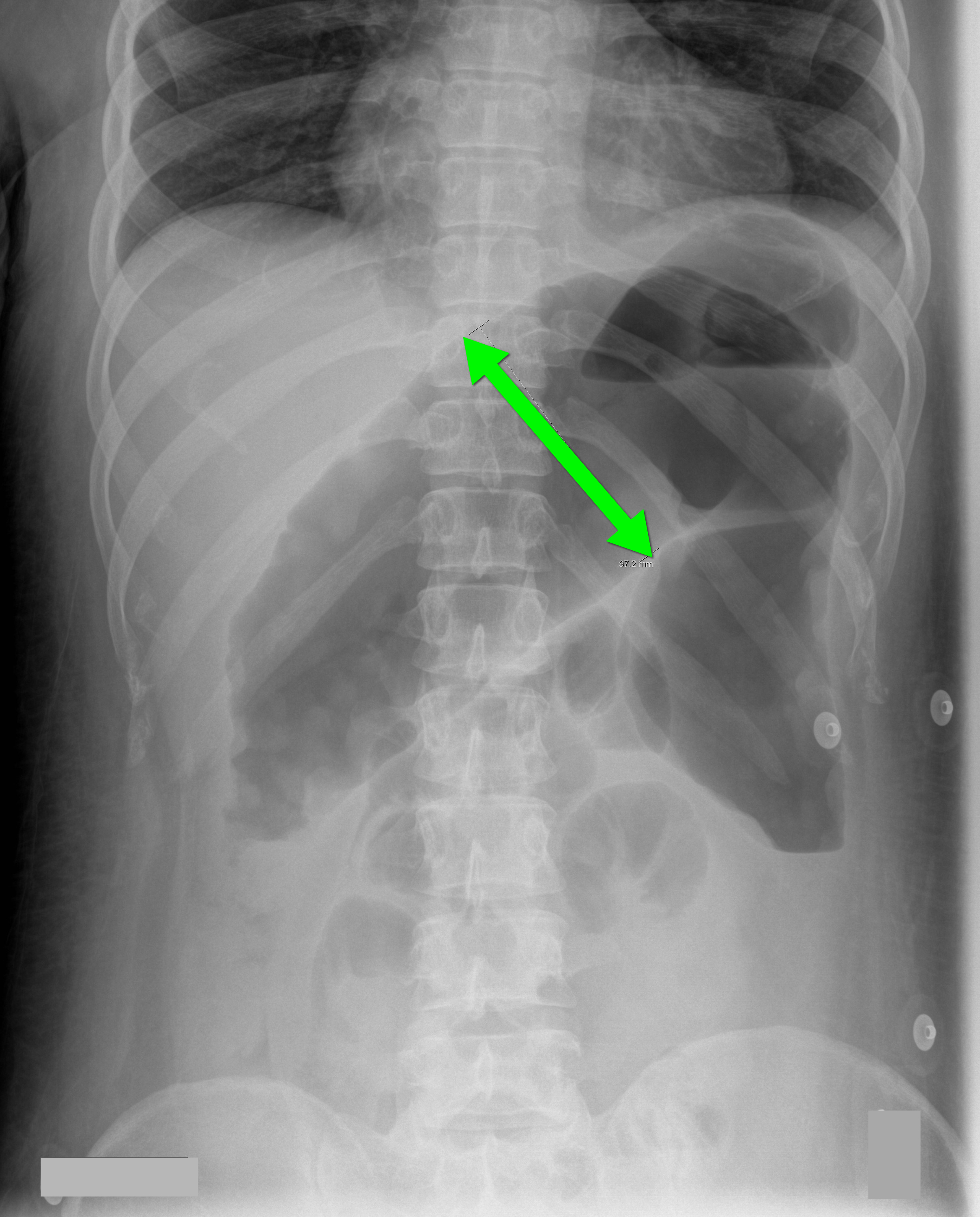
35 year-old male unrestrained driver following motor vehicle crash presents with blunt chest injury. There are multiple injuries on CXR (can you find them all?), but what's up with his right lung?
