Category: Neurology
Keywords: traumatic brain injury, intracranial pressure, cervical collar, immobilization (PubMed Search)
Posted: 4/23/2020 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Cervical collars can increased ICP in moderate-severe TBI. In patients with poor cerebral compliance and impaired cerebral autoregulation, even a small increase in ICP can affect cerebral perfusion.
Nunez-Latino RA, Rubiano AM, Godoy DA. Impact of cervical collars on intracranial pressure values in traumatic brain injury: a systematic review and meta-analysis of prospective studies. Neurocrit Care. 2020;32(1):469-77.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Coronavirus, SARS, SARS-CoV, COVID-19, SARS-CoV-2 (PubMed Search)
Posted: 3/25/2020 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: SARS-CoV has been associated with CNS involvement. Given their similar pathogenesis and finding of hyposmia in COVID-19, SARS-CoV-2 may be associated with risk of CNS involvement.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: traumatic brain injury, antiplatelet, anticoagulation, CT, neuroimaging (PubMed Search)
Posted: 2/26/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Patients on warfarin or a combination of aspirin and clopidogrel have increased risk of significant intracranial injury after blunt head trauma. Aspirin or clopidogrel monotherapy do not appear to be risk factors.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: spinal cord injury, cauda equina, urinary retention, incontinence (PubMed Search)
Posted: 2/12/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
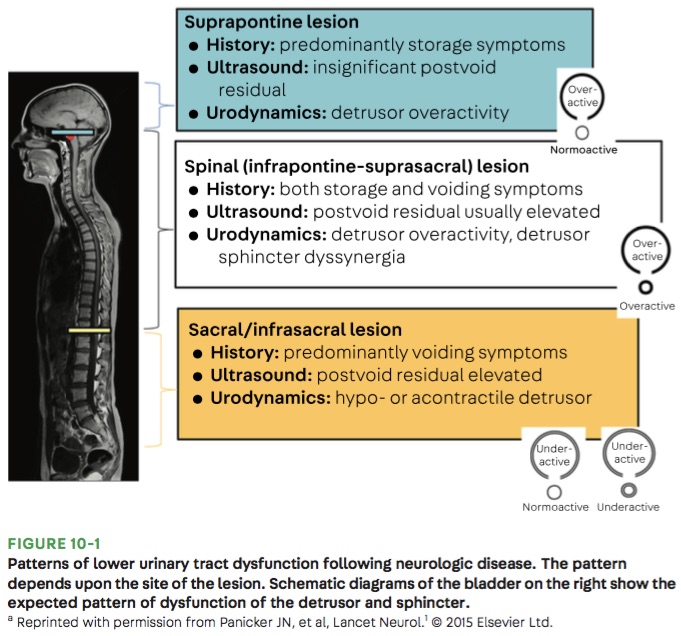
Bottom Line: Urinary retention can be seen with neurological injury involving the lower brainstem, spinal cord, cauda equina, and peripheral nerves.
Panicker JN, Sakakibara R. Lower urinary tract and bowel dysfunction in neurologic disease. Continuum (Minneap Minn). 2020;26(1):178-199.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: ESETT, benzodiazepine, fosphenytoin, valproate, levetiracetam, status epilepticus (PubMed Search)
Posted: 11/27/2019 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Fosphenytoin, valproate, and levetiracetaim have similar efficacy in treatment of benzodiazepine-resistant status epilepticus.
Kapur J, Elm J, Chamberlain JM, et al. Randomized trial of three anticonvulsant medications for status epilepticus. N Engl J Med. 2019;381:2013-13.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Cryptococcus neoformans, cryptococcosis, meningoencephalitis (PubMed Search)
Posted: 10/23/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider cryptococcal meningitis even in immunocompetent patients.
Category: Neurology
Keywords: ACEP, SAH, imaging, nonopioid, CTA, LP (PubMed Search)
Posted: 9/25/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Godwin SA, Cherkas DS, Panagos PD, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med 2019;74(4):e41-74.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH, BP, variability, outcome (PubMed Search)
Posted: 8/28/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Reduced SBP variability is associated with improved outcomes in ICH.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: secondary headache, features, risk factors, red flags (PubMed Search)
Posted: 7/10/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: seizure, status epilepticus, benzodiazepine, antiepileptic, failure (PubMed Search)
Posted: 6/12/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Underdosing of benzodiazepines in status epilepticus may contribute to treatment failure.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: 23.4%, mannitol, intracranial hypertension, herniation, IO (PubMed Search)
Posted: 4/11/2019 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Use of IO allows more rapid administration of 23.4% NaCl with no immediate serious complications.
Wang J, Fang Y, Ramesh S, et al. Intraosseous administration of 23.4% NaCl for treatment of intracranial hypertension. Neurocrit Care. 2019;30(2):364-371.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: headache, back pain, misdiagnosis, stroke, intraspinal, epidural, abscess (PubMed Search)
Posted: 3/14/2019 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The rate of serious neurologic conditions missed at an initial ED visit is low. However, the potential harm of misdiagnosis can be substantial.
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH, volume, ABC/2 (PubMed Search)
Posted: 1/9/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
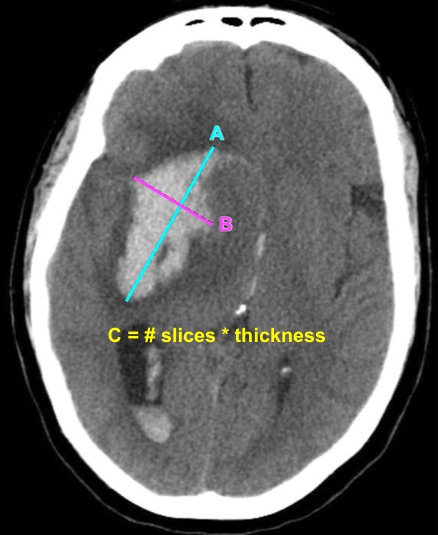
Bottom Line: EPs can reliably estimate ICH volume using the ABC/2 formula. Communicating ICH volume to neurosurgical and neurocritical care consultants can help direct treatment decisions.
