Category: Critical Care
Posted: 8/14/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Femoral venous access is typically limited to the acute resuscitation of critically-ill patients. Several practice-guidelines recommend avoiding the femoral site, or removal once admitted to the ICU, because of the risk of catheter-related bloodstream infection (CRBI) and deep-vein thrombosis (DVT).
A recent systematic review and meta-analysis (including two randomized-control trials and eight cohort-studies) evaluated the risk of CRBI and DVT for catheters placed in either the internal jugular, subclavian, or femoral-venous sites. No difference in the rate of CRBI or DVT was found between the three sites, although the DVT data was less robust (i.e., contained heterogeneous data).
The authors hypothesized that improvements in sterility during central-line placement (e.g., full-barrier precautions), improved nursing care (e.g., central-line site care), and ultrasound guidance may have led to a reduction in femoral site complications.
Although a prospective randomized-control trial is necessary to confirm these results, this meta-analysis challenges the traditional teaching that femoral central-access should be avoided.
Marik, P. et al. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: A systematic review of the literature and meta-analysis Crit Care Med. 2012 Aug;40(8):2479-85.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 8/13/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Placement of central-lines through the subclavian (SC) route has several advantages over other sites of venous cannulation:
• Lower rates of infection
• Lower rates of deep vein thrombosis
Placing a central-line through the "blind" SC approach increases the risk of non-compressible vessel injury and pneumothorax as compared to other approaches (e.g. internal jugular).
Ultrasound can help place central-lines in the SC vein while reducing the risk of complications; this video demonstrates the technique: http://ultrarounds.com/Ultrarounds/Subclavian_Ultrasound.html
Fragou, M. et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011 Jul;39(7):1607-12.
Category: Visual Diagnosis
Posted: 8/5/2012 by Haney Mallemat, MD
(Updated: 8/6/2012)
Click here to contact Haney Mallemat, MD

Answer: Mandibular dislocation...and the Gromis method?
• The Gromis method (a.k.a. the "Masseteric Massage" technique) is an alternative method for reducing mandibular dislocations.
• Firm, direct, and constant pressure is applied bilaterally to the masseter muscles, which relaxes the muscles (i.e., reduces spasm) and allows mandibular reduction with less traction than traditional reduction techniques and with no procedural sedation.
• Rob Orman (@emergencypdx) posts a video of Dr. Daniel Gromis demonstrating the technique: http://vimeo.com/46453741
• Finally, UMEM pearl regulars may recognize this Xray from a post last year where we described another alternative method to reduce mandibular dislocations. Here it is again: http://www.youtube.com/watch?v=Kp8AzHIC0hM
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Critical Care
Posted: 7/31/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Crystalloids (i.e., 0.9% saline and lactated ringers) have been used during resuscitation for more than a century. Their invention, however, was more accidental than intentional.
Crystalloids were first used during the European Cholera epidemic of 1831. Hartog Hamburger later modified this solution in 1896 to the solution we know today as "normal" saline. Hamburger's solution was only intended for in vitro study of RBC lysis and was never intended for clinical use.
Around this time, Sydney Ringer was testing several fluids to use for physiologic studies. Ringer's lab assistant was erroneously substituting tap water for distilled water when preparing these solutions. Ringer later discovered that this tap water contained minerals making the solution "physiologic", isotonic, and safe for human use; Alexis Hartmann later added sodium lactate to create Ringer's Lactate.
Since the invention of crystalloids, many types of resuscitation fluids have been created and studied (i.e., albumins, gelatins, and starches); all have been shown to be more expensive, with no more benefit, and with possibly more harm when compared to crystalloids.
The "perfect" resuscitation fluid still alludes us today, but of all of the solutions marketed crystalloids are arguably the best...despite their accidental history.
Awad, S. et al. The history of 0.9% saline. Clinical Nutrition 2008 Apr;27(2):179-88.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/30/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
25 year-old male was struck by a car while crossing the street. Chest X-ray and CT Chest with 3D reconstruction are shown below. What's the diagnosis?


