Category: Trauma
Keywords: Pneumothorax, cheat tube, indication (PubMed Search)
Posted: 8/17/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This review article answers the basic question: when does a traumatic pneumothorax require tube thoracostomy?
“A pneumothorax greater than 20% of the thoracic volume on chest x-ray or greater than 35 mm on CT, measured radially from the chest wall to the lung parenchyma, should be treated with tube thoracostomy. Pneumothoraces smaller than this may be observed; approximately 10% of these will fail observation and require tube thoracostomy treatment.”
Blank JJ, de Moya MA. Traumatic pneumothorax and hemothorax: What you need to know. J Trauma Acute Care Surg. 2025 Jul 3. doi: 10.1097/TA.0000000000004692. Epub ahead of print. PMID: 40604368.
Category: Trauma
Keywords: Gunshot, ptsd, reinjury (PubMed Search)
Posted: 8/10/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This paper outlines the long term effects of surviving a gunshot wound. The authors conclude:
“Firearm injury survivors frequently experience chronic pain, nerve injury, retained bullet fragments that may cause lead toxicity, physical limitations, and PTSD and are at risk for reinjury. In addition to supportive medical and psychiatric care, survivors of firearm injury may benefit from health care–based violence intervention programs.”
Strong BL, Lauerman MH, Scalea TM. Sequelae and Care After Firearm Injury. JAMA. Published online July 23, 2025. doi:10.1001/jama.2025.10498
Category: Trauma
Keywords: Hypothermia, trauma, mortality (PubMed Search)
Posted: 8/3/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Looking at a trauma database of over 3 million patients, 1% presented with prehospital hypothermia (<35 degrees C). These patients had longer hospital stays, higher resource utilization and higher mortality. Even isolated head injury patients with hypothermia had worse outcomes. Rewarming did increase survival slightly for all patients.
Take away: rewarm hypothermic trauma patients as soon as possible to improve mortality.
Anna Mary Jose, Aryan Rafieezadeh, Muhammad Zeeshan, Jordan Kirsch, Gabriel Froula, Kartik Prabhakaran, Bardiya Zangbar,
Hypothermia on admission predicts poor outcomes in adult trauma patients,
Injury,
Volume 56, Issue 5,
2025,
112076,
ISSN 0020-1383,
https://doi.org/10.1016/j.injury.2024.112076
Category: Trauma
Keywords: Gun shot, antibiotics, prophylaxis, fracture (PubMed Search)
Posted: 7/31/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Looking at 140 patients retrospectively who had abdominal gunshot wounds with associated fractures, prophylactic antibiotics longer than three days did not offer any benefit in preventing fracture infection. Only two patients experienced fracture related infections and 65 total experienced any infection related complications.
From and ED standpoint, it appears reasonable to give a dose of antibiotics in this very rare subset of gunshot wound patients.
Kahler D, DeWitte N, Thompson M, Rehman S, Anderson J. Prophylactic antibiotics in gunshot fractures with concomitant bowel injury to prevent fracture-related infections and other infectious complications. Injury. 2025 Jun;56(6):112304. doi: 10.1016/j.injury.2025.112304. Epub 2025 Apr 8. PMID: 40279804.
Category: Trauma
Keywords: Bcvi, stroke, CVA (PubMed Search)
Posted: 7/28/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
A retrospective, single Australian center review of 300 patients who had blunt cerebral vascular injuries found:
-9.8% had an inpatient CVA
-Most occurred in first 72 hours
-Those receiving no anti coagulation or antiplatelets had 28% CVA incidence.
-Those treated had a 3.6% CVA incidence (anti platelets were better than anti coagulation)
-Carotid artery injury was less common than vertebral artery but had higher frequency of CVA
-associated factors: low GCS, rib fractures, severe trauma
Take away: non-treatment of blunt cerebral vascular injuries had higher inpatient stroke risk. Antiplatelet agents such as aspirin and Clopidogrel performed better than anticoagulants
Stanislaus V, Zhang WW, Chen Z, et al. Inpatient stroke outcomes in patients with blunt cerebrovascular injuries according to risk factors and treatment. Trauma. 2025;0(0). doi:10.1177/14604086251333569
Category: Trauma
Keywords: Mussed injuries, trauma, tertiary survey, (PubMed Search)
Posted: 7/27/2025 by Robert Flint, MD
Click here to contact Robert Flint, MD
This paper looked at the literature regarding missed injuries in trauma patients. Missed injuries was defined as an injury discovered after the patient was discharged. Most of the missed injuries and causes are not novel but are worthy of remembering.
