Category: Orthopedics
Keywords: Benzodiazepines, Back Pain, Sciatica (PubMed Search)
Posted: 5/8/2010 by Michael Bond, MD
(Updated: 5/9/2010)
Click here to contact Michael Bond, MD
Conservative Treatment of Back Pain:
Muscle relaxanats and benzodiazipnes are often used in the non-operative management of sciatica and non-specific low back pain. In fact, a 2003 Cochrane review concluded that muslce relaxanats were effective in the management of non-specific low back pain. However, a recent analysis of randomized trials reported little efficacy or only minor benefits with the use of benzodiazapines in treatment of low back pain.
A recent prospective, randomized, placebo-controlled, double-blinded trial conducted in Germany that enrolled a total of 60 patients found that the use of diazepam was equivilant to placebo in the reduction of distance of referred pain at day 7 of treatment. Diazepam was also noted on average to increase the length of stay of those patients hospitalized by 2 days (median hospital days of 8 for placebo versus 10 for diazepam), and the probablility of pain reduction on a visual analog scale by more than 50% was twice as high in the placebo group (p< 0.0015). Placebo reduced the patients pain more than diazepam.
Though the sample size was small; this study should really make one reevaluate the use of diazepam in the treatment of back pain. Early movement and discouraging bed rest have been associated with decreased back pain, so one mechanism by which benzodiazepines may make things work is by causing enough sedation to prevent early movement.
Brotz D, Maschke E, Burkard S, Engel C, Manz C, Ernemann U, Wick W, Weller M: Is there a role for benzodiazepines in the management of lumbar disc prolapse with acute sciatica? Pain 2010.
Category: Orthopedics
Posted: 4/25/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Carpal Tunnel Syndrome (CTS):
Category: Orthopedics
Keywords: Hip Dislocation, Treatment (PubMed Search)
Posted: 4/11/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Prosthetic hip dislocations are a common occurance in the Emergency Department. After you have gotten the hip back in place there are several ways to prevent the hip from coming out again. An abductor pillow will work but it confines the patient to bed. A better option to prevent further hip dislocations until the patient can get an appropriate brace made or reparative surgery is to place the patient in a straight leg knee immoblizer. It is nearly impossible to dislocate your hip if your knee is fully extended.
So after reduction of their simple hip dislocation (i.e: no fractures) place the patient in a straight leg knee immobolizer and they can followup with their orthopedist as an outpatient.
Category: Orthopedics
Keywords: Ossification Centers, Elbow (PubMed Search)
Posted: 3/27/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Review of the Appearance of Ossification Centers in Children's Elbows
Determing if a child's elbow has a fracture or if you are looking at an ossification center is easier if you remember the mnemonic CRITOE. This is the order that the ossification centers appear:
Category: Orthopedics
Keywords: Knee, Dislocation (PubMed Search)
Posted: 3/13/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Knee Dislocation:
Klineberg EO, Crites BM, Flinn W, et al: The role of arteriography in assessing popliteal artery injury in knee dislocations. J Trauma. 2004 Apr;56(4):786-90.
Hollis JD, Daley B, et al: 10-year review of knee dislocations: is arteriography always necessary? J Trauma. 2005 Sep;59(3):672-5.
Category: Orthopedics
Keywords: Pelligrini, Steida (PubMed Search)
Posted: 3/6/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Pelligrini-Stieda Lesion:
A Pelligrini-Stieda lesion is shown in the radiograph below. This lesion was originally described in 1905, and is associated with a tear of the Medial Collateral Ligament. Heterotrophic calcification forms causing chronic pain, which typically needs to be surgically excised.
So for the students out there, it is possible to diagnosis an MCL tear on plain radiographs. Just not very often.

Category: Orthopedics
Keywords: Segond Fracture (PubMed Search)
Posted: 2/27/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
The Segond Fracture:
An benign appearing avulsion fracture of the lateral tibeal plateau that is marker for more significant injuries such as:
If this avulsion fracture is seen consider immobilzing the patients knee until they can follow up with Orthopedics and/or get an MRI to determine if additional injuries are present.

Category: Orthopedics
Keywords: Spine, Fracture, Diagnosis (PubMed Search)
Posted: 2/20/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
A recent study by Smith et al showed that the general abdomen/pelvic CT scan in trauma patients obtained with 5mm slices is a better screening test for spine fractures than plain films. They also showed that when compared to dedicated reconstructed thoracolumbar CT scan (2mm slices focused on the spine) it did not miss any clinically significant fractures.
