Category: Geriatrics
Keywords: bruising, elderly, forensic, abuse (PubMed Search)
Posted: 3/4/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Category: Neurology
Keywords: headache, steroids, bleed (PubMed Search)
Posted: 2/28/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Benign headaches are common in bodybuilders. However, several less benign headaches are worth noting:
All except the first two are exclusively reported in patients on anabolic steroids, growth hormone, and/or “energy” supplements. Make sure to ask your patient about these risk factors.
Busche K. Neurologic Disorders Associated with Weight lifting and Bodybuilding. Neurology Clinics. 26 (2008) 309–324
Category: Geriatrics
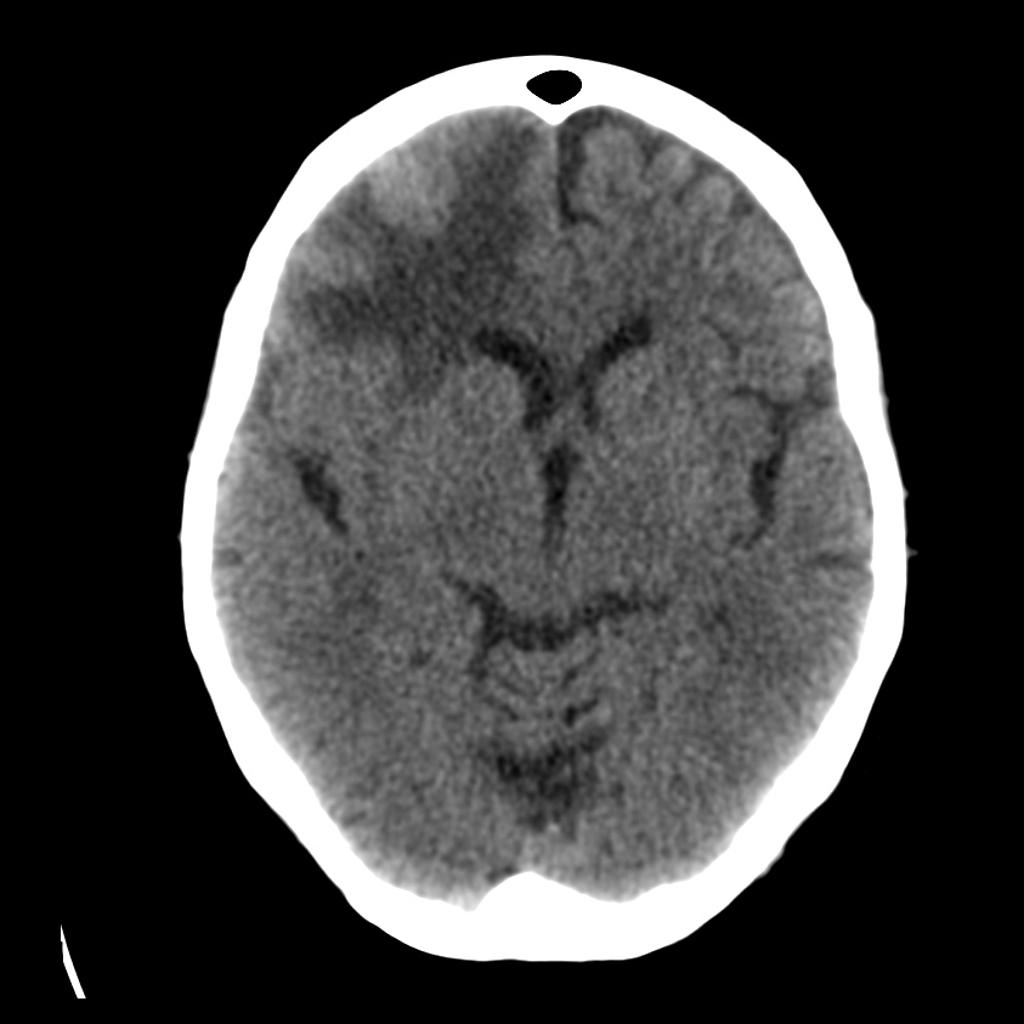
Keywords: dizziness, CT, MRI, Cerebellar (PubMed Search)
Posted: 2/5/2018 by Danya Khoujah, MBBS
(Updated: 2/8/2026)
Click here to contact Danya Khoujah, MBBS
15% of older adults presenting to ED for dizziness have serious etiologies; 4-6% are stroke-related and sensitivity of CT for identifying stroke or intracranial lesion in dizziness is poor (16%), so if CNS etiology suspected, seek neuro consult or MRI (83% sensitivity)
Lo AX, Harada CN. Geriatric dizziness: evolving diagnostic and therapeutic approaches for the emergency department. Clin Geriatr Med. 2013;29(1):181-204.
