Category: Orthopedics
Keywords: Morton, neuroma (PubMed Search)
Posted: 2/18/2012 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Morton's Neuroma
Thomas JL, et al. Diagnosis and treatment of forefoot disorders: Morton's intermetatarsal neuroma. Journal of Foot and Ankle Surgery. 2009;48:251.
Category: Orthopedics
Keywords: Flexor, Tenosynovitis (PubMed Search)
Posted: 1/21/2012 by Michael Bond, MD
Click here to contact Michael Bond, MD
Flexor Tenosynovitis
You can follow this link, http://www.youtube.com/watch?v=qf9SW0ChsCU , to see the physical exam findings of flexor tenosynovitis
Category: Misc
Keywords: Triage, Mass Causality (PubMed Search)
Posted: 12/31/2011 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
START Triage
START triage is a simple system to implement that does not require any special equipment in order to determine who needs immediate, delayed or non-urgent care during a mass causality.
START stands for Simple Triage And Rapid Treatment. Patients are triaged based on 4 factors:
The steps are:
So those that can leave are green, those that do not meet any of the START criteria are YELLOW, and those with any of the four factors are RED or DEAD.
Category: Orthopedics
Keywords: Back Pain, Treatment, Guidlines (PubMed Search)
Posted: 11/19/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Low Back is one of the most common complaints that we see in the Emergency Department. Our first priority is to rule out those causes that can lead to paralysis or death (i.e.: epidural abscess, pathological fracture, cauda equina syndrome, etc…). However, most of the back pain that we will see is musculoskeletal in origin.
The American College of Physicians (ACP) and the American Pain Society (APS) released joint recommendations on the evaluation of treatment of individuals with back pain in 2007.
In summary their key recommendations were:
Links to the Clinical Guidelines are listed below:
Category: Orthopedics
Keywords: Sinus tarsi syndrome (PubMed Search)
Posted: 10/15/2011 by Michael Bond, MD
(Updated: 9/24/2013)
Click here to contact Michael Bond, MD
Sinus Tarsi Syndrome
Category: Orthopedics
Keywords: Posterolateral Corner, knee (PubMed Search)
Posted: 9/17/2011 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Posterolateral Corner Injuries
The posterolateral corner “PLC” of the knee is becoming increasingly recognized as an extremely important structure to maintain the stability of the knee joint.
PLC injuries occur with hyperextension, varus load and tibial external rotation. So the most common mechanism is a posterolaterally directed blow to the anteromedial tibia when the knee is hyperextended. PLC injuries are commonly associated with injury to other ligaments (ACL, PCL, LCL) and occur in isolation in <5% of cases. If suspected make sure to check for other ligamentous injuries.
Since this injury can be missed and is associated with significant disability it is important to test for it. This YouTube video, http://youtu.be/bnXaTdvZZ6o, demonstrates several examination techniques that can identify the injury.
Wheeless Online Ortho Reference http://www.wheelessonline.com/ortho/posterolateral_rotary_instability_of_the_knee
Category: Orthopedics
Keywords: Sugar Tong Splint (PubMed Search)
Posted: 9/3/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Sugar Tong Splint
The sugar tong splint is ideal for splinting fractures of the radius, ulna, or wrist. It prevents flexion and extension at the wrist, limits flexion and extension at the elbow, and prevents supination and pronation. A posterior long arm splint does not prevent supinaton and pronation, therefore, it is of limited use for radius and ulna fractures.
The traditional sugar tong can be difficult to put on a patient without an assistant as it is often hard to hold the splint in position as you begin to ace wrap it. A variation on the sugar tong, the reverse sugar tong, prevents this frustration. The splinting material is cut so that a small piece suspends the splint from the web space between the thumb and index finger. The open ends at the elbow are also easily folded under each other, preventing any bulky splint material from extending out.

The reverse sugar tong is on the left, the original sugar tong on the right.
Check out this video showing how to place a reverse sugar tong splint.
http://www.youtube.com/watch?v=r-RHdttOMf0
Category: Misc
Keywords: Wound, Repair (PubMed Search)
Posted: 7/30/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Wound Repair
A pearl last year addressed the irrigation of wound and the fact that the type of fluid (sterile versus tap water) does not affect infection rates but rather the volume of irrigation is most important.