The statistic for plain radiographs and the nonreconstructive CT scan are shown below.
| | Plain Radiographs | Nonreconstructive CT Scan | ||
| | Lumbar | Thoracic | Lumbar | Thoracic |
| Sensitivity % [95% CI] | 47 [33 to 62] | 13 [3 to 32] | 94 [83 to 99] | 73 [50 to 89] |
| Specificity % [95% CI] | 91 [78 to 97] | 71 [54 to 85] | 95 [85 to 99] | 94 [79 to 99] |
| Positive Predictive Value % [95% CI] | 85 [66 to 96] | 15 [2 to 45] | 95 [86 to 99] | 89 [67 to 99] |
| Negative Predictive Value % [95% CI] | 61 [48 to 72] | 56 [41 to 71] | 93 [82 to 99] | 83 [66 to 93] |
The take home point is that dedicated Spine CT scans are probably not needed unless they are going to be used to guide surgical or non-surgical management, and plain films should probably be abandoned in patients that are undergoing CT scans of the chest/abdomen/pelvis.
Smith MW, Reed JD, Facco R, Hlaing T, McGee A, Hicks BM, Aaland M: The reliability of nonreconstructed computerized tomographic scans of the abdomen and pelvis in detecting thoracolumbar spine injuries in blunt trauma patients with altered mental status. J Bone Joint Surg Am 2009; 91: 2342-2349.
Category: Orthopedics
Posted: 2/14/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Impingement Syndrome and the Diagnostic Accuracy of 5 Common Tests
It is also reported that subacromial impingement syndrome (SAIS) is the more frequent cause of shoulder pain.
The authors of this study attempted to determine the diagnostic accuracy of the following 5 tests for SAIS:
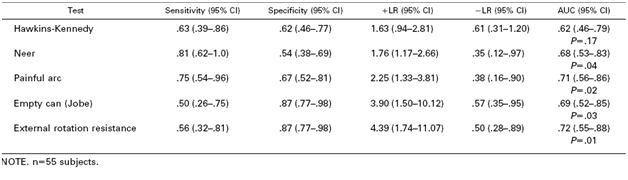
The study demonstrated that any 3 positive tests out of the 5 has a sensitivity of 0.75 (0.54-0.96) , specificity of 0.74 (0.61-0.88), positive likelihood ratio of 2.93 (1.60-5.36) and negative likelihood ratio of 0.34 (0.14-0.80). See the table below for the individual test characteristics. No single test was deemed accurate enough to make the diagnosis by itself.
So in the end you should be familiar with most of these tests in order to use a combination of them to make the diagnosis of impingement syndrome. Future pearls will review how to perform these tests.
Michener LA, Walsworth MK, Doukas WC, Murphy KP: Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil 2009; 90: 1898-1903.
Category: Orthopedics
Keywords: Scaphoid, Fracture (PubMed Search)
Posted: 2/6/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Scaphoid Fractures:
For suspected scaphoid fractures with negative radiographs it is common practice to put a person in a short arm thumb spica splint until followup up radiographs can be obtained in 10-14 days.
However, there is evidence that a short arm thumb spica splint is not enough for people that have a true scaphoid fracture. Gellman et al demonstrated that long arm thumb-spica cast immobilization for six weeks followed by short arm thumb-spica cast immobilization decreased time to union by 25% when compared to short arm thumb-spica casting alone.
The theory is that the short arm splint still allows for forearm rotation that can cause shearing motion of the volar radiocarpal ligaments. A long arm splint prevents this shearing action. The disadvantage of a long arm splint though is potential elbow joint stiffness and muscle atrophy that can occur during the prolonged period of immobilization.
So for your next patient with a scaphoid fracture seen on radiographs place them in a long arm thumb spica splint.
Gellman H, Caputo RJ, Carter V, Aboulafia A, McKay M. Comparison of short and long thumb-spica casts for non-displaced fractures of the carpal scaphoid. J Bone Joint Surg Am. 1989; 71:354-357.
Lawton JN, Nicholls MA, Charoglu CP. Immobilization for Scaphoid Fracture: Forearm Rotation in Long Arm Thumb-spica Versus Munster Thumb-spica Casts. Orthopedics 2007; 30:612
Category: Orthopedics
Keywords: Paronychia (PubMed Search)
Posted: 1/9/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Acute paronychia
Category: Orthopedics
Keywords: Scaphoid, Children (PubMed Search)
Posted: 11/14/2009 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Scaphoid Fractures in Children:
Because of the high (30%) fracture rate seen on followup films it is recommended that all children be placed into a thumb spica splint until followed up.
Evenski AJ, Adamczyk MJ, Steiner RP, Morscher MA, Riley PM. Clinically Suspected Scaphoid Fractures in Children. J Pediatr Orthop 2009; 29: 352-355.
Category: Orthopedics
Keywords: Klein's line, slipped capital femoral epiphysis (PubMed Search)
Posted: 11/7/2009 by Michael Bond, MD
(Updated: 8/31/2014)
Click here to contact Michael Bond, MD
Slipped Capital Femoral Epiphysis (SCFE)
SCFE can present as hip, thigh or knee pain in the young adolescent. Risk factors include hypogonadism, hypothyroidism, hypopituiratism, and obesity. One way to make the diagnosis is to obtain a AP view of the pelvis and draw a line(Klein's line) along the superior border of the neck of the femur. This line should intersect the femoral epiphysis. If it does not the diagnosis of SCFE can be made.