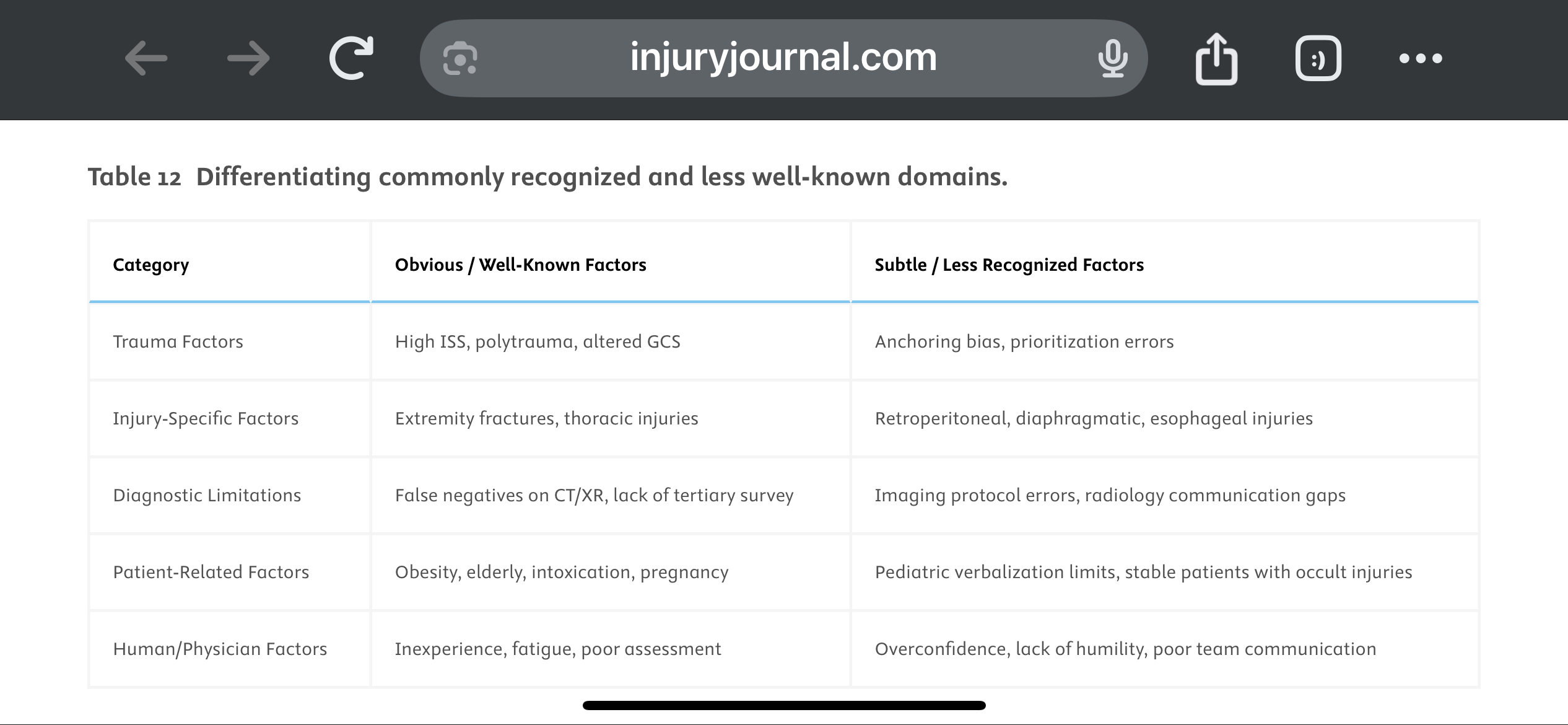
They suggest a Trauma Tertiary Survey helps prevent missed injury. “Tertiary Survey (TTS), which includes a thorough in-hospital re-examination and a review of diagnostic investigations within the first 24 h, has been shown to significantly reduce the occurrence of missed injuries (1–9 %) in severe trauma patients found after a primary and secondary survey.” This concept is similar to a discharge time out in emergency medicine where all data is reviewed, viral signals are confirmed normal and a team discharge is performed.
The paper offers these suggestions to avoid missed injuries:
1.
Standardize Tertiary Trauma Surveys (TTS).
2.
Be Cognizant of Cognitive Biases (e.g., Anchoring Bias).
3.
Repeat Imaging When Clinically Indicated.
4.
Use Protocolized Imaging Techniques (CT/MRI).
5.
Ensure Radiology-Trauma Communication.
6.
Prioritize High-Risk Populations.
7.
Implement Peer Review or Double-Check Systems.
8.
Encourage a Culture of Collaboration and Humility.
9.
Limit Provider Fatigue and Overload.
10.
Create Tailored Checklists for Subtle Injuries.
Vieira, Lucas Fontenelle et al.
Injury, Volume 56, Issue 8, 112600
Category: Trauma
Keywords: TBI, management, parameters (PubMed Search)
Posted: 7/20/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Outcomes in traumatic brain injury are improved when physiologic homeostasis is achieved as soon as possible after injury. Here are the American College of Surgeons’ recommendations. Note SBP over 110 and a hemoglobin over 7. A study looking at a more liberal transfusion target showed worse ARDS and no mortality benefit.
