Category: Visual Diagnosis
Posted: 5/19/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A patient presents with the rash shown below and is treated with penicillin. Fever, headache, and myalgia develop four hours later. What’s the diagnosis?

Answer: Jarisch-Herxheimer reaction
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 5/13/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Prior literature has demonstrated the safety and feasibility of placing subclavian lines with ultrasound guidance; here's a link to a short educational video describing the technique.
The literature has been varied, however, as to which approach is best for venous cannulation with ultrasound; the supraclavicular (SC) or infraclavicular (IC) approach (see references below)
A recent study evaluated both approaches in healthy volunteers in order to determine which approach is superior for cannulation using ultrasound.
98 patients were prospective evaluated by Emergency Medicine physicians with training in ultrasound. In each patient, both SC and IC views were evaluated on both the left and right sides; each view was given a grade for ease of favorability (no patients were actually cannulated)
Overall, it was found that the SC view was significantly more favorable compared to the IC view; the right SC was non-significantly preferred compared to the left SC.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Stachura, M. et al. A Comparison of the Supraclavicular and Infraclavicular Views for Imaging the Subclavian Vein with Ultrasound. The American Journal of Emergency Medicine (in press)
Fragou, M., Gravvanis, A., and Vasilios, D. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: A prospective randomized study. Crit Care Med. 2011; 39: 1607–1612
Mallin, M., Louis, H., and Madsen, T. A novel technique for ultrasound-guided supraclavicular subclavian cannulation. Am J Emerg Med. 2010; 28: 966–969
Czarnik, T., Gawda, R., Perkowski, T. et al. Supraclavicular approach is an easy and safe method of subclavian vein catheterization even in mechanically ventilated patients. analysis of 370 attempts. Anesthesiology. 2009; 111:334–339
Category: Visual Diagnosis
Posted: 5/5/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The clip below demonstrates normal right femoral anatomy. The structure with the asterisk is the right common femoral vein and the arrow is pointing to a branch of the right femoral vein. What is the name of the branch and what is its importance during lower extremity ultrasound?
Answer: Greater Saphenous Vein; it is one of the two regions that should be compressed when evaluating for a lower extremity DVT in the Emergency Department (the other is at the trifurcation of the popliteal vein).
Here is a podcast from the Ultrasound Podcast describing the entire bedisde DVT exam http://www.ultrasoundpodcast.com/2011/08/dvt/
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)a
Category: Visual Diagnosis
Posted: 4/28/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
66 year-old female presents with one week of epigastric and right flank pain. Urinalysis was normal. What’s the diagnosis?

Answer: Choledocholithiasis with pancreatitis secondary to 2.2 cm common bile duct stone
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 4/15/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Only 50% of hemodynamically unstable patients will improve their hemodynamics in response to a fluid bolus. However, because excessive fluid administration can lead to organ edema and dysfunction, it is important to give hemodynamically unstable patients only the necessary amount of fluids to improve their hemodynamics.
There are two general categories of assessing a patient's response to volume administration; static and dynamic assessments (see referenced article below):
Static assessment (generally unreliable, but traditionally used):
Physical exam (dry mucus membranes, cool extremities, etc.)
Urine output
Blood pressure
Central venous pressure via central-line
Dynamic assessment (more reliable but more labor intensive)
Pulse Pressure Variation
IVC Distensibility Index
End-expiratory occlusion test
Passive Leg-Raise
There is no simple way to accurately determine the need for a fluid bolus however the integration of the techniques above can help the clinician make better decisions.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 4/14/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
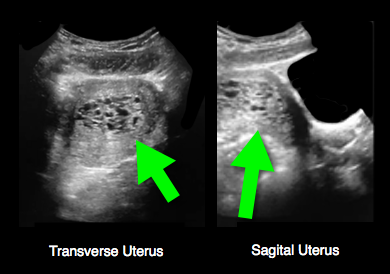
25 year-old female (G1P1) presents with 3 weeks of vaginal bleeding. Her serum beta-HCG is 65,000. Her bedside ultrasound is below; what's the diagnosis?
