Category: Trauma
Keywords: Trauma, blood, Txa, prehospital (PubMed Search)
Posted: 11/10/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this small retrospective study comparing outcomes before and after a prehospital blood administration protocol for penetrating trauma was initiated, the authors found improved survival in those receiving prehospital blood despite a five minute longer on scene time in those receiving blood. Also note TXA was part of the blood protocol but not the control group.
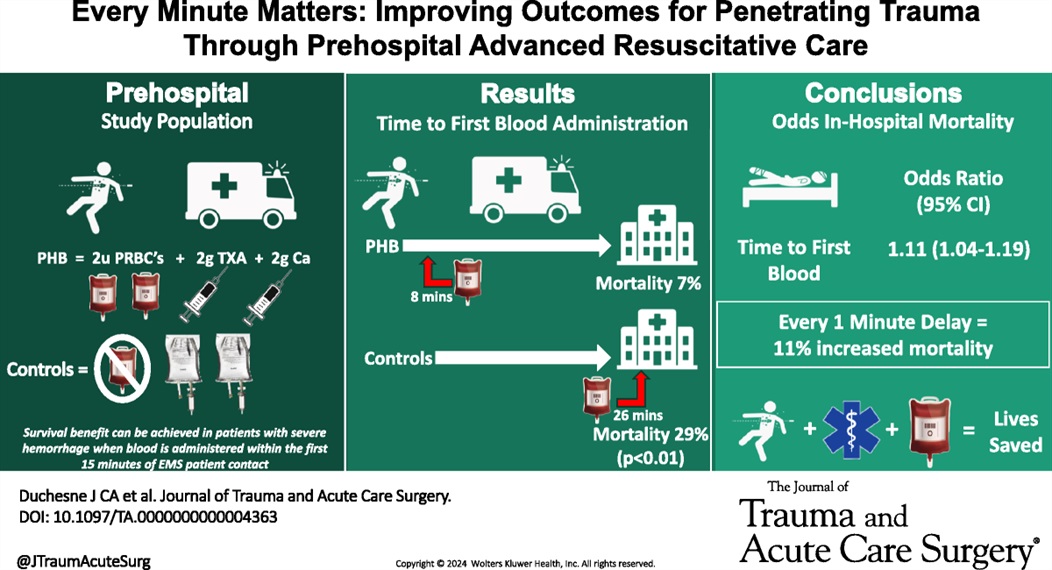
Duchesne, Juan MD; McLafferty, Bryant J. BS; Broome, Jacob M. MD; Caputo, Sydney BS; Ritondale, Joseph P. BS; Tatum, Danielle PhD; Taghavi, Sharven MD, MPH; Jackson-Weaver, Olan PhD; Tran, Sherman MS; McGrew, Patrick MD; Harrell, Kevin N. MD; Smith, Alison MD, PhD; Nichols, Emily MD; Dransfield, Thomas NRP; Marino, Megan MD; Piehl, Mark MD, MPH
Journal of Trauma and Acute Care Surgery 97(5):p 710-715, November 2024. | DOI: 10.1097/TA.0000000000004363
Category: Trauma
Keywords: Repeat, gun violence, Black, revictimization (PubMed Search)
Posted: 11/2/2024 by Robert Flint, MD
(Updated: 11/3/2024)
Click here to contact Robert Flint, MD
This study used the New York State hospital discharge database to look for factors associated with being the victim of repeat gun violence.
Unanswered questions include: is it similar in other areas, what interventions at the patient level could prevent this, what other patient level factors (substance use, etc) are involved, however, this is a good start in looking at this preventable disease.