Category: Neurology
Keywords: edema, hemorrhage, tumor, CT, MRI, contrast (PubMed Search)
Posted: 1/24/2018 by Danya Khoujah, MBBS
(Updated: 2/8/2026)
Click here to contact Danya Khoujah, MBBS
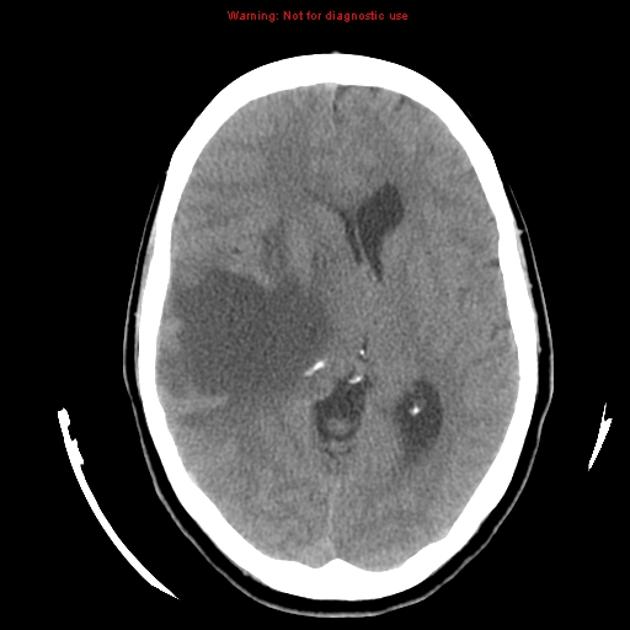

Klein JP, Dietrich J. Neuroradiologic Pearls for Neuro-oncology. Continuum 2017;23(6):1619-1634.
Category: Geriatrics
Keywords: Delirium, dementia, screening, altered (PubMed Search)
Posted: 1/7/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
A recent study was undertaken to validate the 4A's Test for the assessment of delirium in the elderly, with particular focus on inpatient geriatric patients; it revealed that the tool had high sensitivity in detecting delirium, particularly in those with dementia or language barriers, in whom this diagnosis can often be difficult to make. Further studies would be useful in a similar demographic of emergency department geriatric patients to confirm that this straightforward test is generalizable to the emergency department geriatric patient population.
The 4A’s Test used for this study was accessed from www.the4AT.com (Free Access).
The 4AT consists of four items with a maximum achievable score of 12.
Item 1 determines patient’s level of alertness by operator observation (maximum score 4).
Items 2 and 3 screen cognition and attention with the use of the Abbreviated Mental Test-4 (AMT-4) (maximum score 2) and Months Backwards (maximum score 2).
Item 4 assesses for ?uctuation and acute changes in mental state (score 0 or 4).
A score of 0 indicates delirium or cognitive impairment is unlikely.
A score between 1 and 3 indicates possible cognitive impairment (corresponding to stand alone dementia screening tools).
A score of 4 and above is suggestive of delirium.