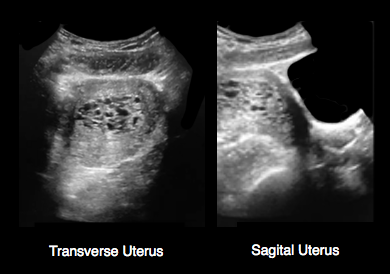
Answer: Hydatidiform mole (molar pregnancy)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 4/7/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
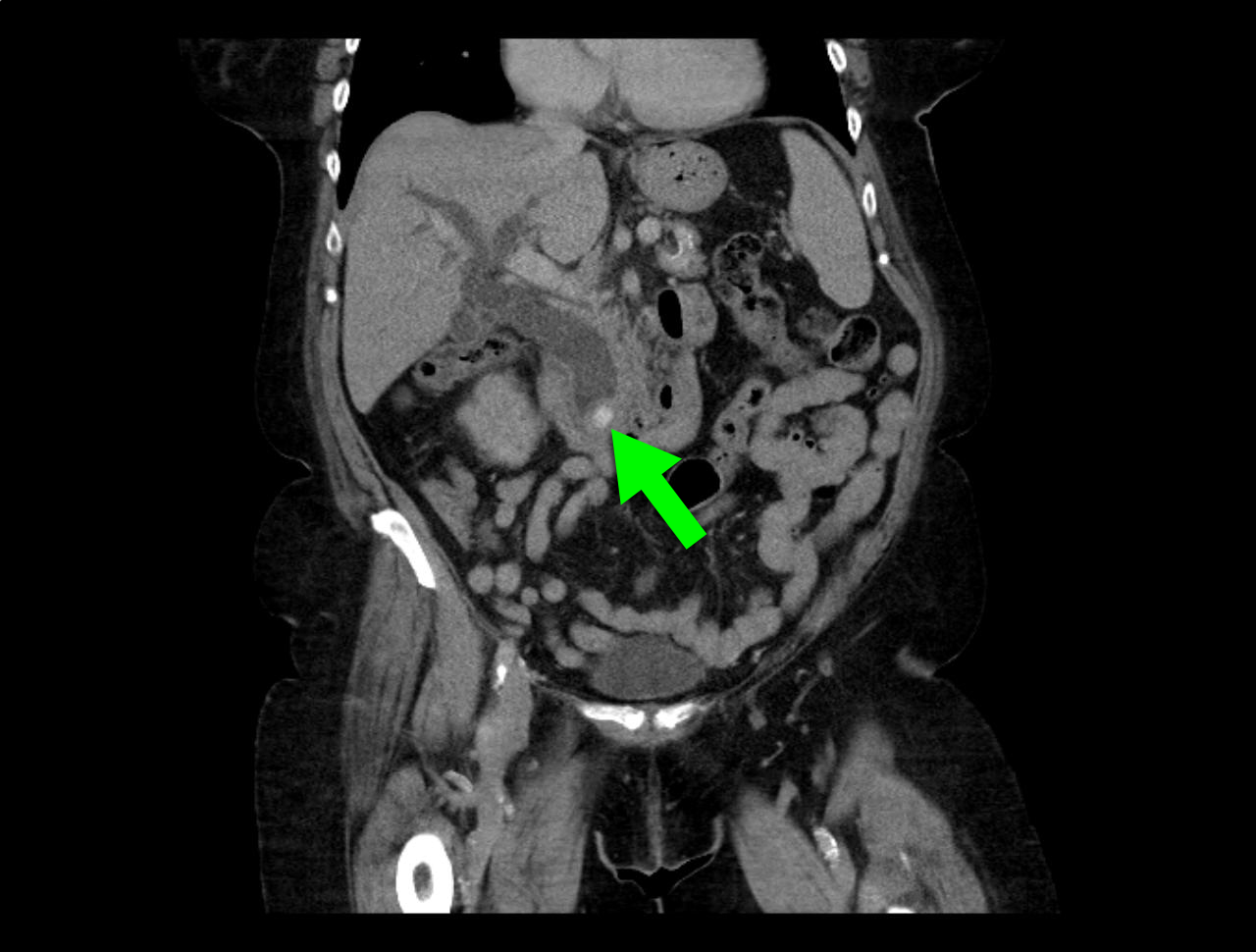
23 year-old female presents complaining of progressive right lower quadrant pain after doing "vigorous" pushups. CT abdomen/pelvis below. What’s the diagnosis? (Hint: it’s not appendicitis)

Answer: Rectus sheath hematoma
Rectus Sheath Hematoma (RSH)
Rectus muscle tear causing damage to the superior or inferior epigastric arteries with subsequent bleeding into the rectus sheath; uncommon cause of abdominal pain but mimics almost any abdominal condition.
May occur spontaneously, but suspect with the following risk factors:
Typically a self-limiting condition, but hypovolemic shock may result from significant hematoma expansion.