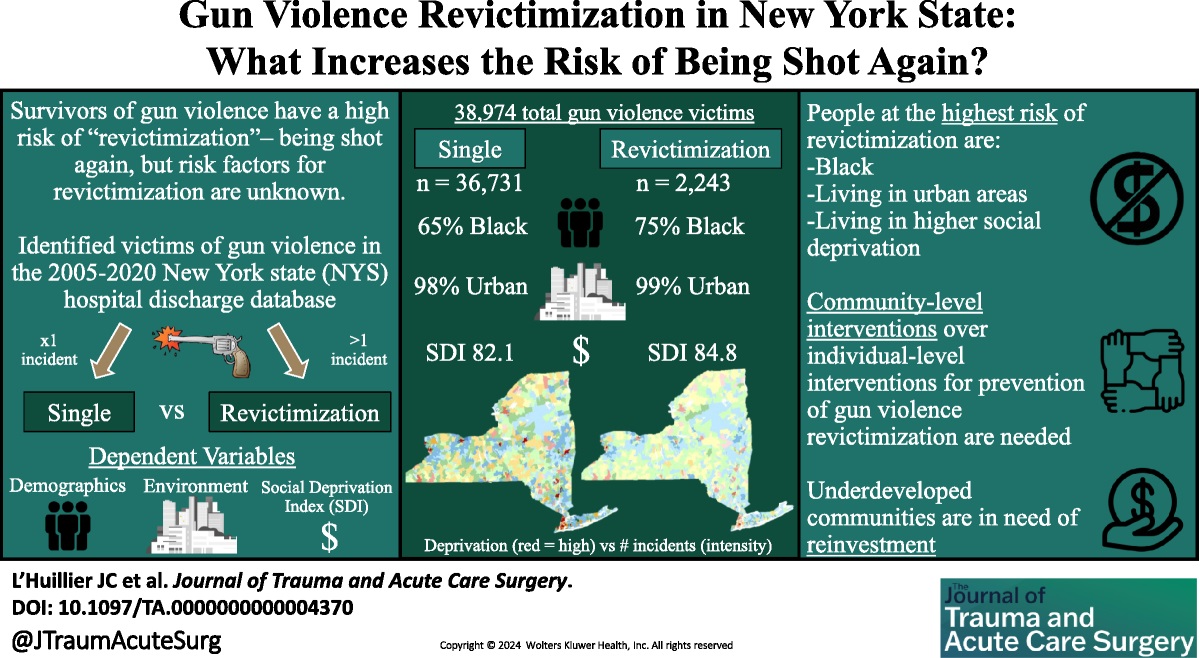
L’Huillier, Joseph C. MD; Boccardo, Joseph D. MS; Stewart, Morgan MUP; Wang, Suiyuan MS; Myneni, Ajay A. MBBS, PhD, MPH; Bari, ASM Abdul MUP; Nitsche, Lindsay J. BS; Taylor, Henry L. Jr PhD; Lukan, James MD, FACS; Noyes, Katia PhD, MPH
Journal of Trauma and Acute Care Surgery 97(4):p 604-613, October 2024. | DOI: 10.1097/TA.0000000000004370
Category: Trauma
Keywords: Adolescent, screening, alcohol, substance use (PubMed Search)
Posted: 11/2/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Recent studies continue to highlight that Black, Native American, female, uninsured and Medicaid patients receive disproportionately more substance use screening when they are trauma patients. The authors of this paper point out that this inappropriate application of screening leads to missed opportunities.
“Screening patients for drug and alcohol use following injury is an evidence-based practice that can trigger wraparound care, such as brief substance use interventions, to prevent reinjury. Adolescents who consume alcohol but are not screened for alcohol use have 2- to 3- fold greater likelihood of reinjury compared with those who were screened and received a brief intervention.”
Sanchez JE, Stey AM. Persistent Inequity Plaguing Pediatric Trauma—An Opportunity for Health Equity Framework. _JAMA Netw Open._2024;7(10):e2436308. doi:10.1001/jamanetworkopen.2024.36308
Category: Cardiology
Keywords: Hypertension, emergency, asymptomatic (PubMed Search)
Posted: 10/30/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Hypertension in the ED comes in two varieties: emergency and asymptomatic (not urgency!). From this position statement: “Hypertensive emergency involves acute target-organ damage and should be treated swiftly, usually with intravenous antihypertensive medications, in a closely monitored setting.”
Conversely, asymptomatic does not require urgent, aggressive management. “Recent observational studies have suggested potential harms associated with treating asymptomatic elevated inpatient BP, which brings current practice into question.”
Without target organ involvement, we do not need to be initiating IV medications or trying to treat the numbers
Bress AP, Anderson TS, Flack JM, Ghazi L, Hall ME, Laffer CL, Still CH, Taler SJ, Zachrison KS, Chang TI; American Heart Association Council on Hypertension; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. The Management of Elevated Blood Pressure in the Acute Care Setting: A Scientific Statement From the American Heart Association. Hypertension. 2024 Aug;81(8):e94-e106. doi: 10.1161/HYP.0000000000000238. Epub 2024 May 28. PMID: 38804130.
