Category: Critical Care
Posted: 7/11/2018 by Ashley Menne, MD
(Updated: 8/7/2018)
Click here to contact Ashley Menne, MD
Legionella is an important cause of community-acquired pneumonia. It ranks among the three most common causes of severe CAP leading to ICU admission and carries a high mortality rate – up to 33%. Resulting from inhalation of aerosols containing Legionella species and subsequent lung infection, it is often associated with contaminated air conditioning systems, and other hot and cold water systems.
Recommended antibiotic regimens include a fluoroquinolone, either in monotherapy or combined with a macrolide (typically Levaquin +/- or Azithromycin).
A retrospective, observational study published in the Journal of Antimicrobial Chemotherapy in 2017 looked at 211 patients admitted to the ICU with confirmed severe legionella pneumonia treated with a fluoroquinolone vs a macrolide and monotherapy vs combination therapy. Combination therapy included fluoroquinolone + macrolide, fluoroquinolone + rifampicin, or macrolide + rifampicin.
Of these 211 cases, 146 (69%) developed ARDS and 54 (26%) died in the ICU. Mortality was lower in the fluoroquinolone-based group (21%) than in the non-fluoroquinolone based group (39%), and in the combination therapy group (20%) than in the monotherapy group (34%). In a multivariable analysis, fluoroquinolone-based therapy, but not combination therapy was associated with a reduced risk of mortality (HR 0.41).
Take Home Points:
-Remember, our usual blanket coverage with vanc + zosyn in the ED does not cover atypicals!
-Consider Levaquin instead of Azithro if there is clinical concern for Legionella PNA
-hyponatremia, abnormal LFTs may be clues in the appropriate context
Cecchini J, Tuffet S, Sonneville R, et al. Antimicrobial strategy for severe community-acquired legionnaires’ disease: a multicentre retrospective observational study. J Antimicrob Chemother. 2017;72(5):1502-1509. doi:10.1093/jac/dkx007.
Category: Critical Care
Posted: 6/26/2018 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Volume Responsiveness, Carotid Ultrasound, and the PLR
Gassner M, Killu K, Bauman Z, Coba V, Rosso K, Blyden D. Feasibility of common carotid artery point of care ultrasound in cardiac output measurements compared to invasive methods. Journal of Ultrasound. 2015;18(2):127-133.
Category: Critical Care
Keywords: cardiac arrest, CPR, obesity (PubMed Search)
Posted: 6/19/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Although not specifically a part of current recommendations due to lack of data, the AHA has previously recommended shifting upward on the sternum during CPR in the pulseless pregnant patient in order to account for upward displacement of the heart by a gravid uterus. Should the same be done for our obese patients?
Lee et al. performed a retrospective study that reviewed chest CTs to determine the location on the sternum that corresponded to the optimal point of maximal left ventricular diameter (OPLV), in both obese and non-obese patients.
They found that the OPLV was higher (more cranial) on the sternum for obese patients than for patients with normal weight, although 96% of obese patients' OPLV fell within 2cm of where the guidelines recommend standard hand placement should be, compared to a notable 52% in non-obese patients.
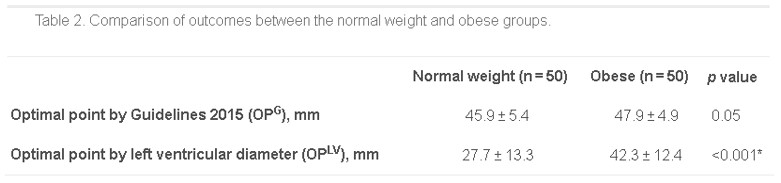
*as measured from the distal end of the sternum
Bottom Line: Radiographically, the location on the sternum that corresponds to optimal compression of the LV is more cranial in obese patients than in non-obese patients. It remains to be seen whether the recommendations for hand placement in CPR should be adjusted, but we may want to consider staying within 4cm of the bottom of the sternum in patients of normal weight.
Lee J, Oh J, Lim TH, et al. Comparison of optimal point on the sternum for chest compression between obese and normal weight individuals with respect to body mass index, using computer tomography: A retrospective study. Resuscitation. 2018; 128:1-5.