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/31/2014 by Haney Mallemat, MD
(Updated: 4/1/2014)
Click here to contact Haney Mallemat, MD
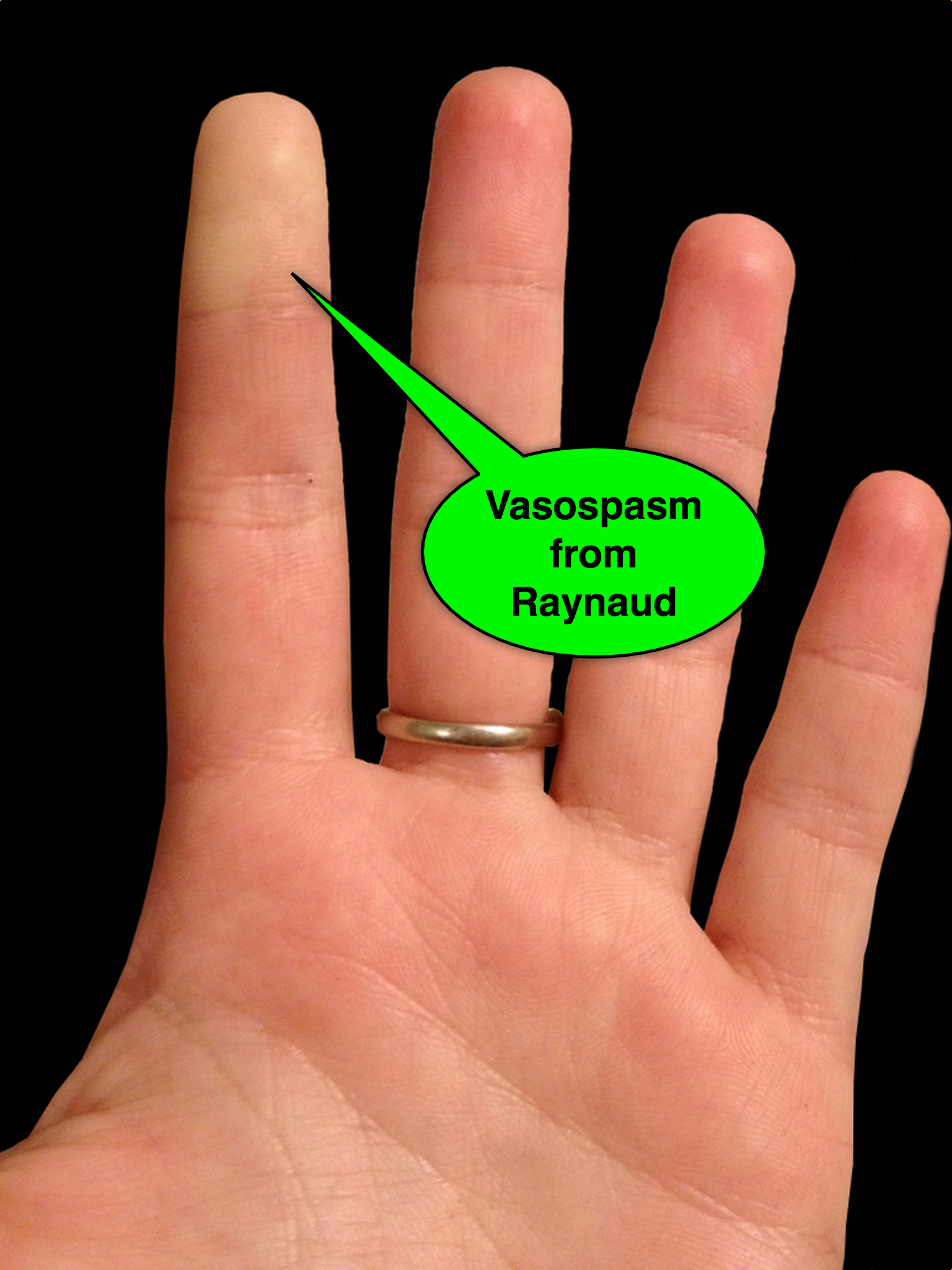
25 year-old female presents with the following. It seems to have occurred spontaneously and spontaneously resolves during her ED evaluation.

Answer: Raynaud phenomenon
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 3/19/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
In 2001, Rivers et al. published a landmark article demonstrating an early-goal directed protocol of resuscitation that reduced mortality in septic Emergency Department patients.
Many questions have arisen throughout the years with respect to that trial; critics have complained about the overwhelming change in clinical practice based on this one single-center randomized trial.
Challenging Rivers data are the ProCESS (Protocolized Care for Early Septic Shock) investigators, who released the results from a multi-center randomized control trial of 1351 septic Emergency Department patients; the primary end-point was 60-day mortality. Click here for NEJM article.
Patients in this trial were randomized to one of three groups:
Protocol-based EGDT
Protocol-based standard (did not require central lines, inotropes, or blood transfusions
Usual care (no specific protocol; care was left to the bedside clinicians)
Bottom-line: The investigators did not find any difference in mortality between patients in the three groups and comment that the most important aspects of managing the septic patient may be prompt recognition and early treatment with IV fluids and antibiotics.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/17/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
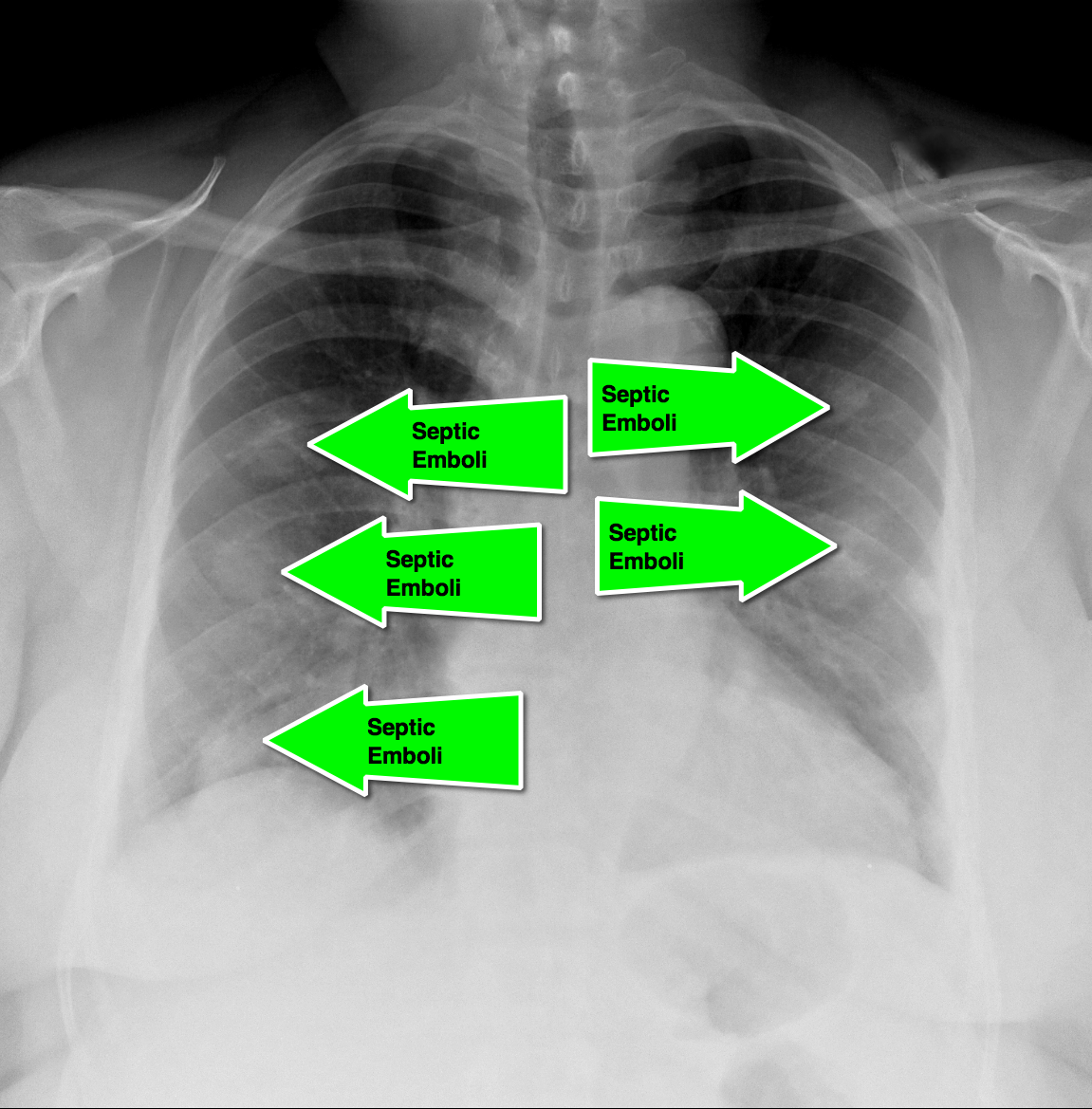
62 year-old male presents with weakness, chills, cough, and malaise. Recently, he had four teeth extracted but felt fine immediately after the extraction. Past medical history includes diabetes and hypertension; CXR is below. What’s the diagnosis?

Answer: Septic pulmonary emboli (a.k.a. pulmonary puffballs); he was eventually diagnosed with bacterial endocarditis.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/14/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
35 year-old carpet-layer presents with swelling of the superior portion of his knee that has progressively gotten worse over one week. He has no fever and has full range of motion (although pain is worse with movement). The knee is not tender to touch and the area is not erythematous or warm. What's the diagnosis?

Answer: Pre-patellar bursitis
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/3/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
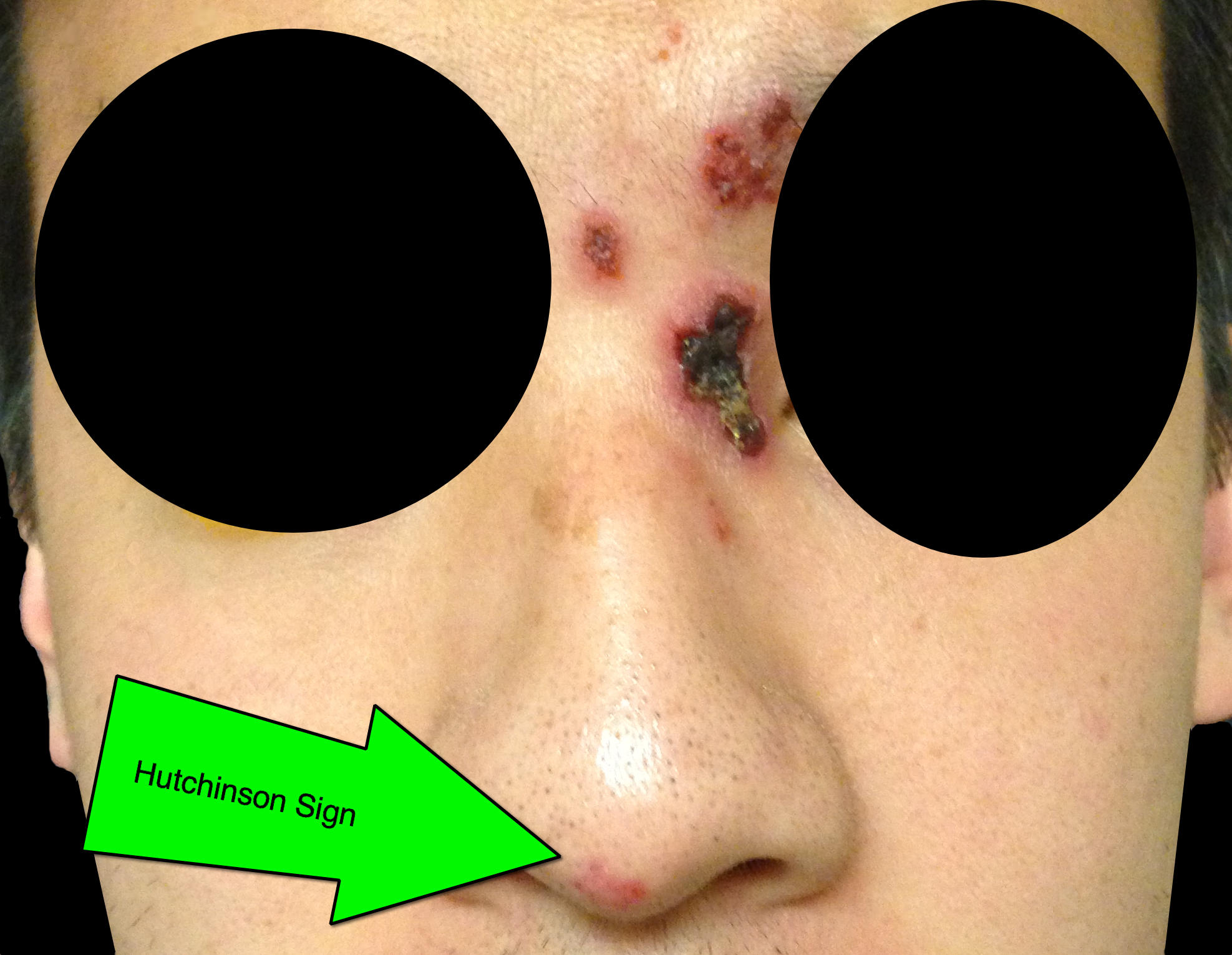
32 year-old male presents with the following. What's the diagnosis?

Answer: Hutchinson's Sign
Herpes zoster ophthalmicus (HZO)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/24/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
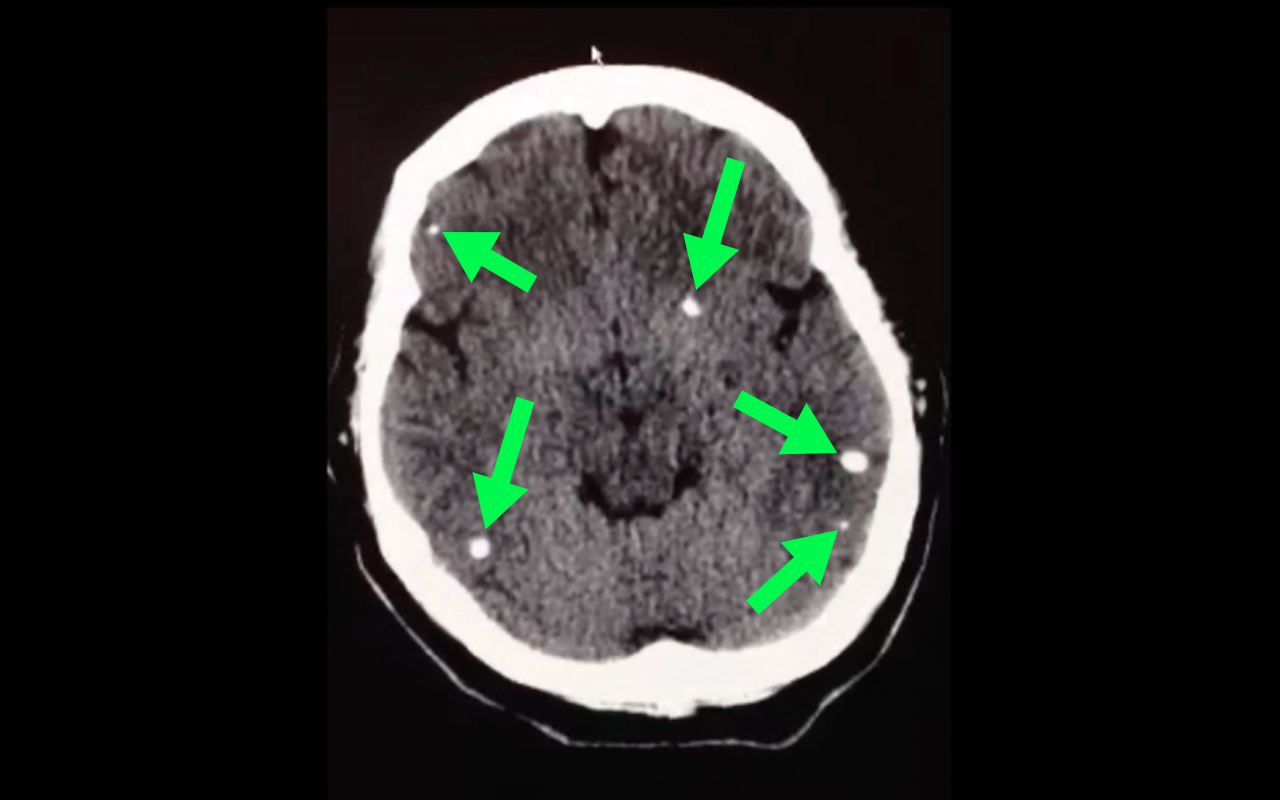
50 year-old with facial weakness and dysarthria. What's the diagnosis?
Stroke secondary to neurocysticercosis
Neurocysticercosis
Neurocysticercosis occurs secondary to ingestion of eggs from the Taenia solium tapeworm; ingestion typically occurs from ingestion of contaminated food.
Most patients are asymptomatic but symptoms of neurocysticercosis may include
Diagnosis is made via imaging such as CT scan; findings may vary depending on what stage of life the parasite is in (e.g., larvae); lumbar puncture should also be performed if the diagnosis is suspected.
Management should be symptomatic (e.g., seizures receive anticonvulsants) as well as eradication of the active parasites using steroids followed by albendazole (anti-parasitic drug)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 2/18/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Zimmerman, J.Cocaine intoxication. Crit Care Clinics 2012 Oct;28(4):517-26
Category: Visual Diagnosis
Posted: 2/17/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
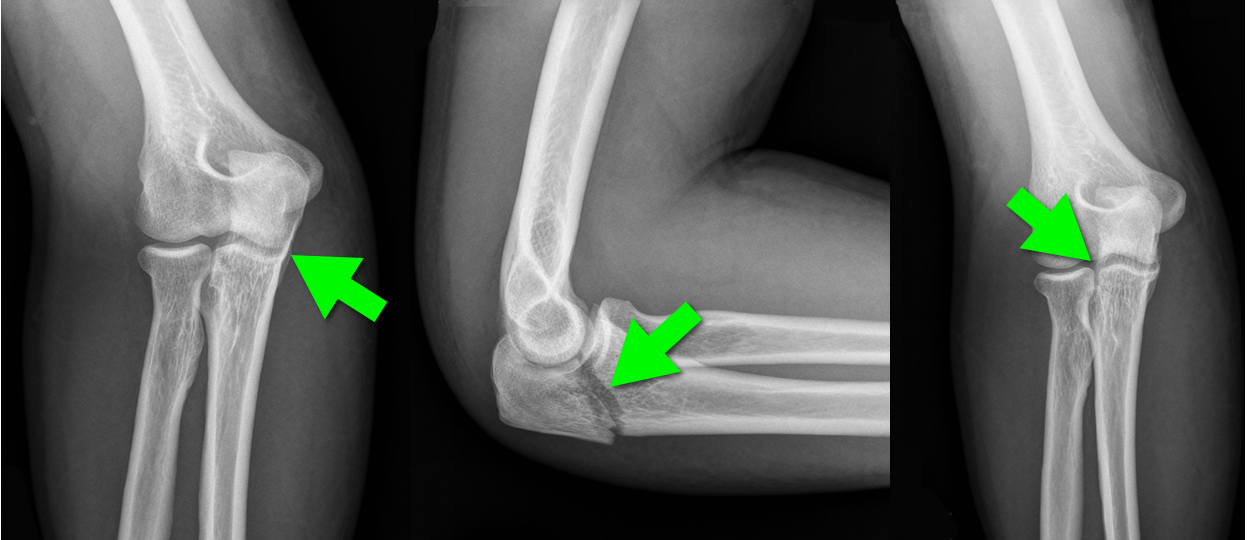
44 year-old construction worker fell off a ladder and presents with elbow pain. What's the diagnosis and what is the most commonly associated nerve injury?

Olecranon fracture; the ulnar nerve is most commonly injured
Pearls for Olecranon Fracture
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/9/2014 by Haney Mallemat, MD
(Updated: 2/10/2014)
Click here to contact Haney Mallemat, MD
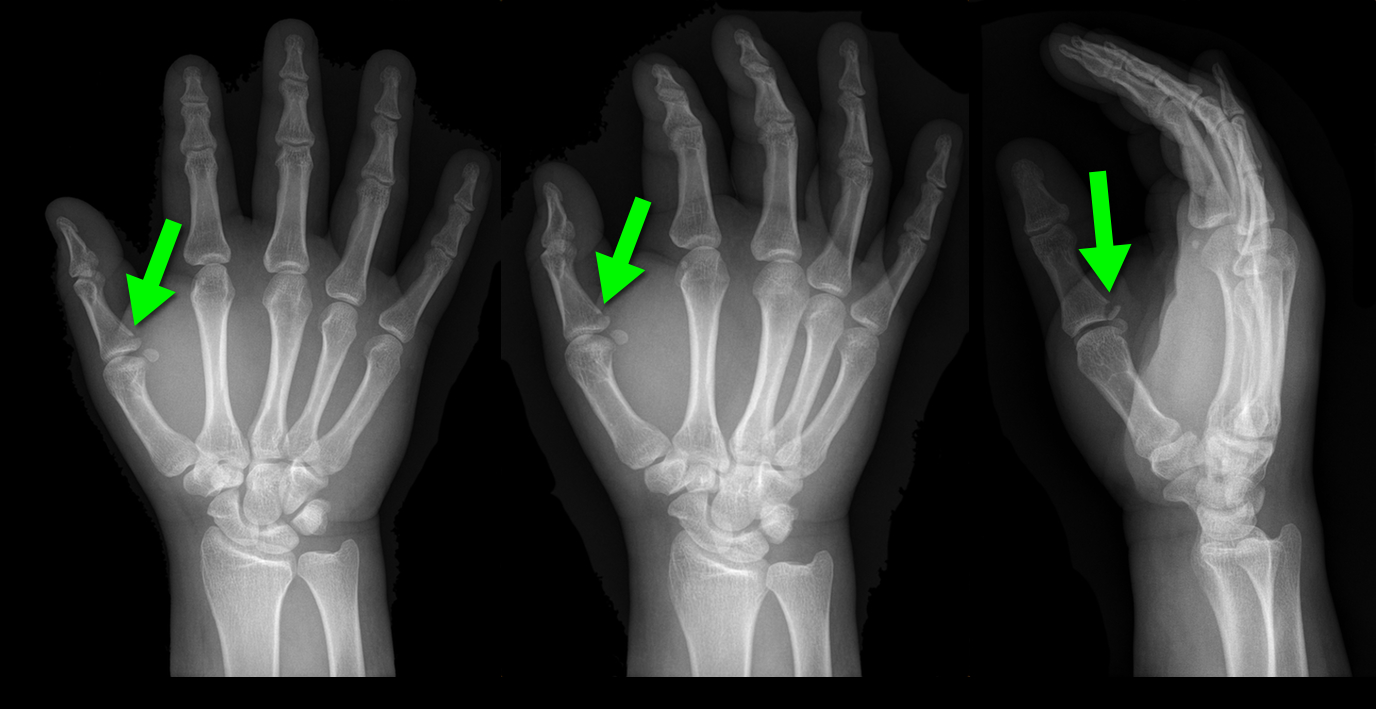
25 year-old male presents after falling off his bicycle. He complains of pain in his right-hand (he is right-hand dominant). What's the diagnosis?

Answer: Gamekeeper's thumb or Skier's thumb
Injury to the ulnar collateral ligament (UCL) secondary
Called “Gamekeeper Thumb” because injury was originally described in gamekeepers who job was to break the necks of captured game (or animals). The act of breaking necks led to a repetitive stress and injury secondary to the valgus forces on the thumb.
UCL can become torn or avulsed from the insertion on the proximal phalanx; the UCL is an important stabilizer of the thumb; improper management can lead to future disability.