Category: Neurology
Keywords: headache, seizure, stroke, neurological deficit, thrombogenic (PubMed Search)
Posted: 12/27/2017 by Danya Khoujah, MBBS
(Updated: 2/8/2026)
Click here to contact Danya Khoujah, MBBS
Long B, Koyfman A, Runyon MS. Cerebral Venous Thrombosis: A Challenging Neurologic Diagnosis. Emerg Med Clin N Am 35 (2017) 869–878
Category: Geriatrics
Keywords: UTI, infection, elderly, symptoms, antibiotics (PubMed Search)
Posted: 12/3/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Asymptomatic bacteriuria is common and increases with age, with an incidence of up to 50% in women over the age of 70. Asymptomatic bacteriuria does not carry an associated high morbidity or mortality if left untreated; it is usually transient and resolves spontaneously. In order to decrease polypharmacy and possible drug interactions in our elderly patients, they should only be diagnosed with and treated for a UTI if they have laboratory evidence of a UTI (bacteriuria and pyuria) and have two of the following:
· Fever
· Worsened urinary urgency or frequency
· Acute dysuria
· Suprapubic tenderness
· Costovertebral angle tenderness
Mody L, Juthani-Mehta M. Urinary Tract Infections in Older Women: A Clinical Review. JAMA. 2014;311(8):844-854. doi:10.1001/jama.2014.303.
Category: Neurology
Keywords: GBS, weakness, intubation, CSF, LP (PubMed Search)
Posted: 11/22/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Allen JA. Chronic Demyelinating Polyneuropathies. Continuum 2017;23(5):1310–1331
Category: Geriatrics
Keywords: elderly, psychiatry, mental health, screening (PubMed Search)
Posted: 11/5/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Arias, S. A., Boudreaux, E. D., Segal, D. L., Miller, I., Camargo, C. A. and Betz, M. E. (2017), Disparities in Treatment of Older Adults with Suicide Risk in the Emergency Department. J Am Geriatr Soc, 65: 2272–2277. doi:10.1111/jgs.15011
Category: Neurology
Keywords: weakness, infection, paralysis, intubation, influenza, vaccine (PubMed Search)
Posted: 10/25/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
It's respiratory infection and flu vaccine season! Time to brush up on Guillain-Barré Syndrome..
- It is the most common cause of acute or subacute flaccid weakness worldwide
- 70% of cases are preceded by an infection in the past 10-14 days, but most are minimized or forgotten by the patient. 40% of these infections are by Campylobacter jejuni.
- 30% develop respiratory failure requiring intubation and ventilation
- Half of the patients will develop their maximum weakness by 2 weeks, most will develop it by 4 weeks.
Donofrio PD. Guillain-Barré Syndrome. Continuum 2017;23(5):1295–1309.
Category: Geriatrics
Posted: 10/1/2017 by Danya Khoujah, MBBS
(Updated: 2/8/2026)
Click here to contact Danya Khoujah, MBBS
Providing consistent, quality emergency care to the elderly is critically important. The Geriatric Emergency Department (GED) guidelines, developed collaboratively, provide a standardized set of guidelines to help improve care of the geriatric population in the emergency department.
In order to improve the standards for geriatric emergency care, representatives from the American College of Emergency Physicians, the American Geriatrics Society, Emergency Nurses Association, and the Society for Academic Emergency Medicine worked together to create the GED Guidelines. These guidelines create a template related to developing a geriatric focused emergency department, including specific recommendations related to staffing and administration, follow up and transition of care, education, quality improvement, equipment and supplies, as well as policies and procedures.
https://www.acep.org/
https://www.acep.org/WorkArea/
Category: Neurology
Keywords: stroke, tPA, thrombolytics, ICH, hemorrhage, adverse events (PubMed Search)
Posted: 9/28/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Category: Geriatrics
Keywords: arrhythmia, syncope, fall (PubMed Search)
Posted: 9/4/2017 by Danya Khoujah, MBBS
(Updated: 2/8/2026)
Click here to contact Danya Khoujah, MBBS
20% of unexplained falls in the elderly can be attributed to an arrhythmia.