Category: Critical Care
Keywords: sepsis, septic shock, guidelines (PubMed Search)
Posted: 5/22/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD


Take Home Points:
For additional reading:
EMNerd, Dr. Rory Spiegel https://emcrit.org/emnerd/em-nerd-case-temporal-fallacy/
Surviving Sepsis Campaign http://www.survivingsepsis.org/Guidelines/Pages/default.aspx
Category: Critical Care
Posted: 5/15/2018 by Ashley Menne, MD
Click here to contact Ashley Menne, MD
Precedex (dexmedetomidine) is a selective alpha-2 adrenergic receptor agonist used as a sedative.
It is unique among sedatives typically used in the ICU in that it lacks GABA activity and lacks anticholinergic activity.
Previous studies have shown significant positive changes in sleep patterns in critically ill patients sedated with dexmedetomidine:
-improved sleep efficiency – decreased sleep fragmentation, decreased stage 1 sleep, increased stage 2 sleep
-improved distribution of sleep (with more than ¾ sleep occurring at night)
Given importance of sleep and preservation of day-night cycles/ circadian rhythms in prevention of delirium, a recent randomized controlled trial evaluated dexmedetomidine's effect on delirium.
100 delirium-free critically ill adults receiving sedatives were randomized to receive nocturnal (21:30-06:15) IV dexmedetomidine (titrated to RASS -1 or max 0.7 mcg/kg/hr) OR placebo until ICU discharge.
80% of patients in the dexmedetomidine group remained delirium-free vs 54% in the placebo group.
There was no difference in the incidence of hypotension, bradycardia, or both between groups.
Alexopolou, et al. Effects of Dexmedetomidine on Sleep Quality in Critically Ill Patients. Anesthesiology 2014; 121:801-7.
Skrobic, et al. Low Dose Nocturnal Dexmedetomidine Prevents ICU Delirium. Am J Respir Crit Care Med 2018; 197:9, 1147-56.
Category: Critical Care
Posted: 5/1/2018 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
DOACs and the Critically Ill
Stensballe J, Moller MH. Ten things ICU specialists need to know about direct oral anticoagulants (DOACs). Intensive Care Med. 2018: epub ahead of print.
Category: Critical Care
Keywords: acute hypoxic respiratory failure, intubation, noninvasive positive pressure ventilation, high flow nasal cannula, BiPAP, vapotherm (PubMed Search)
Posted: 4/25/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
ED physicians frequently utilize modailities such as noninvasive positive pressure ventilation (NIV) and high flow nasal cannula (HFNC) to support and potentially avoid intubation in patients presenting with acute hypoxic respiratory failure. Unfortunately, failure of these measures, resulting in "delayed" intubation, has been associated with increased mortality.1,2
A recent post-hoc analysis of data from a multicenter randomized controlled trial evaluated 310 patients with acute hypoxic respiratory failure managed with supplemental O2 by regular nasal cannula, HFNC, or NIV.3
The following factors were predictive of eventual intubation in the different groups:
Of note, 45% of the 310 patients eventually required intubation, and these patients in general had a higher initial respiratory rate and lower PaO2 at presentation, and were more likely to have bilateral infiltrates on CXR.
Bottom Line: Reevaluate your patients frequently. If RR remains high, P:F ratio remains low, or patient respiratory effort/work of breathing is not alleviated by noninvasive measures, consider pulling the trigger on intubation earlier.
Category: Critical Care
Posted: 4/18/2018 by Ashley Menne, MD
(Updated: 2/8/2026)
Click here to contact Ashley Menne, MD
Linezolid, an antimicrobial agent in the oxazolidinone class, often used to cover MRSA and/or VRE, is a reversible MAOI that increases the risk of serotonin syndrome, particularly when administered with other serotonergic agents.
In 2011, the US FDA issued a warning against concomitant use of Linezolid and other serotonergic agents, particularly SSRIs and SNRIs. When use of linezolid is absolutely indicated, an appropriate washout period prior to initiation was recommended.
Based on published reports and retrospective reviews, the incidence of linezolid-associated serotonin toxicity is between 0.54% and 18.2%.
A study published in the Journal of Clinical Psychopharmacology in Oct 2017 examined the incidence of serotonin syndrome with combined use of linezolid and SSRIs/SNRIs compared with linezolid alone and though there was a trend toward increased incidence in patients on SSRI/SNRIs, the authors were unable to find a statistically significant difference.