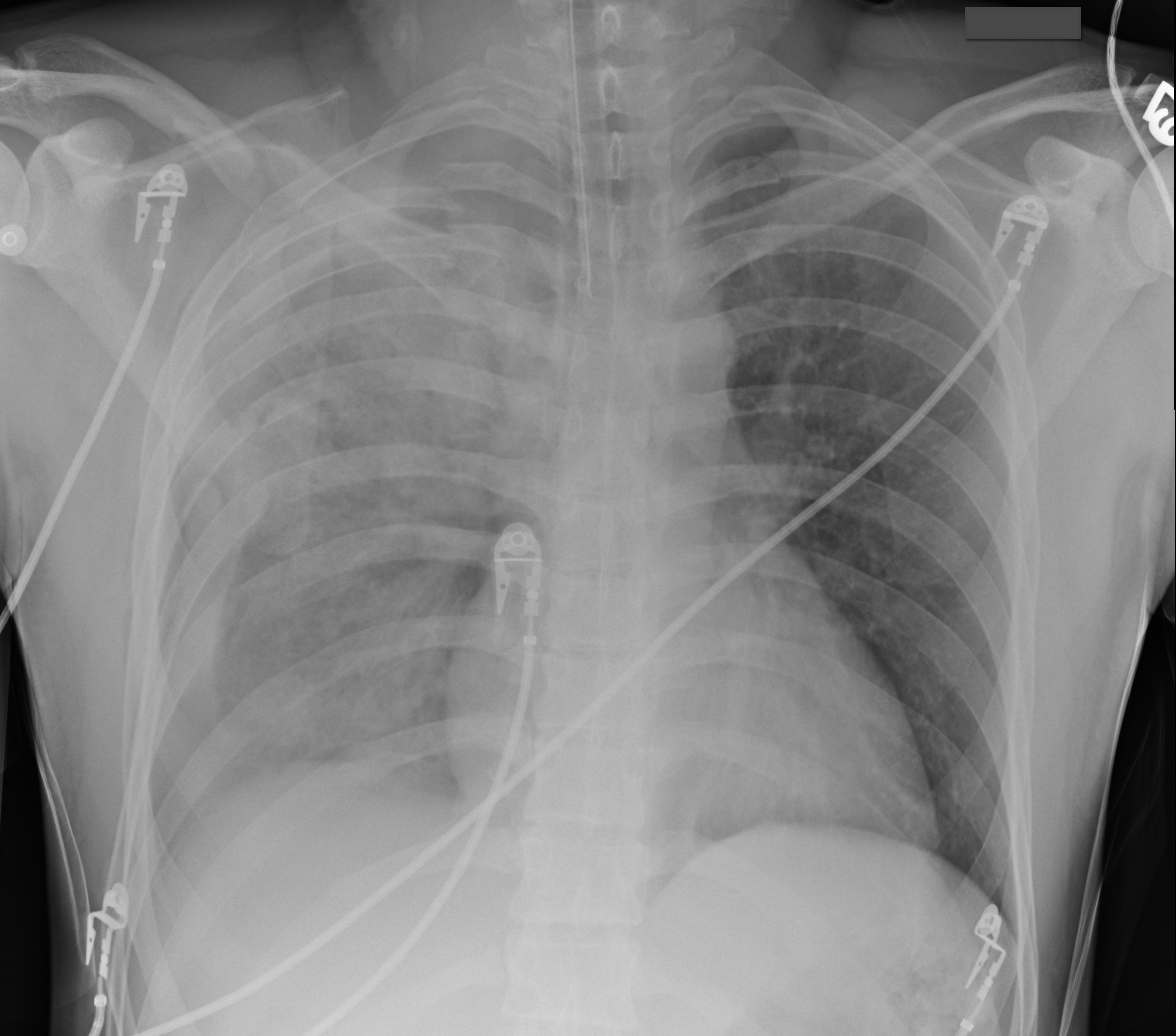
Answer: Pulmonary contusion
Blunt chest trauma may result in pulmonary contusion, a parenchymal lung injury resulting in blood and edema within the alveolar spaces.
The pathophysiologic effects result in reduced lung compliance and gas exchange (i.e., dead space ventilation and/or shunting), increased risk of ARDS, and increased pulmonary vascular resistance. The full pathophysiologic effects may take up to 48 hours to develop. Resolution usually occurs within 3-5 days.
Diagnosis is typically made on CXR, although early CXR may underestimate the severity of injury. CT scan is much more sensitive for diagnosis (see green arrows below).
Management is supportive and requires strict attention to oxygenation. Positive pressure ventilation is occasionally required for respiratory failure and is sometimes recommended prophylactically for elderly patients, because their pulmonary status can rapidly decline secondary to their reduced lung reserve.
Aggressive control of chest wall pain is also required. Pain reduces both the frequency and depth of respirations leading to atelectasis, a reduction in mucus clearance, and an increased risk of pneumonia. Analgesia should be administered systemically, by epidural, or by local nerve block at the level of injury.

Lively, M. Pulmonary contusion in a collegiate diver: a case report. J Med Case Rep. 2011 Aug 10;5:362.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 10/9/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
70 year-old male recently treated for community-acquired pneumonia presents with bloody diarrhea, fever, and severe abdominal pain. Abdominal Xray is shown below. Diagnosis?
Answer: Toxic Megacolon
Toxic megacolon (TM) is an acute colitis with segmental or total colonic dilation (>6cm) plus systemic toxicity.
Actual incidence is unknown, but it is believed that TM is rising because of increasing cases of Clostridium difficile and the aging population.
The most common etiologies are ulcerative, chron, and pseudomembranous colitis, but other causes exist and can be categorized as:
The diagnosis is made based on clinical evidence of colitis plus evidence of colonic dilation on abdominal XR (diameter > 6cm, loss of haustra, or free intraperitoneal air secondary to perforation) or CT scan (demonstrating dilation or perforation).
Treatment includes:
Autenrieth, D et al. Toxic Megacolon Inflammatory Bowel Dis. 2011 Aug 29.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 10/7/2012 by Haney Mallemat, MD
(Updated: 10/8/2012)
Click here to contact Haney Mallemat, MD
26 year-old male from Indonesia presents with severe abdominal pain and weight loss for the past two months. He also states he found this "worm" in the toilet (see below) after a bowel movement. What is the medical treatment for this condition?
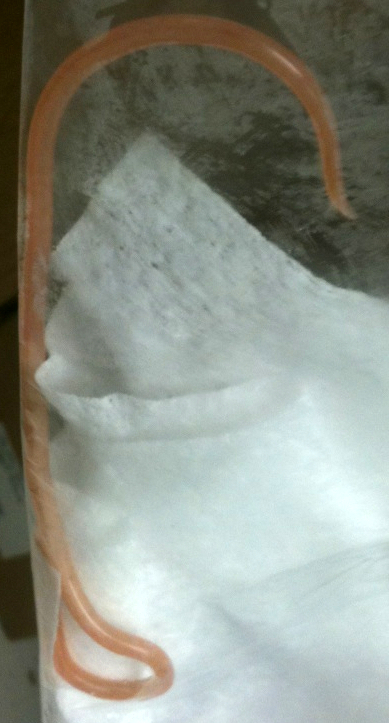
Answer: Mebendazole or albendazole
The image above shows an Ascaris Lumbricoides (AL), the most common intestinal roundworm infection in humans. It typically occurs in inhabitants of impoverished areas with poor sanitation.
Humans acquire AL from ingesting eggs from infected food or soil. Eggs hatch into larvae within the small intestine and then migrate through the mucosa to vascular beds of the alveoli within the lung. Larvae then migrate up the respiratory tree and are swallowed into the GI tract where they mate and more eggs are laid, maturing here or migrating to other organs within the body.
Most infections are asymptomatic, but signs and symptoms can range from nonspecific pulmonary (first two weeks secondary to larval migration into lungs) to severe (after six weeks secondary to the mechanical effects of high parasite load in the gut). Symptoms include:
Treatment during early infection is challenging because AL is non-specific and difficult to diagnose; symptomatic and supportive care is required. When the diagnosis is made, medications such as mebendazole and albendazole can be used to eradicate AL directly within the gut. Situations where worms cause intestinal obstruction, require manual debulking using scopes (e.g., colonoscopy) or surgery.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 10/1/2012 by Haney Mallemat, MD
(Updated: 10/2/2012)
Click here to contact Haney Mallemat, MD
Do you place central-lines?
Do you suture your central-lines into place?
Do you ever get worried that you are going to stick yourself with that needle?
If you answered yes to any of these questions, then maybe this pearl is for you; click here
Follow me on Twitter (@criticalcarenow) or on Google+ (+haney mallemat)
Category: Critical Care
Posted: 9/25/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Intubated patients may occasionally meet certain criteria for extubation while in the Emergency Department. Extubation is not without its risk, however, as up to 30% of patients have respiratory distress secondary to laryngeal and upper airway edema, with some patients requiring re-intubation.
Prior to extubation, Intensivists use a brief “cuff-leak” test (deflation of the endotracheal balloon to assess the presence or absence of an air-leak around the tube) to indirectly screen for the presence of upper airway edema and ultimately the risk of re-intubation. The cuff-leak test is performed by deflating the endotracheal balloon followed by one or more of the following maneuvers:
Ochoa et al. performed a systematic review to determine the accuracy of the “cuff-leak” test to predict upper airway edema prior to extubation. The authors concluded that a positive cuff-leak test (i.e., absence of an air-leak) indicates an elevated risk of upper airway obstruction and re-intubation. A negative cuff-leak test (i.e., presence of an air-leak), however, does not reliably exclude the presence of upper airway edema or the need for subsequent re-intubation.
Bottom line: No test prior to extubation reliably predicts the absence of upper airway edema. Patients extubated in the Emergency Department require close observation with airway equipment located nearby.
Ochoa, ME et al. Cuff-leak test for the diagnosis of upper airway obstruction in adults: A systematic review and meta-analysis. Intensive Care Med (2009) 35:1171–1179
Follow me on Twitter @criticalcarenow or Google+ (+Haney Mallemat)
Category: Visual Diagnosis
Posted: 9/24/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Guide-wires can be challenging to dispose of after central-line insertion because they are difficult to keep on the field, hard to place in the sharps box, and can splash nearby observers.
Click here for this little guide-wire disposal trick.
Follow me on Twitter @criticalcarenow or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 9/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
27 year-old woman with AIDS presents complaining of a painful, puritic, and papular rash. What's the diagnosis?

Answer: Herpes zoster ophthalmicus
Herpes Zoster Ophthalmicus
Follow me on Twitter (@criticalcarenow) or on Google+ (+haney mallemat)
Category: Critical Care
Posted: 9/11/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
40 year-old male with severe uncontrolled hypertension presents with altered mental status (head CT below). The CXR is from the same patient. What's the connection?
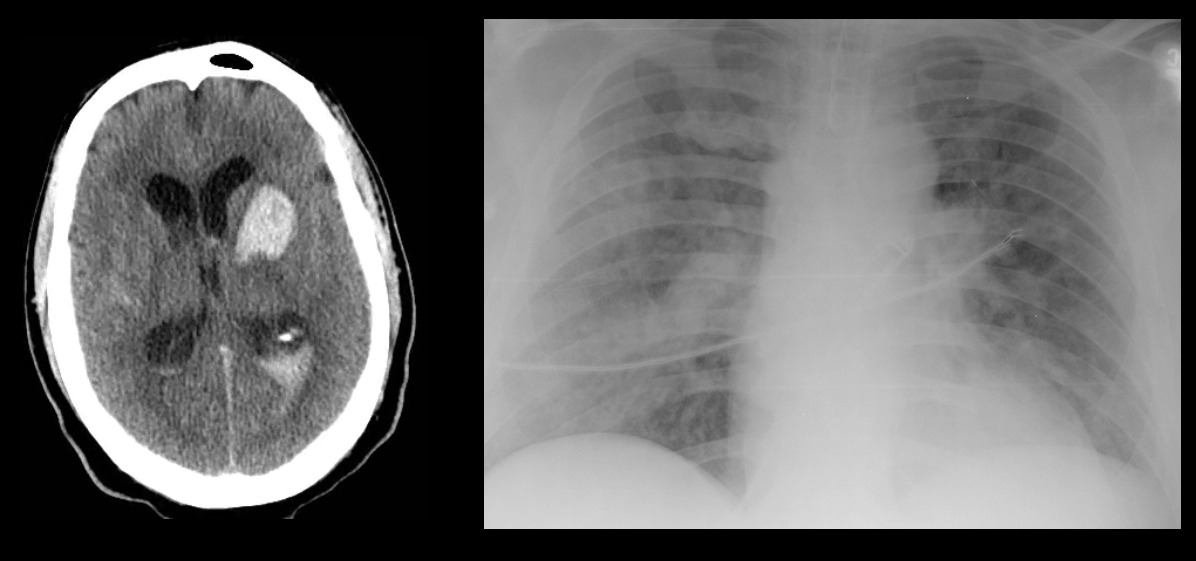
Answer: Neurogenic pulmonary edema (NPE)
NPE is defined as acute pulmonary edema following central nervous system (CNS) insult; NPE has been recognized for over 100 years, but its incidence is underreported due to a lack objective clinical criteria.
The pathophysiology of NPE is poorly understood but it is generally believed that both cardiogenic and non-cardiogenic pulmonary edema play a role. CXR (see above) demonstrates a pattern similar to acute respiratory distress syndrome (i.e., bilateral interstitial infiltrates).