Category: Trauma
Keywords: Cryopercipitate, mass transfusion hemorrhage (PubMed Search)
Posted: 10/27/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
There is uncertainty if adding cryopercipitate empirically to all mass hemorrhage protocols has any benefit to mortality, need for transfusion, or any other meaningful outcome. This small study suggests it does not and that we should save the addition of cryopercipitate to those with lab proven low fibrinogen levels.
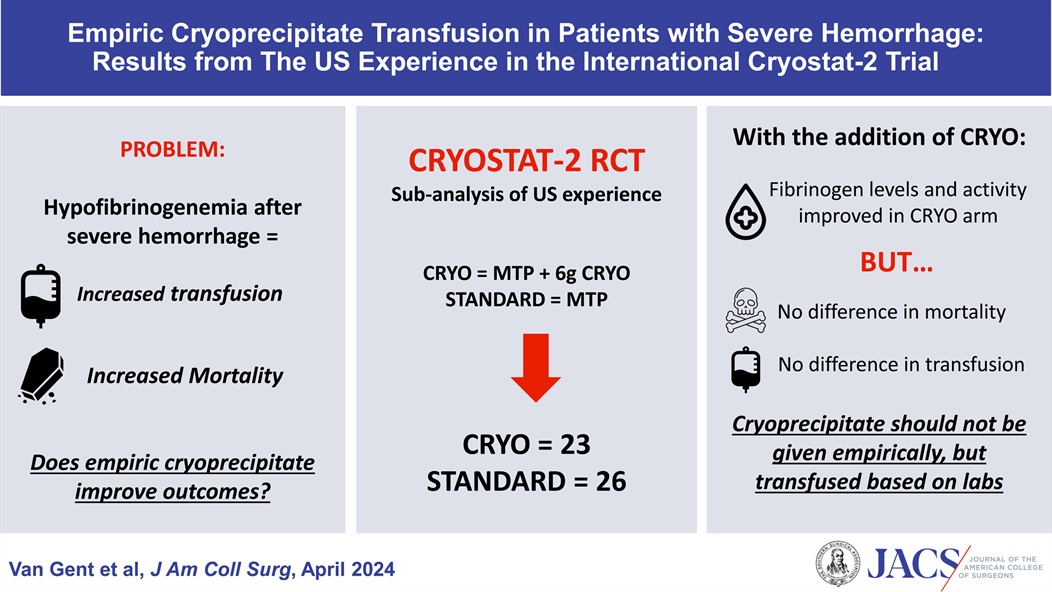
Van Gent, Jan-Michael DO, FACS; Kaminski, Carter W DO; Praestholm, Caroline BS; Pivalizza, Evan G MD; Clements, Thomas W MD; Kao, Lillian S MD, MS, FACS; Stanworth, Simon MD; Brohi, Karim MD; Cotton, Bryan A MD, MPH, FACS
Journal of the American College of Surgeons 238(4):p 636-643, April 2024. | DOI: 10.1097/XCS.0000000000000938
Category: Trauma
Keywords: Neck trauma (PubMed Search)
Posted: 10/24/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
For penetrating neck trauma:
Does it violate the platysma if no, close wound and discharge
If yes, are there any hard signs of injury like enlarging hematoma, air from the wound, difficulty swallowing, blood in the airway, respiratory distress then to the OR
If no, Ct angio of the neck. If negative and no other findings admit for observation or discharge. If positive, to the OR. If equivocal, endoscopy and broncoscopy.
No longer think about the zones of the neck. Treat them all the same.

Category: Trauma
Keywords: Trauma, adrenal crisis, steroids, refractory hypotension. (PubMed Search)
Posted: 10/20/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This article serves as a reminder that trauma can and will precipitate adrenal insufficiency and crisis in those trauma patients who are on steroids pre-injury. Look for prednisone or hydrocortisone as well as autoimmune or rheumatologic diseases on pre-injury medication list and history. Consider the diagnosis in trauma patients with refractory hypotension not responsive to vasopressors. Replacement therapy with hydrocortisone is the therapy.
