Category: Neurology
Keywords: acute ischemic stroke, guideline, metric, English, non-English (PubMed Search)
Posted: 12/9/2020 by WanTsu Wendy Chang, MD
(Updated: 12/10/2020)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Patients' language preference does not appear to affect the efficiency of acute ischemic stroke care, especially at experienced high volume stroke centers.
Zachrison KS, Natsui S, Luan Erfe BM, et al. Language preference does not influence stroke patients' symptom recognition or emergency care time metrics. Am J Emerg Med. 2020 Nov 2 [Online ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: migraine, headache, diagnosis, treatment, prevention (PubMed Search)
Posted: 11/11/2020 by WanTsu Wendy Chang, MD
(Updated: 11/13/2020)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Migraine is a common and debilitating condition that benefits from early treatment. Consider initiating preventive therapy for patients who experience at least 2 migraine days per month and adverse effects despite treatment.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: CNS, PNS, UMN, LMN, reflex, Babinski, tone (PubMed Search)
Posted: 10/14/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
| Central Nervous System | Peripheral Nervous System | |
| Pattern of Symptoms | • Hemibody involvement • Weakness of UE extensors • Weakness of LE flexors | • Distal involvement in polyneuropathy • Distal and proximal involvement in polyradiculoneuropathy • Proximal involvement in polyradiculopathy • Sensory often precedes motor symptoms • Pure proximal>distal weakness may be due to myopathy or NMJ disorder |
| Sensory Symptoms | • Central poststroke pain (hyperalgesia, allodynia) • Sensory level in spinal cord pathology • Proprioception involved early in dorsal column disorders | • Neuropathic pain (burning, tingling, shock-like) • Ascending sensory loss involving distal BLE>BUE in polyneuropathy • Proprioception involved late in polyneuropathy |
| Reflexes | • Hyperreflexia in affected limb(s) after acute period • Positive Babinski’s sign | • Hyporeflexia in affected limb(s) |
| Tone | • Increased after acute period | • Decreased |
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, symptoms, treatment, endovascular (PubMed Search)
Posted: 9/23/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Severity of CVT presentation depends on the location and clot burden. Anticoagulation is key, though consider endovascular intervention if patient does not improve or deteriorates despite anticoagulation.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, prothrombotic, headache (PubMed Search)
Posted: 9/10/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The incidence of CVT is increasing with rate of increase higher in males and older females. Consider CVT beyond traditional risk factors.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: trigeminal neuralgia, TN, tic douloureux, neuropathic facial pain (PubMed Search)
Posted: 8/26/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: New onset trigeminal neuralgia needs workup for its etiology. Carbamazepine and oxcarbazepine can be effective for symptom management though continuous or long-lasting pain exacerbations are difficult to treat.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: cerebrospinal fluid, rhinorrhea, otorrhea, halo, double ring, beta-2 transferrin (PubMed Search)
Posted: 8/12/2020 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Beta-2 transferrin is more accurate than the halo sign to identify CSF containing fluid.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: idiopathic intracranial hypertension, papilledema, intracranial pressure, cranial nerve palsy (PubMed Search)
Posted: 7/8/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Idiopathic intracranial hypertension (IIH) is a vision-threatening illness with significant morbidity and needs to be considered as a possible headache diagnosis in the ED. Most often, this occurs in women of childbearing age with a BMI >30, but atypical varieties exist.
Symptoms: Headache (90%), visual disturbance, pulsatile tinnitus, horizotal diplopia.
Signs: Papilledema, 6th cranial nerve (abducens) palsy.
Evaluation: Neuroimaging including CTV or MRV to identify alternate cause including cerebral venous outflow obstruction, lumbar puncture with opening pressure >30 cmH2O (25-30 cmH2O is gray zone), blood work per clinical presentation, CSF analysis.
Treatment: No clear consensus, but typically acetazolamide. Severe or refractory symptoms may require surgical intervention such as optic nerve sheath fenestration, VP shunt, venous sinus stenting.
Hoffmann J, Mollan SP, Paemeleire K, et al. European Headache Federation guideline on idiopathic intracranial hypertension. J Headache Pain. 2018;19(1):93.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: pregnancy, postpartum, migraine, RCVS, CVT, Bell's Palsy, facial palsy (PubMed Search)
Posted: 6/10/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Pregnancy is associated with an increased risk for RCVS, CVT, and Bell’s Palsy. Pregnancy also affects the frequency of migraines due to hormonal fluctuations.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: traumatic brain injury, clinical decision rule, CT utilization, patient decision, benefit, risk, financial incentive (PubMed Search)
Posted: 5/14/2020 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Discussion of benefit/risk and financial incentive associated with head CT in mild TBI affects patient decision. Interestingly in this population studied, more than half of patients will elect to obtain a head CT even in a low-risk scenario.
Iyengar R, Winkels JL, Smith CM, et al. The effect of financial incentives on patient decisions to undergo low-value head CT scans. Acad Emerg Med. 2019;26(10):1118-24.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: traumatic brain injury, intracranial pressure, cervical collar, immobilization (PubMed Search)
Posted: 4/23/2020 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Cervical collars can increased ICP in moderate-severe TBI. In patients with poor cerebral compliance and impaired cerebral autoregulation, even a small increase in ICP can affect cerebral perfusion.
Nunez-Latino RA, Rubiano AM, Godoy DA. Impact of cervical collars on intracranial pressure values in traumatic brain injury: a systematic review and meta-analysis of prospective studies. Neurocrit Care. 2020;32(1):469-77.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Coronavirus, SARS, SARS-CoV, COVID-19, SARS-CoV-2 (PubMed Search)
Posted: 3/25/2020 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: SARS-CoV has been associated with CNS involvement. Given their similar pathogenesis and finding of hyposmia in COVID-19, SARS-CoV-2 may be associated with risk of CNS involvement.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: traumatic brain injury, antiplatelet, anticoagulation, CT, neuroimaging (PubMed Search)
Posted: 2/26/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Patients on warfarin or a combination of aspirin and clopidogrel have increased risk of significant intracranial injury after blunt head trauma. Aspirin or clopidogrel monotherapy do not appear to be risk factors.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: spinal cord injury, cauda equina, urinary retention, incontinence (PubMed Search)
Posted: 2/12/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
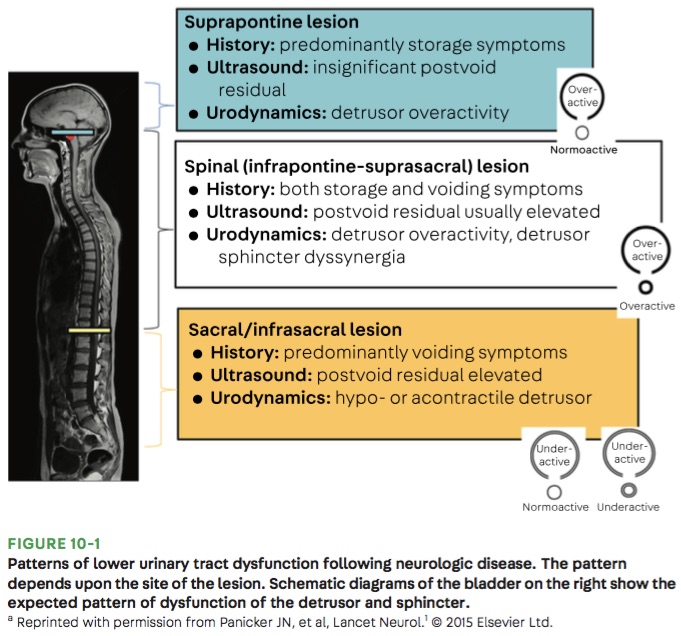
Bottom Line: Urinary retention can be seen with neurological injury involving the lower brainstem, spinal cord, cauda equina, and peripheral nerves.
Panicker JN, Sakakibara R. Lower urinary tract and bowel dysfunction in neurologic disease. Continuum (Minneap Minn). 2020;26(1):178-199.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: ESETT, benzodiazepine, fosphenytoin, valproate, levetiracetam, status epilepticus (PubMed Search)
Posted: 11/27/2019 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Fosphenytoin, valproate, and levetiracetaim have similar efficacy in treatment of benzodiazepine-resistant status epilepticus.
Kapur J, Elm J, Chamberlain JM, et al. Randomized trial of three anticonvulsant medications for status epilepticus. N Engl J Med. 2019;381:2013-13.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Cryptococcus neoformans, cryptococcosis, meningoencephalitis (PubMed Search)
Posted: 10/23/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider cryptococcal meningitis even in immunocompetent patients.
Category: Neurology
Keywords: ACEP, SAH, imaging, nonopioid, CTA, LP (PubMed Search)
Posted: 9/25/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Godwin SA, Cherkas DS, Panagos PD, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med 2019;74(4):e41-74.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH, BP, variability, outcome (PubMed Search)
Posted: 8/28/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Reduced SBP variability is associated with improved outcomes in ICH.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: secondary headache, features, risk factors, red flags (PubMed Search)
Posted: 7/10/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: analgesia, headache, opioids (PubMed Search)
Posted: 6/26/2019 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Primary headaches (not secondary to a life-threatening disease) can be challenging to manage. Remember the following pearls:
Things that DO NOT work: IV fluids, 5-HT3 Antagonists (aka Zofran), diphenhydramine (aka Benadryl), opioids
Things that KINDA work: oxygen for all headaches, sphenopalatine ganglion block (4% lido spray)
Things that PREVENT recurrence: dexamethasone for migraine headaches