Dsouza LB, Pathan SA, Bhutta ZA, et al. ABC/2 estimation in intracerebral hemorrhage: A comparison study between emergency radiologists and emergency physicians. Am J Emerg Med. 2018 Dec 19. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: ultrasound, lumbar puncture, LP, landmark (PubMed Search)
Posted: 12/12/2018 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider using pre-procedural ultrasound-assistance for all lumbar punctures.
Gottlieb M, Holladay D, Peksa GD. Ultrasound-assisted lumbar punctures: a systematic review and meta-analysis. Acad Emerg Med. 2018 Aug 21. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: cervical, spine, clearance, triage, nurse, trauma (PubMed Search)
Posted: 11/14/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: ED triage nurses can safely use the Canadian C-Spine Rule. This approach can improve patient care and decrease length of stay in the ED.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: stroke, TIA, antiplatelet, aspirin, clopidogrel, POINT, CHANCE (PubMed Search)
Posted: 10/10/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Does using a combination of aspirin and clopidogrel decrease your patient’s risk of recurrent stroke after a minor ischemic stroke or high risk TIA event?
Bottom Line: The use of DAPT in minor ischemic stroke and high risk TIA reduces the risk of recurrent stroke. However, the duration of DAPT may affect the risk of major hemorrhage.
| Trial | POINT (Johnston et al, NEJM 2018) | CHANCE (Wang et al, NEJM 2013) |
| Location | N. America, Europe, Australia, New Zealand (82.8% enrolled in the US) | China |
| Population | Age ≥ 18 Within 12 hours of sympton onset NIHSS ≤ 3 or TIA with ABCD ≥ 4 | Age ≥ 40 Within 24 hours of symptom onset NIHSS ≤ 3 or TIA with ABCD ≥ 4 |
| Study Group | Clopidogrel 600mg load, then 75mg daily x 90 days + Aspirin 50-325mg daily x 90 days | Clopidogrel 300mg load, then 75mg daily x 90 days + Aspirin 75mg daily x 21 days |
| Control Group | Aspirin 50-325mg daily x 90 days + Placebo | Aspirin 75mg daily x 90 days + Placebo |
| Primary Efficacy Outcome | Major ischemic event defined as cardiovascular death, stroke, MI | Stroke (ischemic or hemorrhagic) |
| Primary Safety Outcome | Major hemorrhage defined as symptomatic ICH, intraocular bleeding causing vision loss, transfusion ≥ 2 units PRBCs, hospitalization/death related to hemorrhage | Moderate hemorrhage defined as transfusion requirement Severe hemorrhage defined as fatal, ICH, hemodynamic compromise |
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, anticoagulation, low molecular weight heparin, LMWH, UFH (PubMed Search)
Posted: 8/8/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: LMWH appear to be similar in efficacy and safety compared with UFH for the management of CVT.
Al Rawahi B, Almegren M, Carrier M. The efficacy and safety of anticoagulation in cerebral vein thrombosis: a systematic review and meta-analysis. Thromb Res 2018;169:135-9. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Syncope, neurological, neuroimaging, CT, MRI (PubMed Search)
Posted: 6/13/2018 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider obtaining neuroimaging in patients presenting with syncope only if clinical features suggest probable neurological syncope.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH, hematoma expansion, prediction score, BAT score (PubMed Search)
Posted: 5/9/2018 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
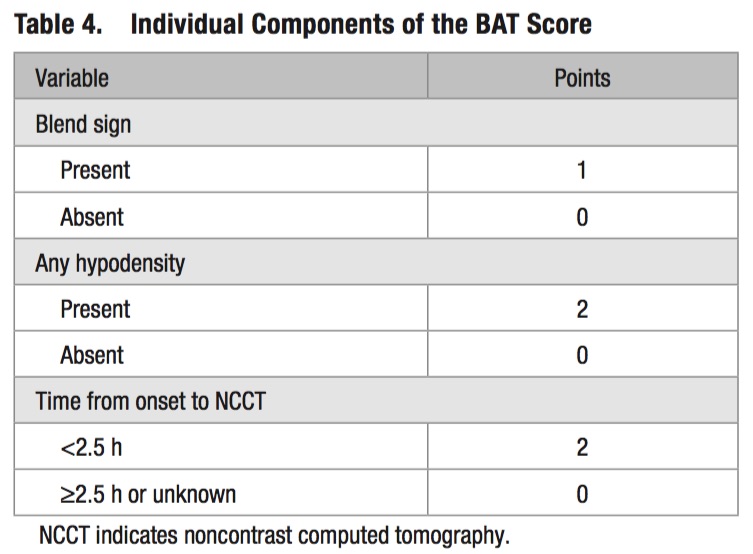
Morotti A, Dowlatshahi D, Boulouis G, et al. Predicting intracerebral hemorrhage expansion with noncontrast computed tomography: The BAT score. Stroke 2018;49(5):1163-9.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: stroke, prehospital, large vessel occlusion, NIHSS, RACE, LAMS, VAN (PubMed Search)
Posted: 3/14/2018 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Follow me on Twitter @EM_NCC