Bhangu J, McMahon CG, Hall P, et al. Long-term cardiac monitoring in older adults with unexplained falls and syncope. Heart 2016;102:681-686.
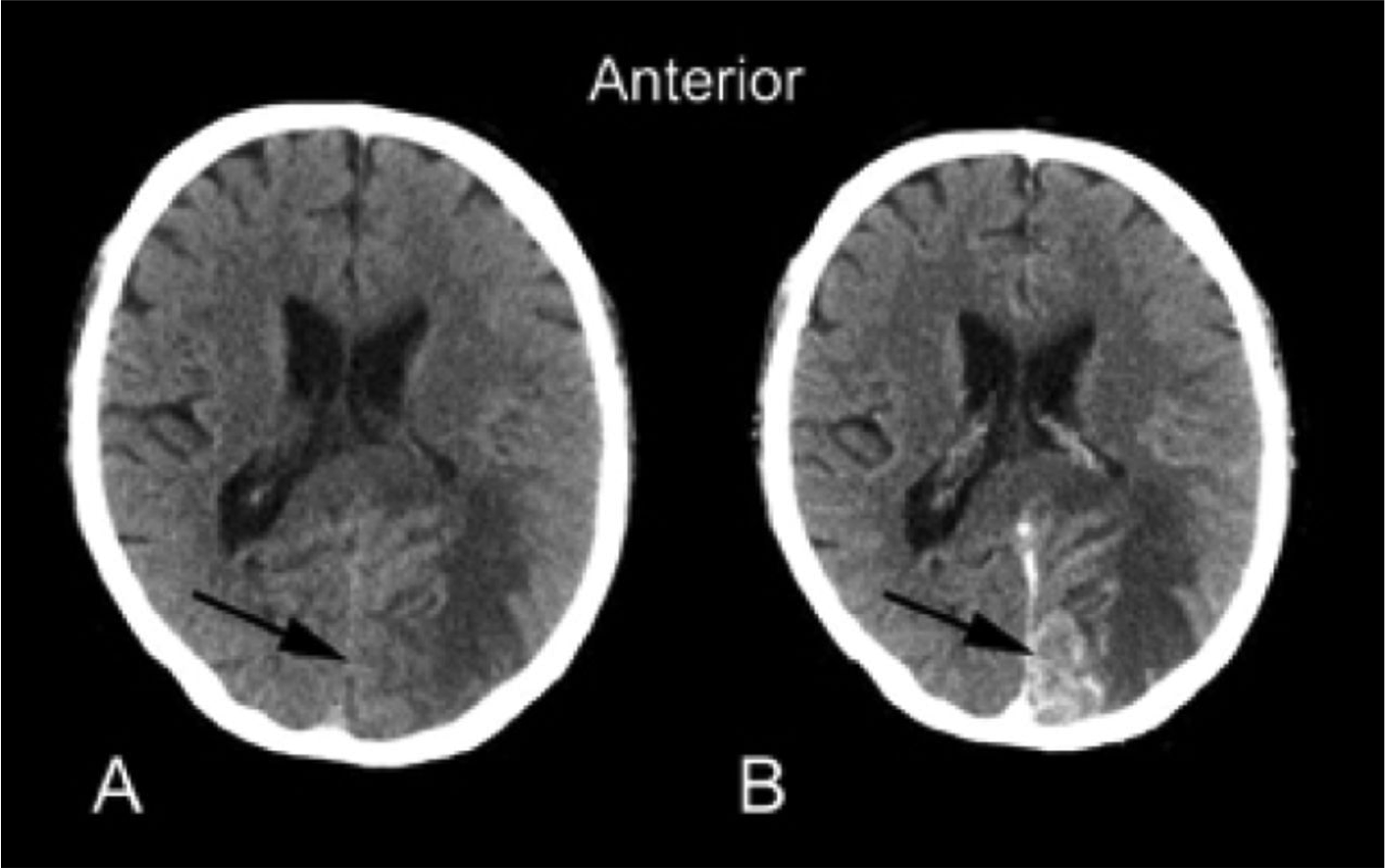
Category: Neurology
Keywords: pituitary apoplexy, subarachnoid hemorrhage, meningitis, headache, CT, MRI (PubMed Search)
Posted: 8/9/2017 by Danya Khoujah, MBBS
(Updated: 2/8/2026)
Click here to contact Danya Khoujah, MBBS
Bottomline: Keep pituitary apoplexy in your differential when considering SAH or meningitis, especially in the presence of risk factors, and have a low threshold to order an MRI.