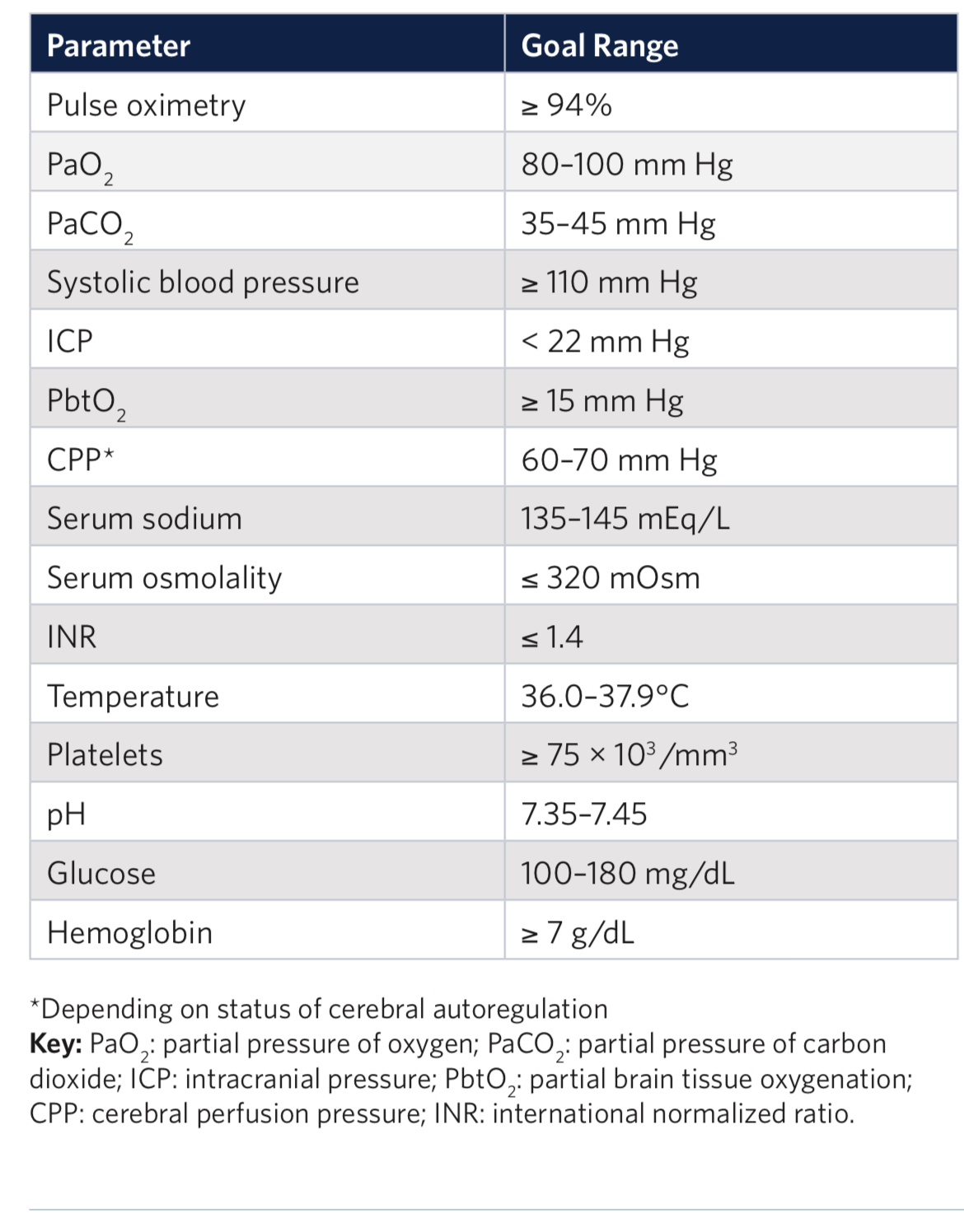
2. Liberal or Restrictive Transfusion Strategy in Patients with Traumatic Brain Injury
Authors: Alexis F. Turgeon, M.D. https://orcid.org/0000-0001-5675-8791, Dean A.Fergusson, Ph.D., Lucy Clayton, M.Sc., Marie-Pier Patton, M.Sc., Xavier Neveu, M.Sc., Timothy S. Walsh, M.D., Annemarie Docherty, M.D., Ph.D., +48 , for the HEMOTION Trial Investigators on behalf of the Canadian Critical Care Trials Group, the Canadian Perioperative Anesthesia Clinical Trials Group, and the Canadian Traumatic Brain Injury Research Consortium*
June 13, 2024N Engl J Med 2024;391:722-735DOI: 10.1056/NEJMoa2404360VOL. 391 NO. 8
Category: Trauma
Keywords: Pedestrian, fatality, injury, cyclist (PubMed Search)
Posted: 7/12/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study from Great Britain compared fatalities for pedestrians and cyclist struck by motor vehicles based on vehicle body type. They found :
“We conclude that in Great Britain, being hit by an SUV as opposed to a passenger car increases injury severity among pedestrians and cyclists, with the strongest effect in children.“
Goodman, Anna, Phil Edwards, and Anthony A. Laverty. 2025. “Do Sports Utility Vehicles (SUVs) Cause More Severe Injuries to Pedestrians and Cyclists than Passenger Cars, in the Case of a Crash? Findings from Great Britain, 2004-2023.” Findings, July. https:/?/?doi.org/?10.32866/?001c.141647.
Category: Trauma
Keywords: Shock index, transfusion, hypotension (PubMed Search)
Posted: 7/5/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
These authors looked at 5958 trauma patients arriving at their trauma center with a systolic blood pressure greater than 90. They calculated shock index (heart rate /sbp) for all of these and then looked at who received a blood transfusion within one hour of arrival. 211 patients received blood in that time frame. “Patients were stratified by SI using the following thresholds: ? 0.7, > 0.7 to 0.9, > 0.9 to 1.1, > 1.1 to 1.3, and > 1.3.”