Volume 62, Issue 6, November–December 2005, Pages 633-637
Brian R. Beeman MD ?, Thomas J. Veverka MD †, Phillip Lambert MD ‡, Dennis M. Boysen Md
Category: Trauma
Keywords: Rectal injury (PubMed Search)
Posted: 10/17/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Rectal injuries are rare and are usually associated with penetrating trauma or significant pelvic fracture from blunt injury. Diagnosis starts with physical exam including inspection for signs of trauma as well as a digital rectal exam looking for blood, bony protuberance and abnormal sphincter tone. Normal digital rectal exam does not exclude injury.
Imagining is important in making the diagnosis.
“Findings on CT associated with rectal injury include a wound tract extending to the rectum, a full-thickness wall defect, perirectal fat stranding, extraluminal free air, intraperitoneal free fluid, and hemorrhage within the bowel wall….A CT with any suggestion of rectal injury should therefore be followed up with rigid proctoscopy to confirm the diagnosis and location of injury, as a combination of CT and endoscopy has a sensitivity of 97% in the diagnosis of rectal injury.”
Fields, Adam MD, MPH; Salim, Ali MD, FACS
Journal of Trauma and Acute Care Surgery 97(4):p 497-504, October 2024. | DOI: 10.1097/TA.0000000000004352
Category: Trauma
Keywords: Rectal injury trauma (PubMed Search)
Posted: 10/13/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Rectal injuries are rare. The majority are secondary to penetrating injuries. Trauma care providers “should have a high clinical suspicion of rectal injury with any missile with a trajectory near the rectum; transpelvic gunshot wounds; stab injuries near the perineum, buttocks, groin, or proximal thighs; or open pelvic fractures. A digital rectal examination with a focus on sphincter tone, presence of blood, palpable defect, or bony protrusion should be carried out. Of note, a normal digital rectal examination does not exclude rectal injury.”
Ct scan with IV contrast (not PO or rectal) is used to identify rectal injuries but will be diagnostic in only 33% of injuries.
Rectal Injury Grading Scale
| Grade | Injury Type | Description of Injury |
|---|---|---|
| I | Hematoma laceration | Hematoma or hematoma without devascularization Partial-thickness laceration |
| II | Laceration | Laceration <50% of circumference |
| III | Laceration | Laceration ?50% of circumference |
| IV | Laceration | Full-thickness laceration with extension into perineum |
| V | Vascular | Devascularized segment |
Fields, Adam MD, MPH; Salim, Ali MD, FACS
Journal of Trauma and Acute Care Surgery 97(4):p 497-504, October 2024. | DOI: 10.1097/TA.0000000000004352
Category: Trauma
Keywords: chest tube, hemothorax, pigtail (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/7/2024)
Click here to contact Robert Flint, MD
The authors reviewed the literature surrounding use of pigtail catheters for traumatic hemothorax and found:
“these data support using percutaneous thoracostomy as a safe and reliable treatment option for hemodynamically stable adult patients with traumatic hemothorax and are backed by major trauma society guidelines including the Eastern Society for the Surgery of Trauma and the Western Trauma Association.1,3 It has the added benefit of the insertion being less painful with the understanding that the percutaneous thoracostomy can always be upsized to a thoracostomy tube.”
Owodunni, Oluwafemi P.Moore, Sarah A.Hynes, Allyson M. et al.
Annals of Emergency Medicine, Volume 0, Issue 0
Category: Trauma
Keywords: Pigtail (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/6/2024)
Click here to contact Robert Flint, MD
Emergency Medicine Cases offers these excellent tips on pigtail catheters placement. Their video/website is worth a look.
PEARL # 1 – LOCATION/LANDMARK: Minimize skin to pleural distance.
PEARL # 2 – ADEQUATE LOCAL ANESTHESIA: This can obviate the need for sedation.
PEARL #3 – DILATING: Do it in a controlled manner.
PEARL #4 – USING THE OBTURATOR: Needless to say, it is there for a reason.
PEARL #5 – INTERPLEURAL BLOCK: Provide your patient with ongoing analgesia.
PEARL #6 – STOPCOCK AND ONE-WAY VALVE IN THE CORRECT POSITIONS
PEARL #7 – USE A GOOD SUTURE: Don’t let that chest tube come out.