Several flaws:
-Study was retrospective
-Incidence of serotonin syndrome in both groups was very low: 1/87 (1.1%) in Linezolid + SSRI/SNRI group compared to 1/261 (0.4%) in Linezolid alone group.
-Patients in “Linezolid alone” group were not on SSRIs or SNRIs, but were allowed to be on other serotonergic medications.
Despite this study, there are many (>30) case reports of Linezolid-associated serotonin syndrome in patients taking other serotonergic agents.
Cyproheptadine (the “antidote”) is an H1 antagonist and nonspecific serotonin antagonist. A single case study published in 2016, reported successful use of cyproheptadine for prophylaxis against serotonin toxicity in a patient with schizophrenia, depression, and severe osteomyelitis requiring treatment with linezolid while on fluoxetine.
Bottom Line:
Risk of linezolid-associated serotonin syndrome may be lower than previously thought, however, it is still not recommended for use in patients taking concomitant serotonergic agents without an appropriate washout period.
In case of resistant infection with no other antibiotic treatment options, the risks and benefits of concomitant administration must be weighed seriously and providers must familiarize themselves with and be vigilant in watching for signs/symptoms of serotonin toxicity.
In situations where use of linezolid is unavoidable in patients on concomitant serotonergic agents, prophylactic cyproheptadine may be considered.
Karkow DC, Kauer JF, Ernst EJ. Incidence of Serotonin Syndrome With Combined Use of Linezolid and Serotonin Reuptake Inhibitors Compared With Linezolid Monotherapy. J Clin Psychopharmacol. 2017;37(5):518-523. doi:10.1097/JCP.0000000000000751.
Deardorff OG, Khan T, Kulkarni G, Doisy R, Loehr C. Serotonin Syndrome: Prophylactic Treatment With Cyproheptadine. Prim Care Companion CNS Disord. 2016;18(4). doi:10.4088/PCC.16br01966.
Woytowish MR, Maynor LM. Clinical Relevance of Linezolid-Associated Serotonin Toxicity. Ann Pharmacother. 2013;47(3):388-397. doi:10.1345/aph.1R386.
Ramsey TD, Lau TT, Ensom MH. Serotonergic and Adrenergic Drug Interactions Associated with Linezolid: A Critical Review and Practical Management Approach. Ann Pharmacother. 2013;47(4):543-560. doi:10.1345/aph.1R604.
Category: Critical Care
Posted: 4/3/2018 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Acute on Chronic Liver Failure
Fuhrmann V, Whitehouse T, Wendon J. The ten tips to manage critically ill patients with acute-on-chronic liver failure. Intensive Care Med. 2018.
Category: Critical Care
Keywords: sepsis (PubMed Search)
Posted: 3/31/2018 by Ashley Martinelli
(Updated: 2/8/2026)
Click here to contact Ashley Martinelli
Bottom Line: Implement sepsis protocols as soon as sepsis is suspected prior to the end of the 3 hour treatment window.
Category: Critical Care
Keywords: cardiac arrest, OHCA, ROSC, targeted temperature management, oxygen, hyperoxia (PubMed Search)
Posted: 3/27/2018 by Kami Windsor, MD
(Updated: 2/8/2026)
Click here to contact Kami Windsor, MD
Background:
Animal studies in post-ROSC management after cardiac arrest have repeatedly demonstrated poorer neurological outcomes with higher amounts of oxygen administration.1 Studies in humans have also demonstrated dose-dependent associations between hyperoxia and poorer neurologic outcomes, as well as in-hospital mortality.2,3
Recent Data
A retrospective analysis of prospectively-collected data in 187 OHCA patients undergoing postarrest care with targeted temperature management found worse neurologic outcomes in patients experiencing hyperoxia in the first 6 hours following ROSC.4
This association was dose-dependent, with worsening outcomes as with higher PaO2 levels >200.