“A main effect was observed for shock index with increased risk for required transfusion for patients with admission shock index >0.7 (P < 0.001). In comparison to shock index of ? 0.7, odds ratios were 2.5(1.7 - 3.8), 8.2(5.4 - 12.2), 24.9(15.1 - 41.1), 59.0(32.0 - 108.6) for each categorical increase in SI.”
Lin TM, Memon AM, Reeson EA, Tolan GC, Low TM, Kupanoff KM, Huang DD, Jones MD, Czarkowski BR, Soe-Lin H, Bogert JN, Weinberg JA. Shock index identifies compensated shock in the 'Normotensive' trauma patient. Injury. 2025 May 8:112419. doi: 10.1016/j.injury.2025.112419. Epub ahead of print. PMID: 40379507.
Category: Trauma
Keywords: facial fracture, transfer, guidelines (PubMed Search)
Posted: 6/29/2025 by Robert Flint, MD
(Updated: 7/2/2025)
Click here to contact Robert Flint, MD
Based on a review of 511 patients transferred to a level one trauma center for evaluation of facial fractures, this group developed the Facial Fracture Transfer Guidelines. they found that over half of the patients transferred to them did not require intervention and were discharged within 6 hours. These guidelines are meant to decrease unneeded transfers yet provide appropriate care to those with traumatic facial injuries.
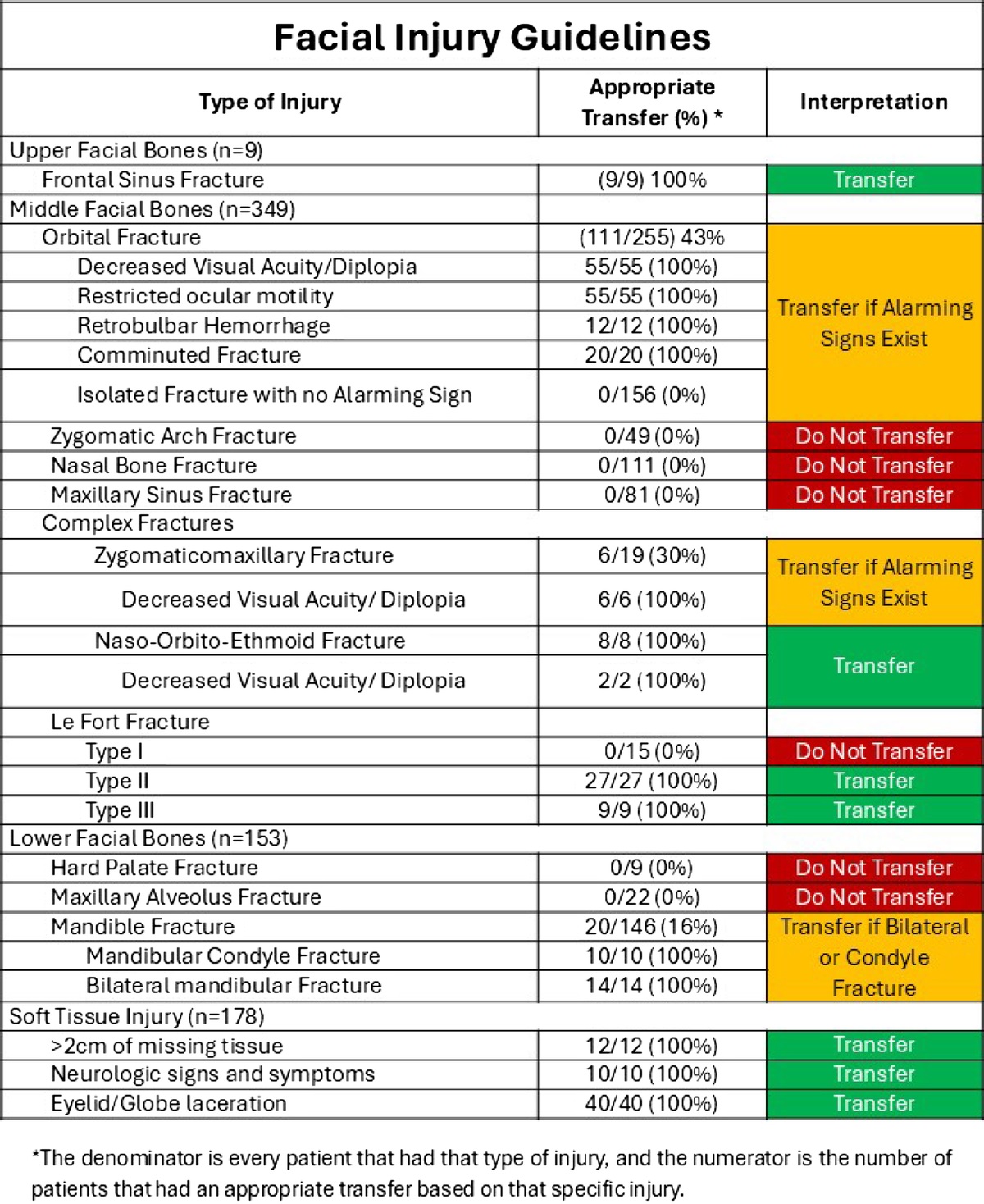
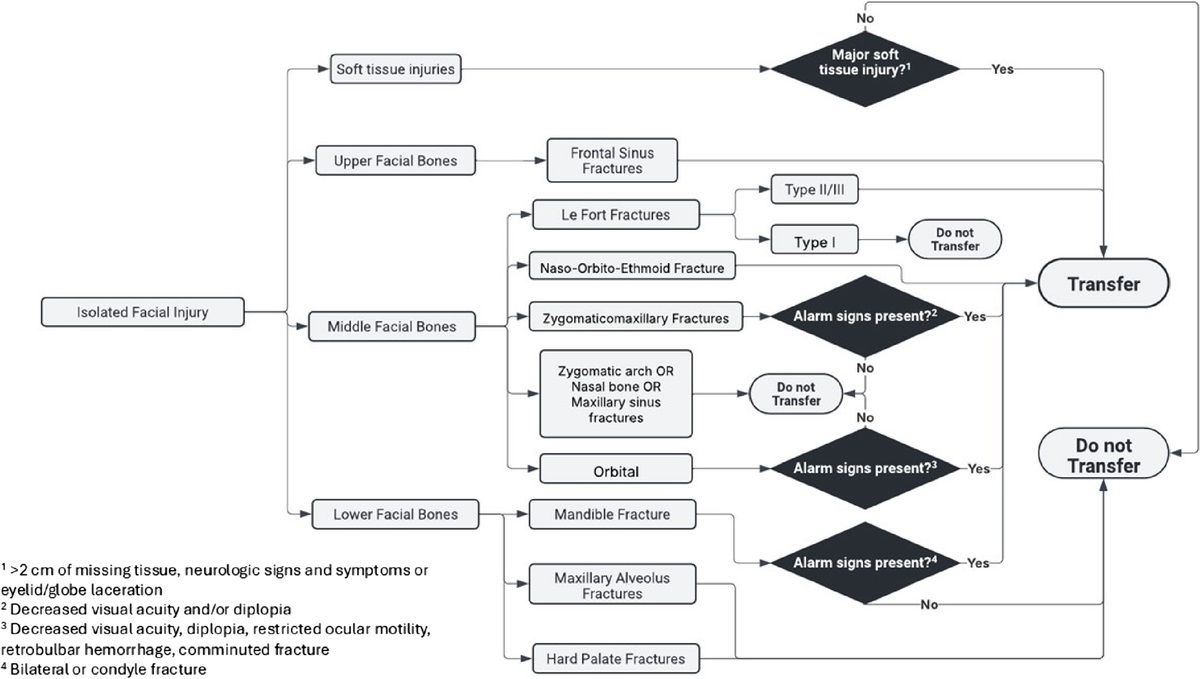
Castillo Diaz, Francisco MD; Anand, Tanya MD, MPH, FACS; Khurshid, Muhammad Haris MD; Kunac, Anastasia MD, FACS; Al Ma'ani, Mohammad MD; Colosimo, Christina DO, MS, FACS; Hejazi, Omar MD; Ditillo, Michael DO, FACS; Magnotti, Louis J. MD, MS, FACS; Joseph, Bellal MD, FACS. Look me in the face and tell me that I needed to be transferred: Defining the criteria for transferring patients with isolated facial injuries. Journal of Trauma and Acute Care Surgery ():10.1097/TA.0000000000004651, May 9, 2025. | DOI: 10.1097/TA.0000000000004651
Category: Trauma
Keywords: facial fracture, Le Fort, orbital fracture (PubMed Search)
Posted: 6/29/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
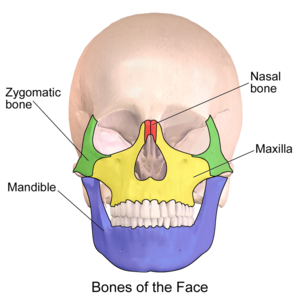
Most common facial fracture is the nasal fracture followed by the zygomatic arch fractures.