Category: Trauma
Keywords: EMS, c-spine, clearance, (PubMed Search)
Posted: 10/4/2024 by Robert Flint, MD
(Updated: 10/5/2024)
Click here to contact Robert Flint, MD
This Canadian study looked at the safety of paramedics using the modified Canadian C-Spine Rule to determine which pre-hospital blunt trauma patients required immobilization. These were MVC and fall patients predominately. Bottom line: appropriately trained paramedics can use the modified Canadian C-Spine rule to clinically clear cervical spines in the field.

| Result of Application | Paramedics’ Interpretation | Investigators’ Interpretation |
|---|---|---|
| Injury | No Injury | Injury |
| --- | --- | --- |
| Immobilization required (N) | 10 | 1,342 |
| Immobilization not required (N) | 1 | 2,668 |
| Sensitivity, % (95% CI) | 90.9 (58.7–99.8) | 90.9 (58.7 to 99.8) |
| Specificity, % (95% CI) | 66.5 (65.1–68.0) | 68.2 (66.7 to 69.7) |
| Positive likelihood ratio, (95% CI) | 2.7 (2.2–3.4) | 2.9 (2.4 to 3.5) |
| Negative likelihood ratio (95% CI) | 0.1 (0.0–0.9) | 0.1 (0.0–0.9) |
Vaillancourt, Christian et al.
Annals of Emergency Medicine, Volume 81, Issue 2, 187 - 196
Category: Trauma
Keywords: Fall, EMS, injury prevention (PubMed Search)
Posted: 9/30/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This meta analysis looked for studies involving community EMS (CEMS) interventions trying to reduce falls. The authors found:
“CEMS fall prevention interventions reduced all-cause and fall-related emergency department encounters, subsequent falls and EMS calls for lift assist. These interventions also improved patient health-related quality of life, independence with activities of daily living, and secondary health outcomes.”
Further, prospective work needs to be done to look at this on a larger scale. We know falls in elderly patients lead to significant morbidity and mortality. This could be one way to improve fall mortality.
Friend TH, Thomas HM, Ordoobadi AJ_, et al_
Community emergency medical services approaches to fall prevention: a systematic review
Injury Prevention Published Online First:22 July 2024. doi: 10.1136/ip-2023-045110
Category: Geriatrics
Keywords: Geriatric fever score (PubMed Search)
Posted: 9/22/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study attempts to validate the use of the Geriatric Fever Score to predict 30 day mortality in patients over age 65 presenting to an emergency department with fever.
The Geriatric Fever Score uses: leukocytosis, severe coma, and thrombocytopenia. One point is award for each abnormality.
Not surprisingly, mortality went up with the higher the score (33%, 42% and 57% for 0,1,2 points)
For me, I’m not discharging anyone with severe coma, leukocytosis or thrombocytopenia in this patient population therefore I’m not sure this scale has much utility for the practicing emergency physician.
Akbari, H., Mirfazaelian, H., Safaei, A. _et al._Predicting mortality in geriatric patients with fever in the emergency departments: a prospective validation study. BMC Geriatr 24, 758 (2024). https://doi.org/10.1186/s12877-024-05346-x
Category: Trauma
Keywords: seizure, head trauma, levetiracetam (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/19/2024)
Click here to contact Robert Flint, MD
The use of seizure prophylaxes in moderate to severe head injury has been recommended for 7 days post-injury. In general, levetiracetam is used for seizure prophylaxes in this group of patients. This study looked retrospectively at high (over 500 mg BID) vs. low (500 mg bid) dosing and found there was no difference in seizure events in either group. Overall 6% of patients had a seizure in this seven day window even with medication given.
Mann A, Livers K, Frick CD, et al. Evaluation of levetiracetam dosing for seizure prophylaxis in traumatic brain injury. Trauma. 2024;0(0). doi:10.1177/14604086241230598
Category: Trauma
Keywords: c-spine, fracture, Burst (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/16/2024)
Click here to contact Robert Flint, MD
Identify this radiographic finding:
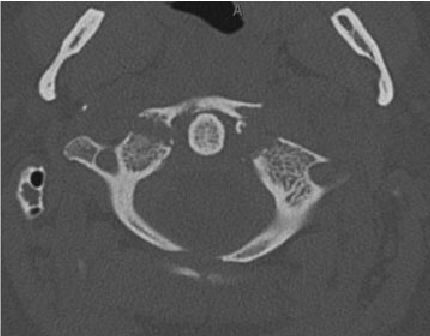
"Jefferson fracture is the eponymous name given to a burst fracture of the atlas. It was originally described as a four-part fracture with double fractures through the anterior and posterior arches, but three-part and two-part fractures have also been described.