However, this is only about 40% sensitivity. Green et al recently published a study that demonstrated that if you measure the distance from Klein's line and the lateral edge of the femoral epiphysis on both sides, and the difference between the two is more than 2mm you can make the diagnosis of SCFE more accurately and sooner.

FIGURE 1. Measurement methods on an anterior-posterior radiograph of a right slipped capital femoral epiphysis. White lines indicate Klein’s line for each hip. A and B, indicate maximum epiphyseal width lateral to Klein’s line. As A is 2mm narrower than B, the right (A) hip qualifies as a slip using our modification but not Klein’s original definition.
Green DW, Mogekwu N, Scher DM, Handler S, Chalmers P, Widmann RF. A modification of Klein's Line to improve sensitivity of the anterior-posterior radiograph in slipped capital femoral epiphysis. J Pediatr Orthop. Jul-Aug 2009;29(5):449-453.
Category: Orthopedics
Keywords: Wound, Irrigation, Fibroblast (PubMed Search)
Posted: 10/31/2009 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Wound Irrigation
A recent article by Thomas et al showed that any concentration of betadiene and hydrogen peroxide used to irrigate a wound was more toxic to fibroblasts (required for wound healing) then it was to bacteria. Low concentrations of chlorhexidine remained bactericidial while having minimal affects on fibroblasts.
WIth the addition of this study the routine practice of soaking a wound in betadiene or hydrogen peroxide should be abandoned. Good irrigation with normal saline or even tap water is all that is really needed to decontaminiate a wound. If a bactericidal agent is needed then low concentrations of chlorhexidine should be used.
Thomas, GS. Mechanisms of Delayed Wound Healing by Commonly Used Antiseptics. J Trauma 2009; 66:82-91
Category: Orthopedics
Keywords: winged scapula, trapezius, serratus anterior, long thoracic nerve (PubMed Search)
Posted: 10/18/2009 by Dan Lemkin, MS, MD
(Updated: 2/8/2026)
Click here to contact Dan Lemkin, MS, MD
Winged scapula is caused by muscular injury or damage to corresponding muscular innervation. Mechanism can be due to blunt or penetating thoracic trauma.
Clinical findings include
Treatments
Category: Orthopedics
Keywords: Scaphoid Fracture, CT (PubMed Search)
Posted: 10/17/2009 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Snuff Box Tenderness:
It has become the standard of care that individuals with snuff box tenderness, or pain with axial loading of the thumb, be placed in a thumb spica splint for 1-2 weeks until follow up x-rays can be done. This is done to rule out an occult scaphoid fracture. However, this practice can be hugely inconvenient to the patient and result in some atrophy of their forearm.
An alternative approach is to obtain a CT scan through the wrist to look specifically at the scaphoid bone. If the CT scan is negative you can send them home with some pain control, RICE (Rest, Ice, Compression, Elevation) treatment and let them use thier thumb. No splint is needed. If it is positive then you can splint them and have them follow up with orthopedics or hand surgery.
Category: Orthopedics
Keywords: AC Joint, Separation, Dislocation (PubMed Search)
Posted: 9/26/2009 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
AC Joint Dislocations
The acromioclavicular (AC) Joint is commonly injured when a person falls onto their shoulder.
The AC Joint consists of three ligaments:
Injuries to this joint are classified as Type I – Type VI and involve sprain or tears of the AC or CC ligaments
Category: Orthopedics
Keywords: Monteggia's Fracture (PubMed Search)
Posted: 8/1/2009 by Michael Bond, MD
Click here to contact Michael Bond, MD
Monteggia's Fracture
Wheeless' Textbook of Orthopaedics http://www.wheelessonline.com/ortho/monteggias_fracture
Category: Orthopedics
Keywords: jones fracture,foot fracture,malunion (PubMed Search)
Posted: 6/21/2009 by Dan Lemkin, MS, MD
(Updated: 7/18/2009)
Click here to contact Dan Lemkin, MS, MD
Jones fracture
Presented with persistant foot pain from
Jones fracture malunion.
http://www.wheelessonline.com/ortho/jones_fracture
http://www.wheelessonline.com/ortho/avulsion_frx_of_base_of_5th_metatarsal
Category: Orthopedics
Keywords: Blast, hand, injuries (PubMed Search)
Posted: 7/5/2009 by Michael Bond, MD
Click here to contact Michael Bond, MD
Blast Injuries:
In honor of the 4th of July holiday, here is a quick pearl about blast injuries.
Philipson MR, Southern SJ. The blast component of firework injuries--not to be underestimated. Injury. 2004:35; 1042-1043.