CNS insults that are abrupt, rapidly progressive, and increase intracranial pressure (e.g., subarachnoid hemorrhage, intraparenchymal hemorrhage, traumatic brain injury, subdural, etc.) have the highest risk for NPE. Neural injury leads to sympathetic activation, the release of catecholamines, and one or all of the following:
Treatment of NPE includes:
Davidson, D. et al. Neurogenic pulmonary edema. Crit Care. 2012 Mar 20;16(2):212.
Follow me on Twitter (@criticalcarenow) and Google+ (+haneymallemat)
Category: Visual Diagnosis
Posted: 9/10/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
40 year-old male with severe uncontrolled hypertension presents with altered mental status. Head CT is shown here. Name three common anatomic locations generally seen for non-traumatic intracerebral hemorrhage.
Answer: The most common anatomic sites for intra-cerebral hemorrhage are:
...and, don't forget the most common causes of non-traumatic intra-cerebral hemorrhage:
Follow me on Twitter (@criticalcarenow) and Google+ (+haneymallemat)
Category: Visual Diagnosis
Posted: 9/3/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
32 year-old female presents with 5 days of fever, chills, and flank pain. She is hypotensive on presentation and urinalysis shows pyuria. Click here for the non-contrast CT scan. What's the diagnosis and what type of antibiotics should be started empirically?
Answer: Staghorn caliculi secondary to struvite stone. Broad-spectrum antibiotics to cover anaerobic bacteria should be initiated.
Follow me on Twitter (@criticalcarenow) and Google+ (+haneymallemat)
Category: Critical Care
Posted: 8/28/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A Cochrane review of 37 studies concluded that Succinylcholine (SUC) is superior to Rocuronium (ROC) during rapid sequence intubation.
The authors claim that compared to ROC, SUC has a faster onset of action (45 vs. 60 seconds) and overall a shorter duration of action (10 vs. 60 minutes).
Dr. Reuben Strayer wrote a letter to the journal editors and stated that these findings should be interpreted carefully; he highlighted that most of the studies in the review used doses of ROC less than 0.9 mg/kg (most studies used 0.6mg/kg).
Dr. Strayer asserted that ROC’s onset of action is dose dependent; when using doses of 1.2 mg/kg, ROC’s onset is indistinguishable from that of SUC. He also stated another major benefit of ROC is the lack of adverse effects that SUC possesses (hyperkalemia and malignant hyperthermia).
What are your thoughts on this? Go to http://www.facebook.com/Criticalcarenow and take the poll (there are 5 choices). Results will be posted next week.
Seupaul RA, Jones JH. Evidence-based emergency medicine. Does succinylcholine maximize intubating conditions better than rocuronium for rapid sequence intubation? Ann Emerg Med. 2011 Mar;57(3):301-2. Epub 2010 Nov 18.
Strayer RJ. Rocuronium versus succinylcholine: Cochrane synopsis reconsidered. Ann Emerg Med. 2011 Aug;58(2):217-8.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 8/27/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
56 year-old male presents with chest pain. You perform an ultrasound of the heart and see the clip below. What's the diagnosis? Thanks to Dr. Ken Butler for the case.
Answer: Type A Dissection
Click here for an explanation.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 8/20/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
36 year-old female presents with left knee-pain following a motor vehicle crash (XRs are shown). What's the diagnosis AND what is the first test that should be performed to assess for vascular injury?
Answer: Anterior knee-dislocation and Ankle-Brachial Index (ABI)
Both anterior and posterior knee-dislocations have the potential for popliteal arterial injury.
ABI compares Doppler pressures of arms to legs to screen for lower limb ischemia (click here to learn more ABIs). ABIs can be used to accurately predict whether patients with knee dislocations have sustained vascular injury.
A prospective study by Mills et al. demonstrated the sensitivity, specificity, and positive predictive values of an ABI lower than 0.90 were 100% for arterial injury, requiring surgical treatment.
Conversely, the negative predictive value of an ABI that was 0.90 or higher was 100%, suggesting no further workup is required.
Mills W, Barei D, McNair P. The Value of the Ankle-Brachial Index for Diagnosing Arterial Injury After Knee Dislocation: A Prospective Study. Journal of Trauma-Injury Infection & Critical Care: June 2004 - Volume 56 - Issue 6 - pp 1261-1265.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