50% are associated with other cervical spine injuries
33% are associated with a C2 fracture
25-50% of young children have a concurrent head injury
blunt cerebrovascular injury (BCVI): vertebral artery injury
extracranial cranial nerve injury" 1.
Category: Trauma
Keywords: fracture, spine, x-ray (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/9/2024)
Click here to contact Robert Flint, MD
Identify this injury and other associated injuries:
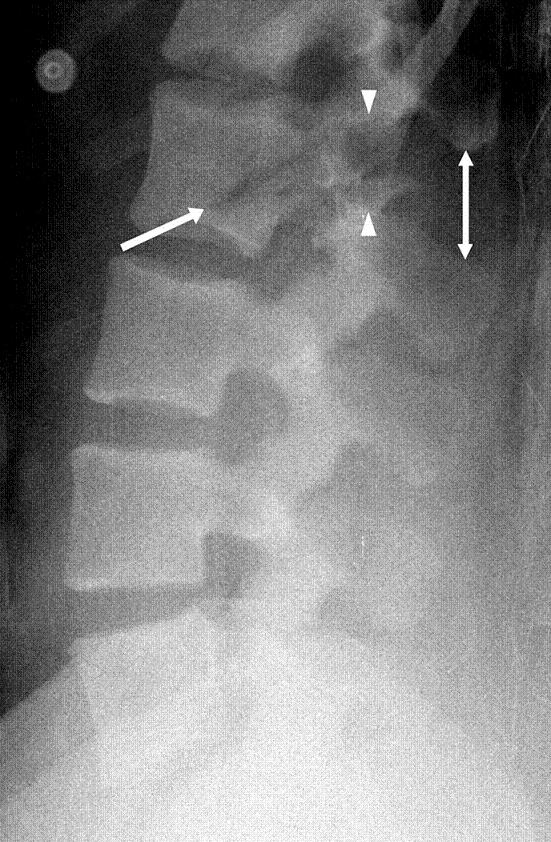
“Chance fractures also referred to as seatbelt fractures, are flexion-distraction type injuries of the spine that extend to involve all three spinal columns. These are unstable injuries and have a high association with intra-abdominal injuries. There is a high incidence of associated intra-abdominal injuries (especially the pancreas, duodenum, and abdominal aorta) that can result in increased morbidity and mortality. Associated intra-abdominal injuries appear to be more common in the pediatric age group with an incidence approaching 50%.” 2.
1.Chance Fracture - Medicalopedia
2. Jones J, Kogan J, Vadera S, et al. Chance fracture. Reference article, Radiopaedia.org (Accessed on 06 Sep 2024) https://doi.org/10.53347/rID-10186
Category: Trauma
Keywords: blunt bowel injury, BIPS, prediction, blunt trauma (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/8/2024)
Click here to contact Robert Flint, MD
Predicting which blunt abdominal trauma patients have mesenteric or bowel wall injuries early in their ED course will decrease morbidity and mortality. It is also a challenge even in the age of advanced CT imaging. This study from India looks at the Bowel Injury Prediction Score as a possible means to catch these injuries early in the course of care. The score uses white blood cell count over 17,000 (1 point), abdominal tenderness at the time of presentation(1 point), as well as a McNutt's scoring scale grade 4 (1 point) (table). The study found those with a score greater than 2 (out of 0-3) were much more likely to have bowel or mesenteric injury at time of laparotomy. Tenderness and CT findings were more likely to be predictive of bowel injury than WBC greater than 17,000. “BIPS had 94.5% sensitivity, 72% specificity, 88% PPV, and 86% NPV for identifying patients with sBBMI.”