Bottom Line:
Category: Critical Care
Posted: 3/21/2018 by Ashley Menne, MD
Click here to contact Ashley Menne, MD
Worsening hypoxemia is not uncommon upon initiation of VV ECMO for severe ARDS as tidal volumes drop to double digits (often <20cc) after transition to “lung rest” ventilator settings. The following are strategies to improve peripheral oxygenation:
1. Increase the blood’s oxygen content
- Ensure FIO2 of ECMO sweep gas is 1
- Increase ECMO blood flow
o Limited by cannula size and configuration – may require placement of additional venous drainage cannula
o Also limited by greater risk of recirculation and hemolysis
- Increase blood oxygen-carrying capacity
o Transfuse PRBCs – some advocate for goal hemoglobin 12-14, though institutional practices vary significantly
2. Minimize recirculation
- Maximize distance between drainage and return cannulae
3. Reduce oxygen consumption
- Optimize sedation and neuromuscular blockade. (This is not the appropriate scenario for awake ECMO.)
- Consider therapeutic hypothermia
4. Decrease cardiac output and intrapulmonary shunt
- Consider beta blocker (esmolol) infusion
- Prone positioning (only if staff are experienced with proning on ECMO as this poses significant risk of cannula displacement)
5. Consider switching to hybrid configuration (VVA – continued venous drainage cannula and venous return cannula with addition of arterial return cannula)
Montisci A, Maj G, Zangrillo A, Winterton D, Pappalardo F. Management of Refractory Hypoxemia During Venovenous Extracorporeal Membrane Oxygenation for ARDS. ASAIO J. 2015;61(3):227-236. doi:10.1097/MAT.0000000000000207.
Category: Critical Care
Posted: 3/20/2018 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Peri-Intubation Cardiac Arrest
De Jong A, et al. Cardiac arrest and mortality related to intubation procedure in critically ill adult patients: A multicenter cohort study. Crit Care Med. 2018; 46:532-9.
Category: Critical Care
Keywords: ICU, fungal infection, septic shock, antifungal therapy, empiric (PubMed Search)
Posted: 2/27/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Which septic patients should receive empiric antifungal therapy?
Patients with fungemia only make up about 5% of patients presenting with septic shock, but invasive fungal infections are associated with increased hospital mortality (40-50%), prolonged ICU and hospital length of stay, and increased costs of care.1
The EMPIRICUS trial showed no mortality benefit to empiric antifungals for all, even patients with candidal colonization and recent exposure to antibiotics.2
Bottom Line
Therapy should always be tailored to the specific patient, but providers should strongly consider admininistering empiric echinocandin (micafungin, caspofungin) over fluconazole in patients with severe sepsis/septic shock and:
*Especially consider addition of antifungal in patients who do not show improvements after initial management with IVF and broad spectrum antibiotics in the ED.*
Which septic patients should receive empiric antifungal therapy?
Patients with fungemia only make up about 5% of patients presenting with septic shock, but invasive fungal infections are associated with increased hospital mortality (40-50%), prolonged ICU and hospital length of stay, and increased costs of care.1
The EMPIRICUS trial showed no mortality benefit to empiric antifungals for all, even patients with candidal colonization and recent exposure to antibiotics. (It demonstrated decreased rate of new invasive fungal infection, but did not increase survival).2
Risk factors for invasive fungal infections include:3
Which antifungal agent should we use?
Although older studies have not shown benefits to echinocandin, such as micafungin, over fluconazole as initial empiric antifungal therapy,4,5 a recent study by Garnacho-Montero et al. demonstrated improved 30 and 90-day mortality in patients with candidemia whose initial antibiotic was an echinocandin rather than fluconazole.6
Category: Critical Care
Posted: 2/21/2018 by Ashley Menne, MD
Click here to contact Ashley Menne, MD
-Nonischemic cardiomyopathy, classically seen in post-menopausal women preceded by an emotional or physical stressor
-Named for characteristic appearance on echocardiography and ventriculography with apical ballooning and contraction of the basilar segments of the LV – looks like a Japanese octopus trap or “takotsubo" (pot with narrow neck and round bottom)
-Clinical presentation usually similar to ACS with chest pain, dyspnea, syncope, and EKG changes not easily distinguished from ischemia (ST elevations – 43.7%, ST depressions, TW inversions, repol abnormalities) and elevation in cardiac biomarkers (though peak is typically much lower than in true ACS)
** Diagnosis of exclusion – only after normal (or near-normal) coronary angiography **
-Care is supportive and prognosis is excellent with full and early recovery in almost all patients (majority have normalization of LVEF within 1 week)
-Supportive care may include inotropes, vasopressors, IABP, and/or VA ECMO in profound cardiogenic shock
** LVOT Obstruction **
-occurs in 10-25% of patients with Takotsubo’s cardiomyopathy
-LV mid and apical hypokinesis with associated hypercontractility of basal segments of the LV predisposes to LV outflow tract obstruction
-Important to recognize as it is managed differently:
-may be worsened by hypovolemia, inotropes, and/or systemic vasodilatation
-mainstay of treatment is avoidance of the above triggers/exacerbating factors while increasing afterload
*phenylephrine is agent of choice +/- beta blockade
Take Home Points:
***Diagnosis of exclusion!!! Presentation very similar to ACS and ACS MUST be ruled out
* Treatment is supportive and similar to usual care for cardiogenic shock. Can be severe and require mechanical circulatory support!