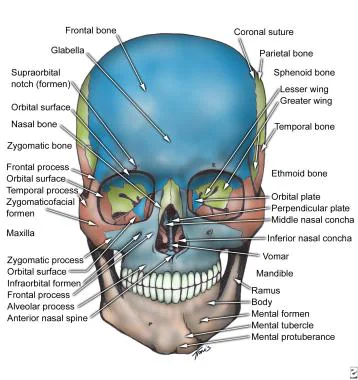
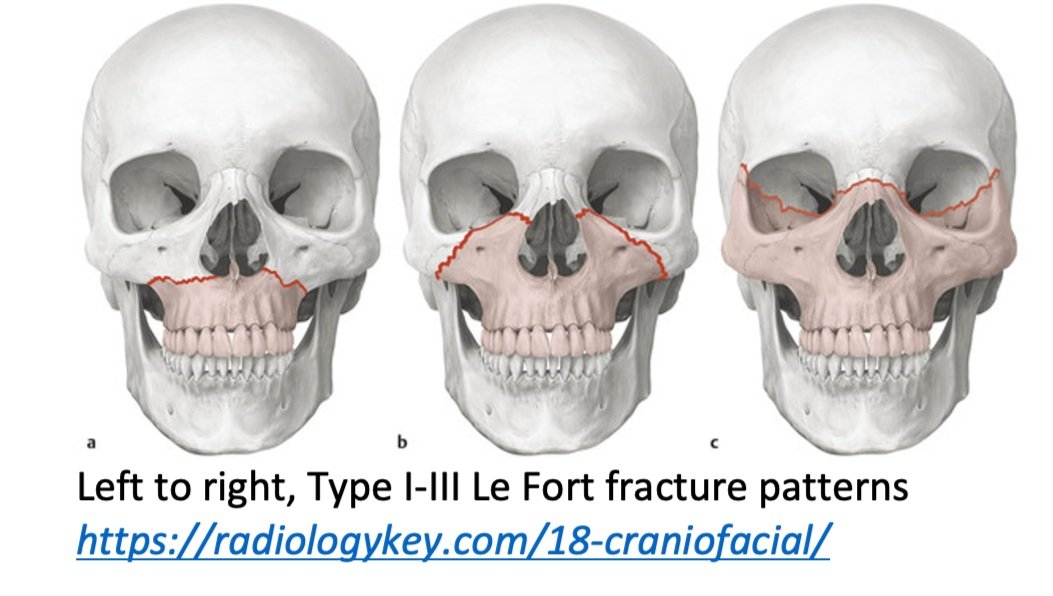
Le Fort Classification of facial fractures/facial stability. The higher the number, the more unstable.
Orbital blow out fractures may entrap the ocular muscles leading to eye immobility in various directions.
Category: Trauma
Keywords: Head injury, BIG, pediatric (PubMed Search)
Posted: 6/23/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Brain injury guidelines were designed to decrease transfers and neurosurgical consults for adults with head injuries.
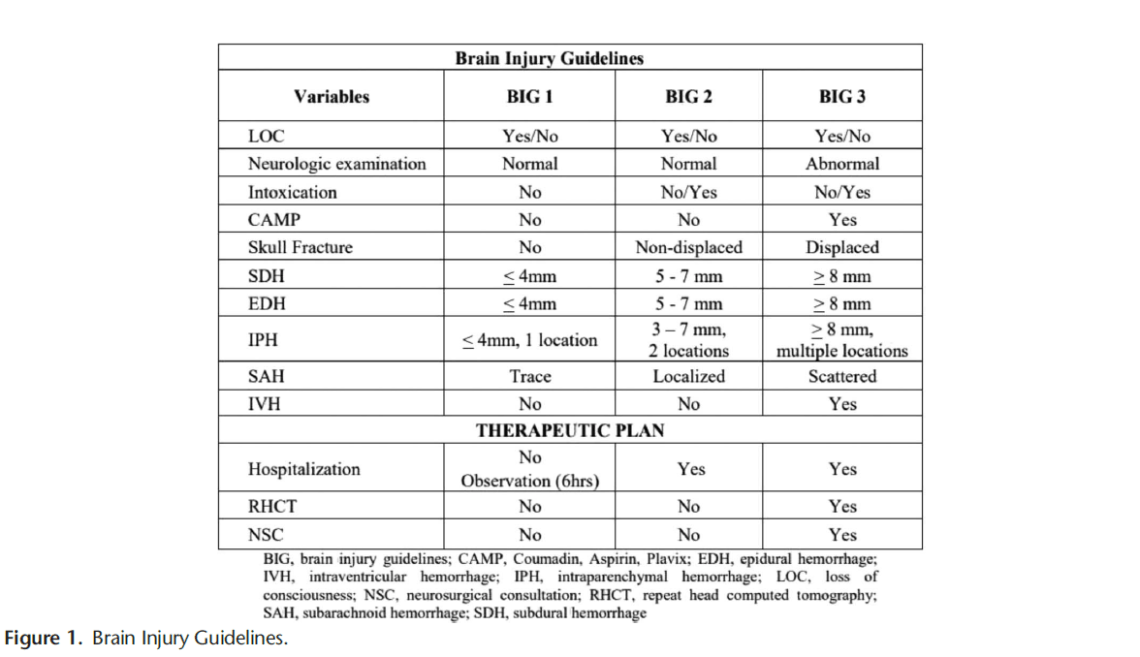
A new retrospective study suggests that modified guidelines may be feasible in the pediatric population as well. More data is needed but this is an important step in assuring safe resource utilization in pediatric head injury patients.
1. https://first10em.com/the-brain-injury-guidelines-can-we-avoid-talking-to-neurosurgeons/
2. Kay AB, Glasgow SL, Kahan AM, Swendiman RA, Kastenberg ZJ, Roach CM, Wan HY, Bollo RJ, Iyer RR, Ravindra VM, Morris DS, Yorkgitis BK, Joseph B, Russell KW. Small Change, BIG Impact: Proposal of the Brain Injury Guidelines for kids (kBIG). J Pediatr Surg. 2025 May 17;60(8):162372.