My take away is an abnormal CT scan or significant tenderness of presentation warrant concern for mesenteric or bowel wall injury and surgical evaluation is appropriate for these patients. An elevated or normal white blood cell count isn't helpful in these patients. Surgeons may use this scale to help them decide if a patient warrants a trip to the operating room
| GRADE | FINDING |
|---|---|
| 1 | Isolated mesenteric contusion without associated bowel wall thickening or adjacent interloop fluid collection |
| 2 | Mesenteric hematoma?<?5 cm without associated bowel wall thickening or adjacent interloop fluid collection |
| 3 | Mesenteric hematoma?>?5 cm without associated bowel wall thickening or adjacent interloop fluid collection |
| 4 | Mesenteric contusion or hematoma (any size) with associated bowel wall thickening or adjacent interloop fluid collection |
| 5 | Active vascular or oral contrast extravasation bowel transaction or pneumoperitoneum |
Gupta SK, Singh PK, Sharma S, Gupta SK. Prospective validation of Bowel Injury Prediction Score for early diagnosis of surgically significant blunt bowel and mesenteric injury. Trauma. 2023;0(0). doi:10.1177/14604086231187523
Category: Med-Legal
Keywords: adverse event, vital signs, tachycardia, hypotension (PubMed Search)
Posted: 9/6/2024 by Robert Flint, MD
(Updated: 9/7/2024)
Click here to contact Robert Flint, MD
This review reminds us that discharging emergency department patients with abnormal vital signs is a risk for the patient and the provider. The more abnormal vital signs that are present, the higher the risk of adverse event and subsequent return to the emergency department.
“Hypotension at discharge was associated with the highest odds of adverse events after discharge. Tachycardia was also a key predictor of adverse events after discharge and may be easily missed by ED clinicians.”
Always address abnormal vital signs in your medical decision making portion of the chart and be very wary of discharging anyone with tachycardia or other abnormal vital signs.
Can I Discharge This Adult Patient with Abnormal Vital Signs From the Emergency Department?
Long, Brit et al. Journal of Emergency Medicine, Volume 0, Issue 0 Articles in Press May 18, 2024 DOI: 10.1016/j.jemermed.2024.05.009
Category: Trauma
Keywords: IPV, violence, injury, ulna, orthopedics (PubMed Search)
Posted: 9/1/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this systemic literature review of orthopedic injuries identified in intimate partner violence (IPV) the authors remind us that finger, hand, and especially isolated ulnar fractures are very commonly associated with IPV. When we see these injury patterns extra effort is required to determine if IPV is involved.
| Citation | **Bhandari et al.**3 | **Khurana et al.**18 | **Loder et al.**12 | **Porter et al.**13 | **Kavak et al.**7 | **Thomas et al.**17 |
|---|---|---|---|---|---|---|
| Division of injury locations | Fingers, wrist, shoulder dislocation, humerus fracture | Finger, hand, wrist, forearm, elbow, humerus, shoulder | Finger, hand, wrist, forearm, elbow, humerus, shoulder | Radius/ulna, humerus, upper extremity, right/left | Phalanx, radius, ulna (diaphysis/metaphysis, distal/proximal) | Phalanges (distal/medial/proximal), hand/finger, forearm, arm/shoulder right/left |
| Most common UEF location | Fingers (n = 11) | Finger (34.3%) | Finger (9.9%) | Radius and ulna (n = 80; 5.9%) | Ulna (14.5%) | Finger (46%) |
| Most common injury type‡ | Musculoskeletal sprains (all n = 21; 28% back n = 7; neck n = 6) | UEF (27.2%) | Contusions/abrasion (43.4%) | Rib fracture (17.5%) | Soft-tissue lesions (n = 1,007, 82.2%) | UEF (52%) |
* IPV = intimate partner violence, UEF = upper extremity fracture, and UEI = upper extremity injury.
† Summary table demonstrating the location prevalence of UEIs caused by cases of IPV. Fractures were quantified separately from other UEIs in this specific table.
‡ In all included articles the most common injury type was an injury to the head or neck; these are excluded because of the study aim.
Orthopaedic Injury Patterns in Intimate Partner Violence: Defensive Wounds and Fracture PatternsA Systematic Literature Review
Roan Willson, BS Erika Roddy, MDHolly Martinson, PhDCaitlin Farrell Skelton, MPHLisa Taitsman, MD, MPH
The Journal of Bone and Joint Surgery
August 2024; 12 (8): e24.00082
DOI 10.2106/JBJS.RVW.24.00082