*10-25% have LVOT obstruction. Manage with phenylephrine +/- beta blockade
Weiner MM, Asher DI, Augoustides G, et al. Takotsubo Cardiomyopathy?: A Clinical Update for the Cardiovascular Anesthesiologist. J Cardiothorac Vasc Anesth. 2017;31(1):334-344. doi:10.1053/j.jvca.2016.06.004.
Category: Critical Care
Posted: 2/6/2018 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Hyperoxia and the Post-Arrest Patient
Roberts BW, et al. Association between early hyperoxia exposure after resuscitation from cardiac arrest and neurological disability: a prospective multi-center protocol-directed cohort study. Circulation 2018; epub ahead of print.
Category: Critical Care
Keywords: sepsis, septic shock, glucocorticoids, steroids, hydrocortisone (PubMed Search)
Posted: 1/29/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
As hospital volumes increase and ED patient boarding becomes more commonplace, emergency physicians may find themselves managing critically ill patients beyond the initial resuscitation.
The benefit of glucocorticoids in critically ill patients with septic shock has remained a topic of controversy for decades due to conflicting studies, including the 2002 Annane trial and the 2008 CORTICUS trial, which had opposing results when it came to the mortality benefit of steroids.
The results of the eagerly-awaited ADRENAL trial, a multicenter randomized controlled trial investigating the benefit of steroids in septic shock, were released earlier this month:
Take Home Points:
1. Administration of standard daily dose hydrocortisone by infusion does not seem to affect mortality in septic shock.
2. Emergency providers should continue to consider stress-dose steroids in patients with shock and a high risk of adrenal insufficiency (e.g., chronic steroid therapy, genetic disorders, infectious adrenalitis, etc).
Category: Critical Care
Posted: 1/9/2018 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Septic Cardiomyopathy
Beesley S, et al. Septic cardiomyopathy. Crit Care Med 2018. [epub ahead of print]
Category: Critical Care
Keywords: endotracheal intubation, cardiac arrest, airway, respiratory failure (PubMed Search)
Posted: 1/2/2018 by Kami Windsor, MD
(Updated: 1/4/2018)
Click here to contact Kami Windsor, MD
Although the data is limited, current published rates of in-hospital, non-operating room peri-intubation cardiac arrest (PICA) range from 2 to 6%.1,2,3
Several risk factors associated with PICA have been identified and include:
Other common findings:
Bottom Line: Endotracheal intubation is one of the riskiest procedures we regularly perform as emergency physicians.
References
1. Heffner AC, Swords DS, Neale MN, Jones AE. Inicidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation. 2013; 84(11):1500-4.
2. Kim WY, Kwak MK, Ko BS, et al. Factors associated with the occurrence of cardiac arrest after emergency tracheal intubation in the emergency department. PLoS One. 2011; 9(11):e112779.
3. Wardi G, Villar J, Nguyen T, et al. Factors and outcomes associated with inpatient cardiac arrest following emergent endotracheal intubation. Resuscitation. 2017; 121:76-80.
Category: Critical Care
Posted: 12/12/2017 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Sedating The Critically Ill Patient
Metha S, et al. What's New in Intensive Care: Ten Tips for ICU Sedation. Intensive Care Med 2017. [epub ahead of print].