Category: Trauma
Keywords: Intubation, trauma, mortality, operating room, Ed (PubMed Search)
Posted: 6/15/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
In this Israeli study comparing mortality for trauma patients intubated in the emergency department vs the operating room, in hospital mortality was higher for the ED group before controlling for injury severity score and shock. After controlling for injury severity and shock, there was no difference in In hospital mortality. Coupled with previous research, if intubation can wait until after resuscitation and in the OR, that is ideal. And sometimes it just has to happen in the ED and we should be prepared for rapid resuscitation.
Talmy T, Radomislensky I, Brzezinski Sinai I, Shaylor R, Katorza E, Gendler S; Israel Trauma Group Collaborators. Intubation Setting and Mortality in Trauma Patients Undergoing Hemorrhage Control Surgery: A Propensity Score-Matched Analysis. Anesth Analg. 2025 May 16. doi: 10.1213/ANE.0000000000007542. Epub ahead of print. PMID: 40378073.
Category: Trauma
Keywords: Hysterotomy (PubMed Search)
Posted: 6/8/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Another case series of 3 resuscitative hysterotomies, all performed by obstetricians, reported 33% maternal and 67% neonate survival.(1).
The mechanics of the procedure are:
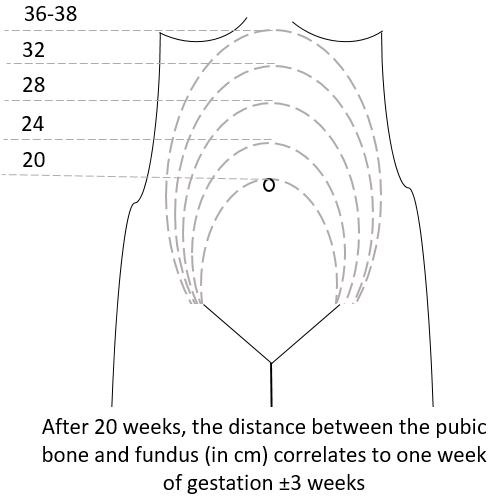
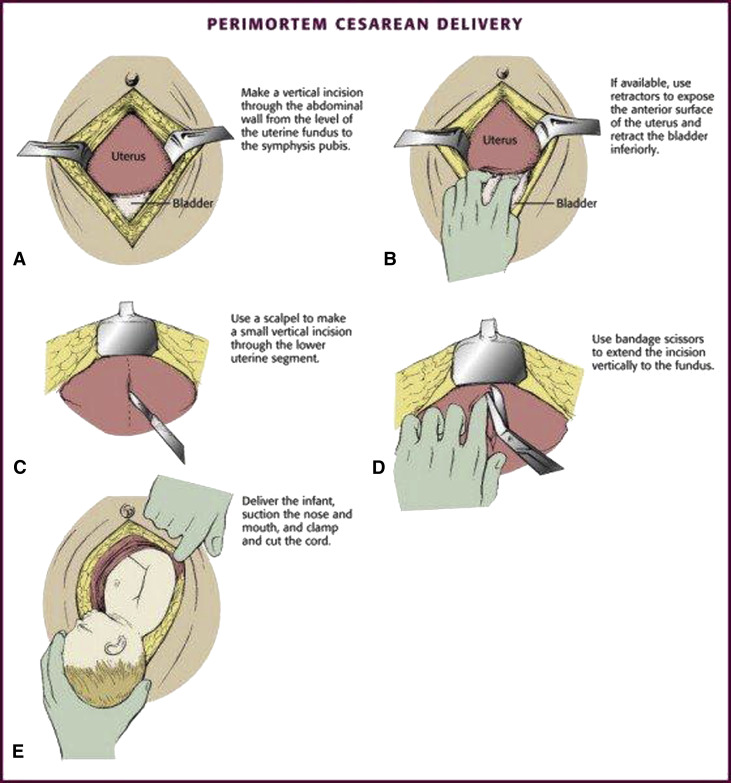
(3)
Category: Trauma
Posted: 6/7/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
A literature search revealed very little evidence, however in 66 women and 68 neonates who underwent resuscitative hysterotomy for out of hospital cardiac arrest 4.5% of women and 45% of neonates survived to discharge. The longest down time was 29 minutes and 47 minutes for women and neonates respectively. While more evidence is needed, it appears this procedure should be performed as early as possible and may lead to some survival benefit.
Leech C, Nutbeam T, Chu J, Knight M, Hinshaw K, Appleyard TL, Cowan S, Couper K, Yeung J. Maternal and neonatal outcomes following resuscitative hysterotomy for out of hospital cardiac arrest: A systematic review. Resuscitation. 2025 Feb;207:110479. doi: 10.1016/j.resuscitation.2024.110479. Epub 2024 Dec 29. PMID: 39736393.
Category: Trauma
Keywords: Femur fracture, splint (PubMed Search)
Posted: 6/6/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
The National Association of Emergency Medical Service Physicians reminds us that femur fractures rarely cause enough blood loss to cause hemodynamic instability (look for other sources), often have concomitant injuries in the pelvis or distal extremity, and can be effectively splinted either static or with traction (which has contraindications, complications, and technical hurdles).
John W. Lyng, Joshua G. Corsa, Philip S. Nawrocki, Brad D. Raetzke, Josh
Nackenson & Nichole Bosson (07 May 2025): Prehospital Trauma Compendium: Management
of Suspected Femoral Shaft Fractures – A position statement and resource document of
NAEMSP, Prehospital Emergency Care, DOI: 10.1080/10903127.2025.2493846
To link to this article: https://doi.org/10.1080/10903127.2025.2493846
Category: Trauma
Keywords: Nail gun injury, surgery, antibiotics (PubMed Search)
Posted: 5/31/2025 by Robert Flint, MD
(Updated: 6/1/2025)
Click here to contact Robert Flint, MD
An Australian retrospective study of 158 patients treated for nail gun injuries found those treated with operative debridement or with prophylactic antibiotics had no different 30 day infection rates compared to patients receiving no antibiotics.
Slater S, Vasudeva M, Mitra B, Sreedharan S. Penetrating nail gun injuries: Role of antibiotics and surgical management. Trauma. 2025;0(0). doi:10.1177/14604086251320524
Category: Trauma
Keywords: geriatric, trauma, CT scan (PubMed Search)
Posted: 5/29/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This literature search from 1946-2023 looking at comparing selective use of CT scans vs whole body scans in geriatric trauma found no benefit of whole body CT in mortality, hospital length of stay or ED discharge. This study only included 15,000 pts over that very long time line. More robust, current work needs to be done on this important topic.
Tang P, Elkington O, Stevens S. Whole body CT-scan vs. selective CT-scan in geriatric trauma: Systematic review and meta-analysis. Trauma. 2025;0(0). doi:10.1177/14604086241304629
Category: Trauma
Keywords: Incarcerated, trauma, mortality, disparity (PubMed Search)
Posted: 5/11/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Looking at a year’s worth of data from the National Trauma Databank, the authors found incarcerated trauma patients were more likely to be stabbed, male, persons of color and have a higher adjusted mortality rate.
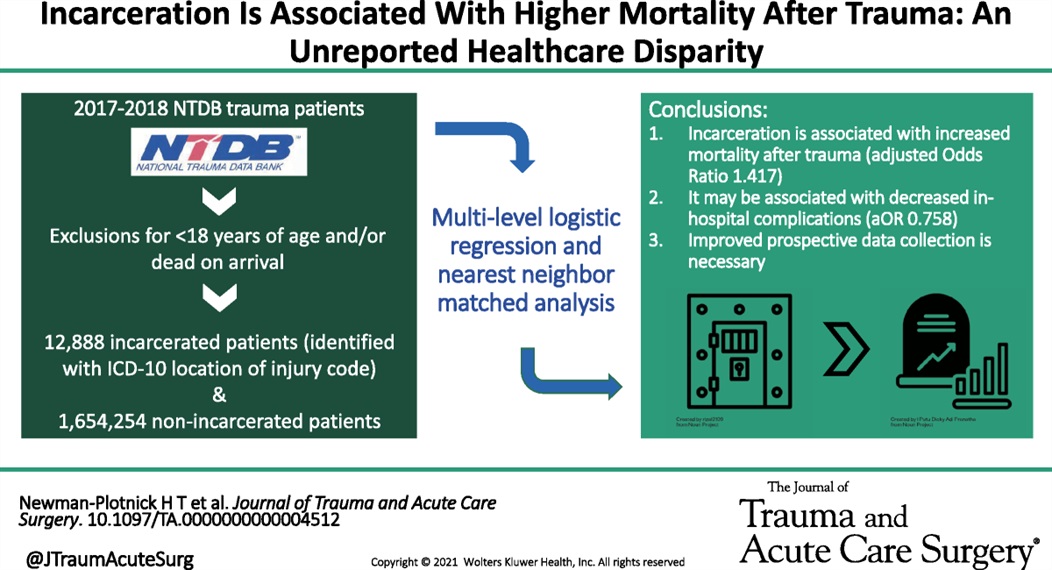
Newman-Plotnick, Harry MD, MPH; Byrne, James P. MD, PhD; Haut, Elliott Richard MD, PhD, FACS; Hultman, Charles Scott MD, MBA, FACS
Journal of Trauma and Acute Care Surgery 98(5):p 785-793, May 2025. | DOI: 10.1097/TA.0000000000004512
Category: Trauma
Keywords: Gun violence, mental health, suicide (PubMed Search)
Posted: 4/28/2025 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study looked at exposure to gun violence and found increased use of mental health resources, depression and suicide risk even with a single exposure. Repetitive exposure increased suicide risk as well as mental health service utilization, depression and overall health service utilization. While further work is needed, screening our patients for gun violence exposure could undercover mental health needs.
Daniel C. Semenza, Allison E. Bond, Devon Ziminski, Michael D. Anestis,
Frequency, recency, and variety of gun violence exposure: Implications for mental health and suicide among US adults,
Social Science & Medicine,
Volume 366,
2025,
117672,
ISSN 0277-9536,
https://doi.org/10.1016/j.socscimed.2025.117672.
(https://www.sciencedirect.com/science/article/pii/S0277953625000012