Category: Geriatrics
Keywords: abuse, marks, interview (PubMed Search)
Posted: 7/3/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
When you are working up an elderly patient for trauma look for patterns such as circumferential bruising on the wrists that have the pattern of fingers the same way you would look at the injuries of a child. Remember that the person who is sitting next to them is frequently the person that is abusing them. Therefore, it is important to interview the patient alone.
Lachs MS, Pillemer KA. Elder Abuse. N Engl J Med 2015; 373:1947-1956
Category: Neurology
Keywords: autoimmune, cancer, encephalopathy (PubMed Search)
Posted: 6/28/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Category: Geriatrics
Keywords: Geriatric, cardiology, symptoms, atypical, angina (PubMed Search)
Posted: 6/4/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Older patients with acute coronoary syndrome (ACS) are less likely to present with typical ischemic chest pain (pressure-like quality, substernal location, radiating to jaw, neck, left arm/shoulder and exertional component) compared with younger counterparts.
Typical angina symptoms predictive of acute myocardial infarction (AMI) in younger patients were less helpful in predicting AMI in the elderly population.
Autonomic symptoms such as dyspnea, diaphoresis, nausea and vomiting, pre-syncope or syncope are more common accompaniments to chest discomfort in elderly ACS patients.
Symptoms may also be less likely to be induced by physical exertion; instead, they are often precipitated by hemodynamic stressors such as infection or dehydration
Bottom Line: Keep a high index of suspicion for ACS in older patients as they present atypically.
Category: Neurology
Keywords: syncope, vasovagal, orthostatic, blood pressure (PubMed Search)
Posted: 5/24/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Vasovagal syncope is a subtype of neurally mediated syncope, and it is distinctly different from orthostatic hypotension.
Patients with orthostatic syncope have severe orthostatic hypotension that results in transient loss of consciousness immediately or within moments of standing up. This is different from neurally mediated syncope, which develops gradually under conditions of prolonged orthostatic stress such as standing for several minutes. Tilt table testing is useful for true orthostatic syncope, but not for neurally mediated syncope. In addition, checking for “orthostatic hypotension” may not capture patient with orthostatic syncope, because the hypotension occurs so quickly after standing up. Of note, patients may still have orthostatic tachycardia or intolerance with neurally mediated syncope.
Category: Neurology
Keywords: syncope, vasovagal, seizures, orthostatic, blood pressure (PubMed Search)
Posted: 5/10/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Cheshire WP. Syncope. Continuum 2017;23(2):335–358.
Category: Geriatrics
Keywords: geriatric, trauma, imaging (PubMed Search)
Posted: 4/3/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
· In the elderly, falling is the most common mechanism of injury
· Unavoidable Risk factors: age 85 or older, male, Caucasian, history of falls
· Other factors: alcohol consumption, polypharmacy
· Mechanisms of fall: slipping, tripping, stumbling
· Physical exam to include: gait, balance, proprioception, vision, strength and cognitive function testing
· Must consider neglect/abuse, affects 10% of seniors per year
· Evaluate for anticoagulant use due to increased risk of intracranial injury
· Use advanced imaging to identify occult hip fractures when clinically suspected and plain radiographs are negative
Abraham, MK, Cimino-Fiallos, NE. Falls in the Elderly: Causes, Injuries, and Management. Medscape February 1, 2017.
http://reference.medscape.com/features/slideshow/falls-in-the-elderly