Sterile versus unsterile gloves have also been studied, and it turns out that clean unsterile gloves have the same rate of infection as sterile gloves but come with a substantial cost savings.
When caring for a contaminated wound it is most important to remove any gross contamination, and then irrigate the wound as much as possible. A 20 mL syringe with an 18G angio-catheter provides the proper pressure to remove debris without causing tissue damage. The wound can then be closed wearing the gloves that are most comfortable or accessible to you.
Finally, from a medicolegal standpoint it is always best to inform the patient that you have tried to remove all of the contamination but there is still a chance that the wound can get infected.
Category: Infectious Disease
Keywords: C. Diff Colitis (PubMed Search)
Posted: 7/16/2011 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
C. Diff Colitis
The general treatment recommendations for C. Diff Colitis are to place the patient on PO metronidazole and if they fail this treatment PO vancomycin (125 mg 4x day). Vancomycin is generally reserved for resistant cases due to the fear that it could induce Vancomycin resistant enterococcus.
For severally ill patients it is recommended that you prescribe IV metronidazole and PO vancomycin when they are not actively vomiting. Remember there is no role for IV vancomycin as it does not get into the bowel lumen to eradicate the infection.
There is some great news though, the FDA recently approved a new drug, a macrolide antibiotic fidaxomicin (Dificid), for the treatment of C. Diff Colitis. Fidaxomicin was found to be as effective as vancomycin in preventing recurrence 3 weeks after treatment. Currently it is recommended that fidaxomicin be reserved for cases where patients are having recurrences after 3 weeks of vancomycin treatment.
The FDA news release can be found at http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm257024.htm
Category: Orthopedics
Keywords: kocher, septic arthri (PubMed Search)
Posted: 6/18/2011 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Kocher Criteria for Septic Arthritis in Children:
Septic arthritis should be suspected in children that have a painful joint especially if they do not want to weight bear. Orthopedics uses the Kocher Criteria to determine the probability of whether the joint is infected.
Four elements make up the criteria:
If only one sign is present there is a 3% chance the child has a septic joint.
Category: Orthopedics
Keywords: Iliopsoas, tendonitis, syndrome (PubMed Search)
Posted: 5/21/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Iliopsoas tendonitis and Iliopsoas Syndrome
Category: Orthopedics
Keywords: Tendon, laceration (PubMed Search)
Posted: 5/7/2011 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Tendon Lacerations:
A reasonable approach to all tendon lacerations is to close the wound and splint in the hand in the position of function until the patient can be seen by a hand surgeon in the next 1-3 days. These injuries do not require immediate surgical repair.
Wheeless Textbook of Orthopaedics. http://www.wheelessonline.com/ortho/extensor_tendon_lacerations
Category: Orthopedics
Keywords: Tendon Laceration (PubMed Search)
Posted: 4/30/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Tendon Lacerations:
Hand lacerations need to be carefully explored in order to determine whether there is an associated tendon laceration. These can be be difficult to find unless a systematic approach is followed:
Future pearls will cover techniques on how to repair tendon lacerations. Stay tuned.
Category: Orthopedics
Keywords: Knee Dislocation, Prosthetic (PubMed Search)
Posted: 4/9/2011 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Knee dislocations are uncommon, and prosthetic knee dislocations even rarer. Some general facts about prosthetic knee dislocations are:
Wang CJ, Wang HE. Dislocation of total knee arthroplasty: a report of 6 cases with 2 patterns of instability. Acta Orthop Scand 1997;68:282-285.
Stiehl JB, Komistek RD, Dennis DA, et al. Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br 1995;77:884-889.