Treatment is with a short-arm thumb-spica cast and follow up with a hand surgeon to determine whether management will be conservative or operative.
Chuter GS, Muwanga CL, Irwin LR (June 2009). "Ulnar collateral ligament injuries of the thumb: 10 years of surgical experience". Injury 40 (6): 652–6 Wheeless' Textbook of Orthopaedics Online: Surgical treatment of acute gamekeeper's thumb
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 2/3/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
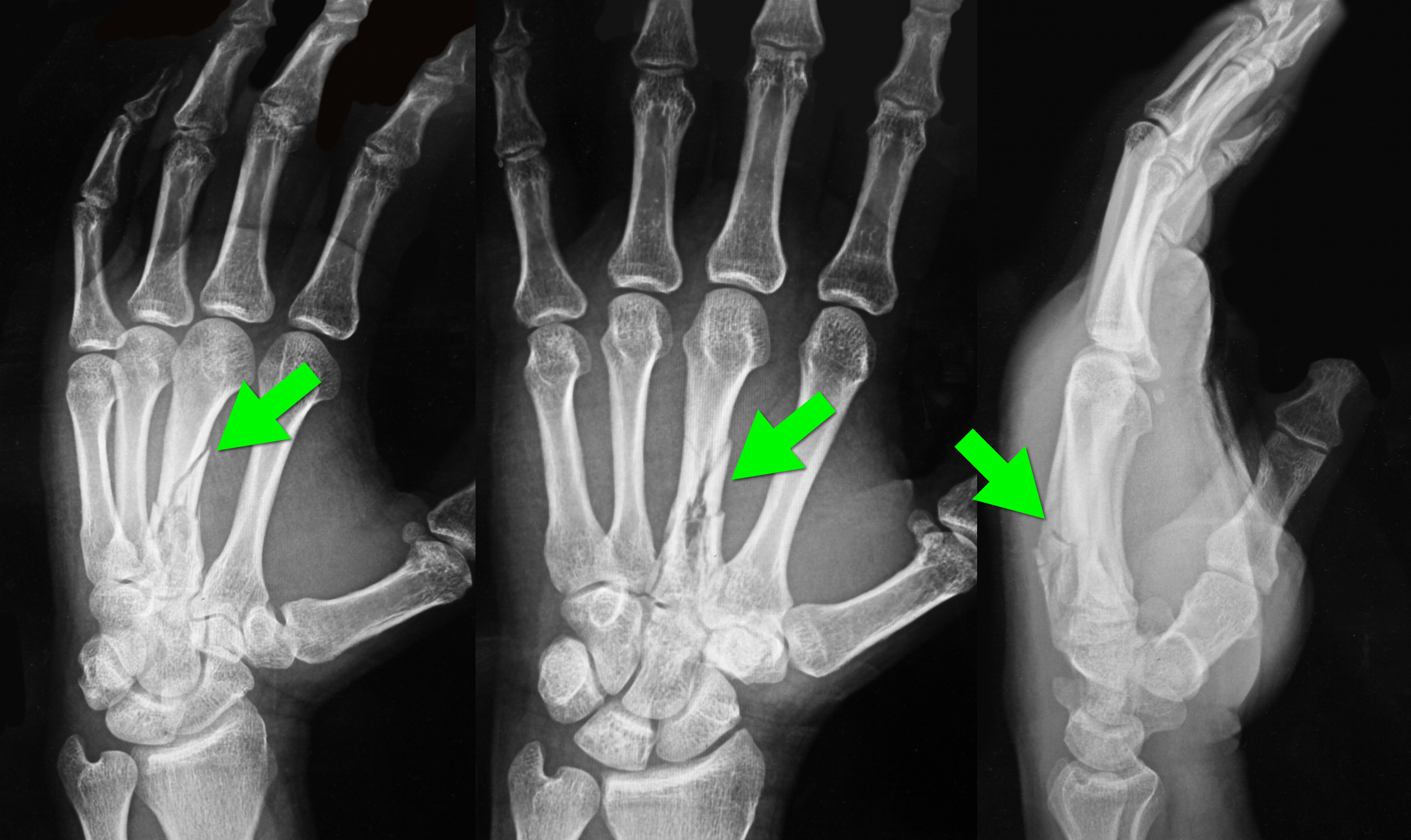
34 year-old left-hand dominant male sustained injury to left hand after his pressurized greasing-gun discharged into the palm of his hand. He has a small lac to the hand but is in extreme pain. On exam his hand is very puffy and he is neurovascularly intact (XR below) What is the next step in management?

Metacarpal fracture; emergent surgical consult is required
High-Pressure Injection Injuries (HPI) injuries
HPI devices (e.g., grease, paint guns, etc.) may cause injury when the device accidently discharges, typically into the operator’s dominant hand during attempts to clean the nozzle.
Injuries may initially appear benign, however injuries should be considered surgical emergencies because they often require debridement / washout of materials injected into deeper tissues.
Tissue damage is multi-factorial and includes direct injury (e.g., high-pressure tissue damage, vascular compression, etc.) and indirect injury from material injected into tissues (e.g., chemical inflammation / injury, granuloma formation, deep-tissue infections, etc.).
Radiographs may assist surgical planning by identifying subcutaneous air, debris, or unanticipated fractures.
Treatment:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Critical Care
Posted: 1/28/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
NSSTIs occur secondary to toxin-secreting bacteria; NSSTIs are surgical emergencies with a high-morbidity / mortality
Risk factors: immunocompromised host (DM, AIDS, etc.), intravenous drug use, malnourishment, peripheral vascular disease
Type I (polymicrobial; most common), Type II (monomicrobial; typically clostridia, streptococci, staph, or bacteroides), Type III (Vibrio vulnificus; seawater exposure)
Signs / Symptoms: pain out of proportion to exam (occasionally no pain at all), skin findings (blistering / bullae, gray-skin discoloration, or “Dishwater-like” discharge), or systemic toxicity (altered mental status, elevated lactate, etc.)
Diagnostic radiology
Treatment is emergent surgical debridement with simultaneous hemodynamic resuscitation PLUS broad-spectrum antibiotics; consider clindamycin becuase it has anti-toxin activity
Adjunctive therapies include Intravenous intraglobulin (neutralizes toxins secreted by bacteria) and hyperbaric oxygen
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/27/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
32 year-old with diabetes presents with fever, erythema, and warmth of his lower extremity; his leg is not particularly painful. He is diagnosed with cellulitis, started on antibiotics, and admitted to the hospital. While boarding in the Emergency Department he becomes rigorous and hypotensive. An ultrasound of his cellulitis is performed and is shown below. What’s the diagnosis?
"Cobblestoning" of subcutaneous tissue consistent with cellulitis. There are also areas of subcutaneous air raising the concern for necrotizing fasciitis.
Special thanks to Dr. Mike Mallin from the Ultrasound Podcast for the clip. Want to see more amazing ultrasound clips? Check out Sonocloud
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 1/20/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
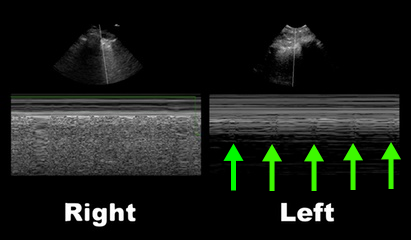
50 year-old male intubated for respiratory distress. Ultrasound is used post-intubation to confirm tube placement and the following images are obtained. What's the diagnosis?
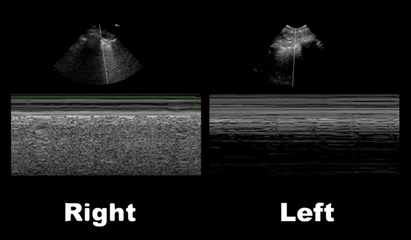
Right main-stem intubation as demonstrated by presence of lung-pulse on the left side
Lung-Pulse
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