Answer: Aortic dissection / transection
Blunt Aortic Injury

Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/23/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
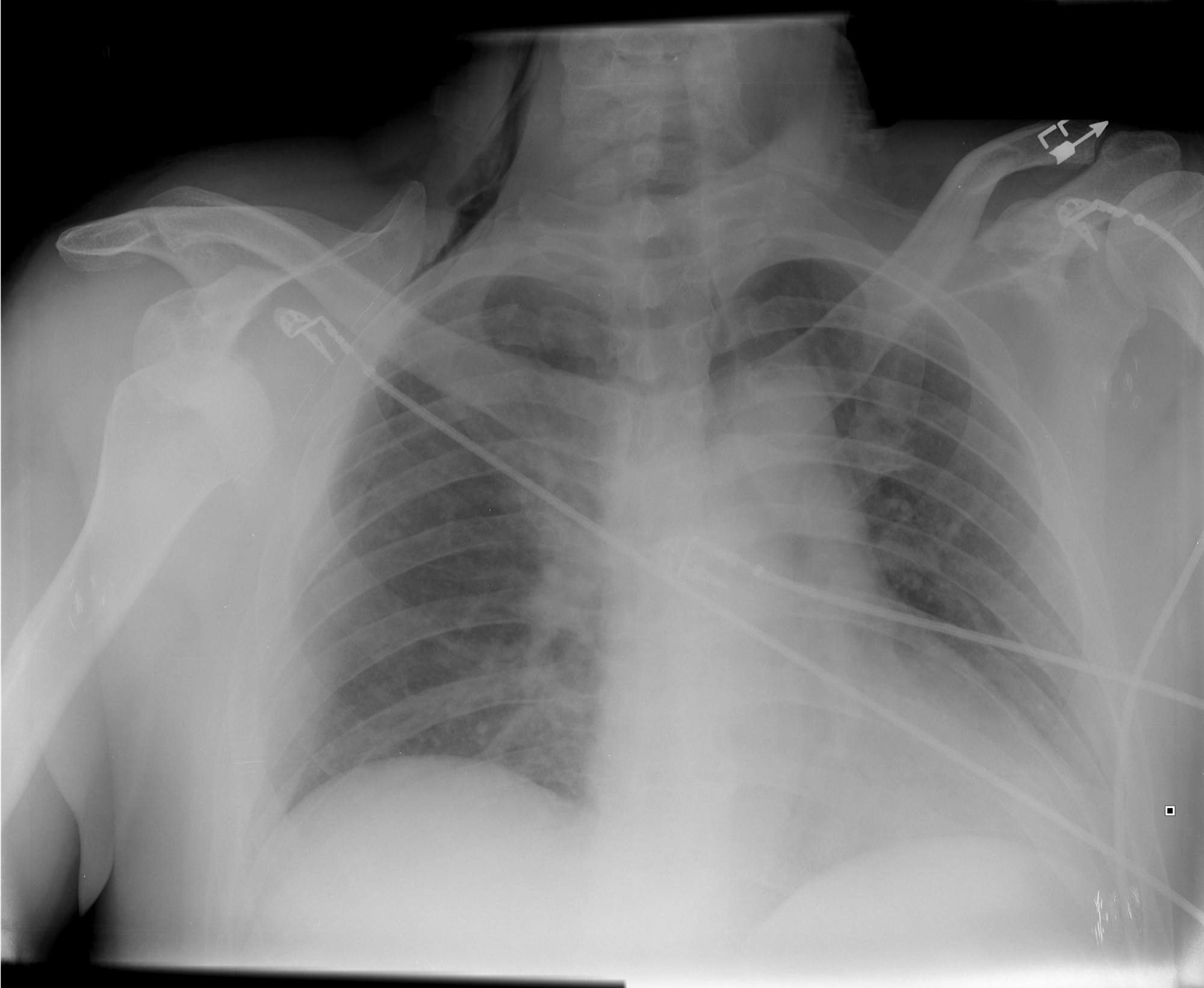
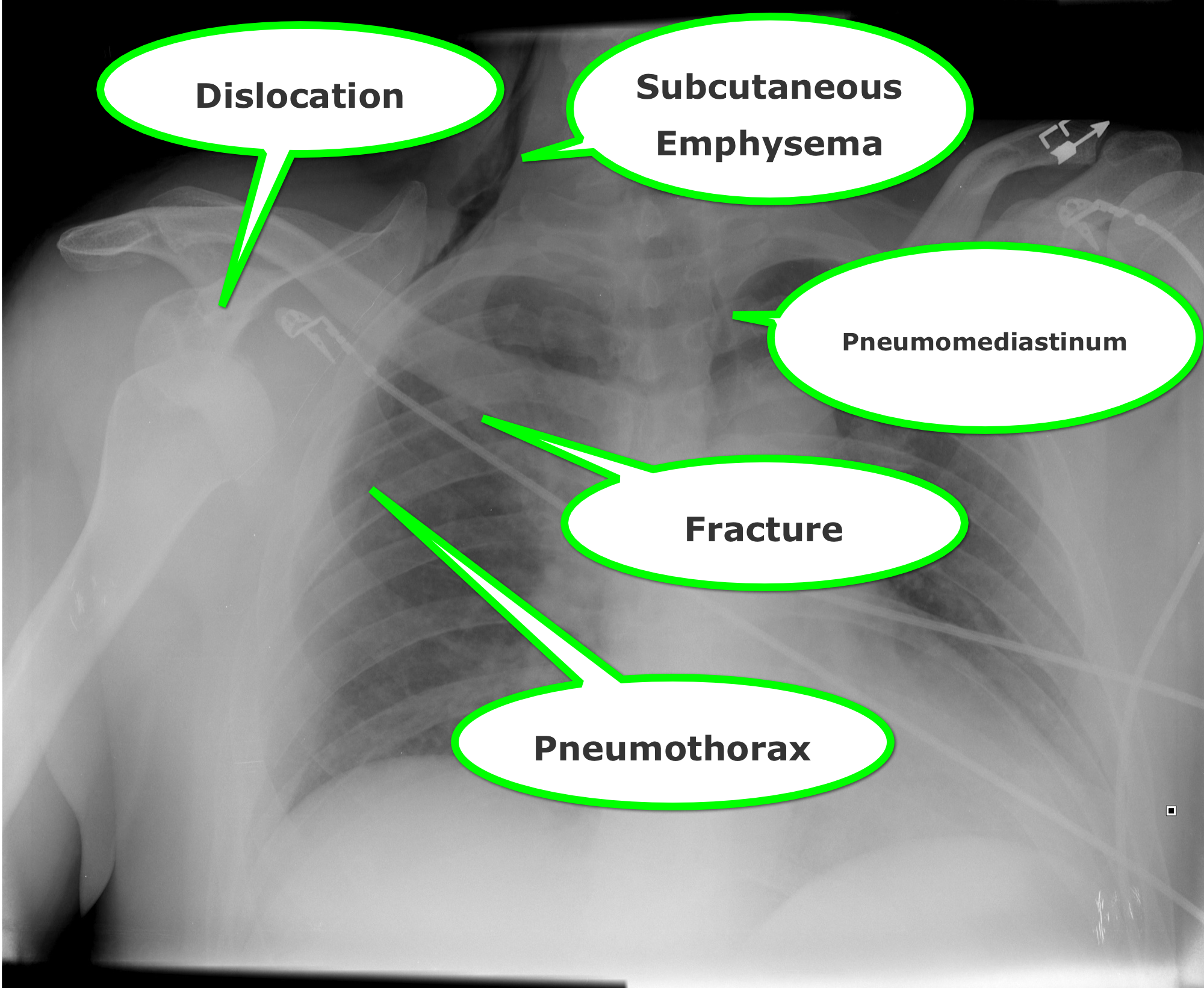
Find four abnormalities in the chest Xray below.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 7/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Wernicke encephalopathy (WE) is a neurologic disorder secondary to prolonged thiamine deficiency; it is characterized by confusion, ataxia, and ocular abnormalities.
Traditional medical teaching advises against the administration of glucose (or glucose containing fluid) in thiamine deficient patients, without first giving thiamine, as this may precipitate WE.
This teaching is problematic, however, in hypoglycemic patients who require the immediate administration of glucose while simultaneously being suspected of thiamine deficiency (e.g., malnourished alcoholics). Delays in treating hypoglycemia may be more harmful (e.g., seizures, permanent neurologic deficits, etc.) than the risk of WE.
Schabelman et. al performed a literature search to unearth the origins of this teaching. Nineteen papers related to this topic were found consisting of case reports, animal studies, and expert opinion; there were no randomized trials, cohort studies, or case-control studies.
Bottom-line: The available evidence does not support withholding glucose treatment until thiamine can be administered and educators should consider abolishing this dogmatic teaching until better evidence is available.
Schabelman, et al. Glucose before thiamine for Wernicke encephalopathy: a literature review. J Emerg Med. 2012 Apr; 42(4): 488-94
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/15/2012 by Haney Mallemat, MD
(Updated: 7/16/2012)
Click here to contact Haney Mallemat, MD
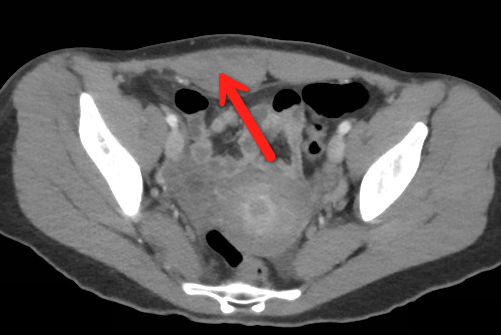
23 year-old female presents complaining of progressive right lower quadrant pain after doing "vigorous" pushups. CT abdomen/pelvis below. What’s the diagnosis? (Hint: it’s not appendicitis)
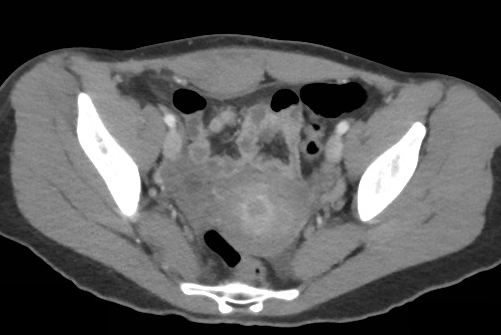
Answer: Rectus Sheath Hematoma
Rectus Sheath Hematoma (RSH)
Rectus muscle tear causing damage to the superior or inferior epigastric arteries with subsequent bleeding into the rectus sheath; uncommon cause of abdominal pain but mimics almost any abdominal condition.
May occur spontaneously, but suspect with these risk factors:
Typically a self-limiting condition, but hypovolemic shock may result from significant hematoma expansion.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/8/2012 by Haney Mallemat, MD
(Updated: 7/9/2012)
Click here to contact Haney Mallemat, MD
A previously healthy 3 year-old male presents with a one-day history of fever, drooling, and refusal to move his neck. The lateral neck x-ray is shown. What's the diagnosis?
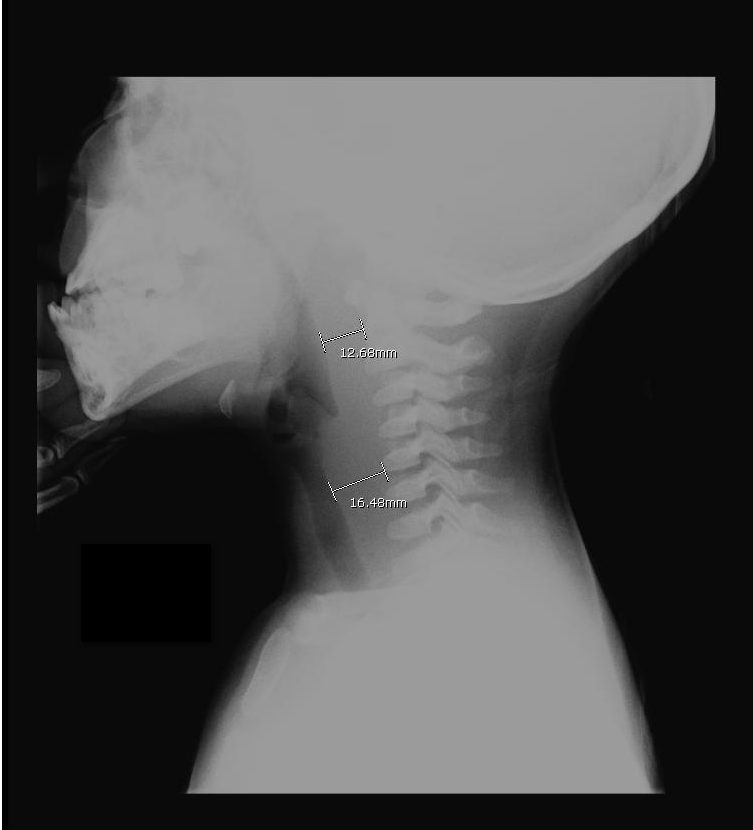
Answer: Retropharyngeal abscess
Retropharyngeal Abscess (RPA)


Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Keywords: hydroxyethyl starch crystalloid, colloid, lactated ringers, normal saline, resuscitation, sepsis, hypotension (PubMed Search)
Posted: 7/3/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Septic patients with hemodynamic instability often require intravenous fluids as part of their resuscitation. Major debate has occurred whether the optimal resuscitation fluids are crystalloids (e.g., normal saline) or colloids (e.g., albumin).
In theory, colloids are more potent intravascular expanders than crystalloids because their oncotic pressure is higher and should increase intravascular volume similarly to larger amounts crystalloid (i.e., colloids require less volume during resuscitation).
Despite these theoretical benefits, the colloid hydroxyethyl starch (HES), has come under scrutiny after prior studies have linked its use with adverse outcomes.
A recent prospective randomized-control trial compared the use of HES to lactated acetate for resuscitating septic patients and found that HES significantly increased both the incidence of renal-replacement therapy and mortality at 90 days (both primary end-points in the study).
Bottom line: There is no convincing data that HES performs superiorly to crystalloid for resuscitation in sepsis and there is increased harm with its use. Furthermore, the increased cost of HES compared to crystalloids does not justify its routine use.
Perner A., et al. Hydroxyethyl Starch 130/0.4 versus Ringer's Acetate in Severe Sepsis. NEJM. 2012 Jun 27.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/2/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Have you ever had to give a national presentation, but can't find that one ultrasound clip or image that you really need? You could "borrow" it from someone on the internet, but you are secretly afraid that the "owner" of the clip is lurking somewhere in the audience. Well, the guys at the Ultrasound Podcast (www.ultrasoundpodcast.com) have come to your rescue by creating SonoCloud, a free access ultrasound library. At Sonocloud, you will find several categories of ultrasound clips and images for you to view and share,...and again it's FREE. In fact, the only thing you are expected to do is upload some of your own ultrasounds to share.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 6/24/2012 by Haney Mallemat, MD
(Updated: 6/25/2012)
Click here to contact Haney Mallemat, MD
77 year old male presents to the Emergency Department one week after a motor vehicle crash in which he suffered minor facial injuries. He is now concerned because his eye looks like this. Diagnosis?
Answer: Subconjunctival Hemorrhage
Subconjunctival hemorrhage is the accumulation of blood between the conjunctiva and sclera (i.e., subconjunctival space) secondary to bleeding from conjunctival or episcleral blood vessels.
Subconjunctival hemorrhage may be caused by:
Treatment should be directed towards reversing the underlying cause and providing symptomatic relief (e.g., artificial tears)
Prognosis is typically good. Occasionally the hemorrhage becomes yellowish-green (similar to a bruise) during the healing phase; this eventually resolves.
Bonus Pearl: As July 1rst approaches a new class of doctors will begin their journey to become Emergency Medicine specialists. The EM Basic website, created by Dr. Steve Carroll, was developed as a boot camp guide for Emergency Medicine. At the EM Basic website, you can find podcasts and discussions of must know topics within Emergency Medicine. Check it out today at http://embasic.org or on iTunes
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 6/19/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Two recently presented abstracts at the 2012 Society of Critical Care Medicine conference suggest that the combination of vancomycin and piperacillin-tazobactam may lead to acute kidney injury (AKI) in the critically ill. There may also be evidence to suggest that piperacillin-tazobactam alone increases the risk of AKI.
Both abstracts retrospectively compared patients who received either vancomycin alone or the combination of vancomycin and piperacillin-tazobactam. In both studies, the rates of AKI were significantly lower in patients treated with vancomycin alone as compared to patients receiving both vancomycin and piperacillin-tazobactam.
Bottom line: Although the current evidence does not support a change in our clinical practice, more prospective studies exploring this topic are necessary.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Min, et al. Acute Kidney Injury in Patients Recieving Concomitant Vancomycin and Piperacillin/Tazobactam. Critical Care Medicine. December 2011. 39(12); p 200
Hellwig, et. al. Retrospective Evaluation of the Incidence of Vancomycin and/or Piperacillin-Tazobactam Induced Acute Renal Failure. Critical Care Medicine. December 2011. 39(12); p 79
Category: Visual Diagnosis
Posted: 6/18/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
79 year old male with headaches, ataxia, falls, and difficulty urinating. What's the diagnosis?
Diagnosis: Ventriculomegaly secondary to Normal Pressure Hydrocephalus
An approach to ventriculomegaly
Ventriculomegaly is due to cerebral atrophy (e.g., Parkinson disease) or increased cerebrospinal fluid (CSF) within the ventricles. Increased CSF is due to:
Congenital causes of ventriculomegaly:
Acquired causes of ventriculomegaly:
Category: Visual Diagnosis
Posted: 6/11/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
19 year-old male presents with L ankle pain and obvious deformity after jumping out of a window and landing on his inverted foot. What's the diagnosis?

Sub-talar dislocation
Wheeless' Textbook of Orthopedics
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 6/4/2012 by Haney Mallemat, MD
(Updated: 6/5/2012)
Click here to contact Haney Mallemat, MD
Consider rhabdomyolyisis secondary to heat exposure as summertime approaches; have a low threshold to screen patients if they are at risk (e.g., people exercising in high-ambient temperatures).
Symptoms include muscle tenderness, cramping, and swelling with associated weakness. Patients with altered mental status (e.g., heat stroke) should be examined for limb induration, skin discoloration (i.e., ischemia), or compartment syndrome.
Complications:
Treatment
Khan, F. Y. Rhabdomyolysis: a review of the literature. The Netherlands journal of medicine, 67(9), 272 – 283.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 5/28/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Ultrasound is useful during intubation; here is a video explaining how: http://ultrarounds.com/ultrarounds.com/Visual_Pearl_May_28,_2012.html
Today's Bonus Pearl:
EMRA has developed a great antibiotic guide for the iphone (http://itunes.apple.com/us/app/2011-emra-antibiotic-guide/id393020737?mt=8) or android (https://play.google.com/store/apps/developer?id=Emergency+Medicine+Residents'+Association). This app is a bit pricey ($15.99), but is easy to use and well organized. Enjoy!
Chou, H. et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. Jun 2011
Werner SL,et al. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med 2007;49:75–80.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 5/21/2012 by Haney Mallemat, MD
(Updated: 5/22/2012)
Click here to contact Haney Mallemat, MD
Carcinoid tumors are neuroendocrine malignancies typically located in the GI tract; most commonly in the terminal ilium and appendix.
Carcinoid tumors produce serotonin, histamine, bradykinin, and/or prostaglandin that result in diarrhea, facial flushing, or bronchospasm. These vasoactive substances may also lead to hypotension and vasodilatory shock.
The tumor may also affect the tricuspid and pulmonary valves leading to right-heart failure secondary to valvular regurgitation, stenosis or both.
Treatment is directed at controlling the malignancy (e.g., octotrotide and tumor resection) as well as managing the right-sided heart failure when it occurs (e.g., inotropes, diuretics, vasopressors, etc.).
Fox, D. J. (2004). Carcinoid heart disease: presentation, diagnosis, and management. Heart, 90(10), 1224–1228
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 5/14/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
This week's visual pearl is an interesting ultrasound of a psoas abscess submitted by Dr. Sa'ad Lahri. He is an Attending physician in the Emergency Department of the Khayelitsha Hospital in Cape Town, South Africa. The video quality is grainy, but it automatically replays so you can watch it a few times.
http://ultrarounds.com/ultrarounds.com/Visual_Pearl_May_14,_2012.html
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 5/8/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Severe acute pancreatitis (SAP) is a life-threatening form of pancreatitis, with up to 30% mortality.
SAP may lead to hypovolemic shock (secondary to vasodilation and capillary leak), hypoxemia (from acute respiratory distress syndrome), and multi-organ failure.
Suspect SAP with signs and symptoms of pancreatitis plus any of the following:
Treatment of SAP should focus on:
Greer, S. E., & Burchard, K. W. (2009). Acute pancreatitis and critical illness: a pancreatic tale of hypoperfusion and inflammation. Chest, 136(5), 1413–1419.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