Category: Orthopedics
Posted: 3/12/2011 by Michael Bond, MD
(Updated: 3/19/2011)
Click here to contact Michael Bond, MD
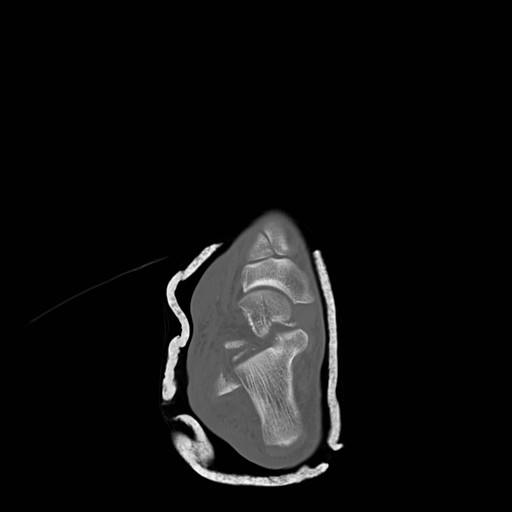
Talar Neck Fractures
Have a high rate of avascular necrosis (AVN), nonunion, and arthritis. Almost all require ORIF


Category: Orthopedics
Keywords: radius, fracture, treatment (PubMed Search)
Posted: 2/19/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Distal Radius Fractures
Typically distal radius fractures are treated with closed reduction and splinting in the ED, followed by operative repair. This is done because it is felt that patients will have the best functional outcomes if the bones are restored to their normal anatomic alignment. However, two studies published in 2010 suggest differently.
The study by Neidenbach showed that after one year there was no difference in functional outcomes between patients that were just splinted in the ED in the position the fracture was found versus those that had closed reduction with splinting.
The second study by Ego showed that there was no difference in outcomes between those that underwent conservative treatment with closed reduction and splinting versus those that underwent operative repair.
The take home point from these studies for the EM physician is that most distal radius fractures can be splinted in the position found with them following up with an orthopaedist. There is probably little advantage to performing a closed reduction in the ED knowing that this procedure can use a lot of valuable time and resources.
Neidenbach P, Audige L, Wilhelmi-Mock M, Hanson B, De Boer P. The efficacy of closed reduction in displaced distal radius fractures. Injury. 2010;41(6):592-598.
Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92(9):1851-1857.
Category: Orthopedics
Keywords: Shoulder, Dislocation, FARES (PubMed Search)
Posted: 1/15/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
FARES Method for Reduction of Anterior Shoulder Dislocations.
This method that was recently highlighted in a publication had a ~78% success rate with the authors able to reduce the shoulder in an average of 2.36 ±1.24 minutes without having to give the patients any analgesics or sedatives. The technique is done by:
Consider trying this with your next shoulder dislocation. No single method of reduciton is 100% successful, but methods like this that only require a single provider and do not require analgesics are extremely helpful in improving patient flow as they do not utilize a lot of ED resources..
Category: Orthopedics
Keywords: peroneal, tendon, subluxation (PubMed Search)
Posted: 1/1/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Peroneal Tendon Subluxation: The Other Ankle Sprain
Roth et al. Peroneal tendon subluxation: the other lateral ankle injury. Br J Sports Med (2010) vol. 44 (14) pp. 1047-53
Category: Orthopedics
Keywords: Septic Arthritis, Diagnosis (PubMed Search)
Posted: 12/18/2010 by Michael Bond, MD
(Updated: 12/19/2010)
Click here to contact Michael Bond, MD
Septic Arthritis
It is generally taught that if the synovial fluid white blood count (WBC) is less than 50,000 it is not septic, however, there is growing evidence that a clear delineation in the WBC between septic arthritis and inflammatory arthritis is not possible. In fact, inflammatory arthritis (rheumatoid and gout) actually increases your risk for septic arthritis and the two can coexist. Gram stains of the fluid only show organisms in 50% of those with septic arthritis so you also can not rely on them either. Inflammatory markers (CRP, ESR) can be elevated with inflammatory or septic arthritis so they too can not differentiate between the two.
In the end, because of the risk of permanent joint dysfunction, it is important to make the diagnosis on clinical grounds and treat empirically if you are unsure. Err on the sound of treatment. Serial joint aspirations to drain synovial fluid have the same outcomes as operative washout.
A recent article that discusses the concerns with making the diagnosis of septic arthritis is:
Mathews et al. Bacterial septic arthritis in adults. Lancet (2010) vol. 375 (9717) pp. 846-55
Mathews et al. Bacterial septic arthritis in adults. Lancet (2010) vol. 375 (9717) pp. 846-55
Category: Orthopedics
Keywords: spondyloysis, spondylosis, spondylolistesis, spondylitis (PubMed Search)
Posted: 12/4/2010 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Dr. Corwell covered Spondyloysis in July 2010 https://umem.org/res_pearls_referenced.php?p=1134 but if you are like me you might have trouble remembering the differences between the following terms:
