Category: Pediatrics
Keywords: avulsion fracture, orthopedics, pelvic injury, trauma (PubMed Search)
Posted: 2/14/2020 by Mimi Lu, MD
(Updated: 2/15/2020)
Click here to contact Mimi Lu, MD
A 15 y.o. female presents to your emergency department with sudden onset hip pain after winding up to kick a soccer ball during her game today. You see a well-developed female in obvious discomfort, with tenderness to palpation over her lateral hip and pain with passive ROM at the hip. You obtain this x-ray. What is your diagnosis?
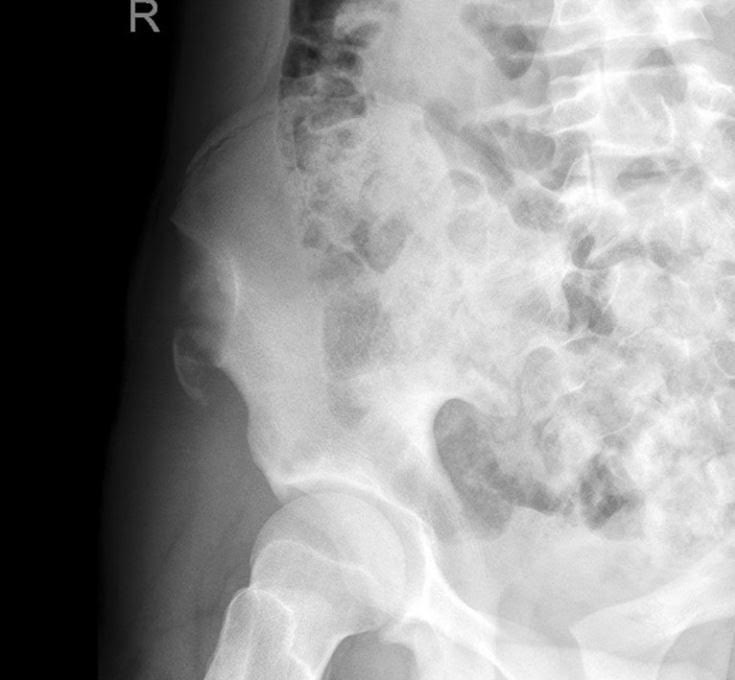
Answer: Avulsion fracture of the anterior superior iliac spine.
Injury:
An avulsion fracture of the anterior superior iliac spine is an uncommon injury seen almost exclusively in adolescent athletes.
They mostly result from a sudden, forceful, and/or unbalanced contraction of the attached musculotendinous unit (sartorius muscle or tensor fascia lata) during the starting phase of running, jumping, kicking, etc.
The most implicated sports include soccer, running, and ice hockey.
History/Exam:
The patient may report sudden shooting pain referred to the involved tuberosity.
Physical exam may include localized edema and tenderness to palpation and pain on passive ROM at the hip.
Anatomy:
The iliac crest is the weakest component of the pelvic ring during adolescence.
The avulsed fragment is usually displaced distally and laterally.
Treatment:
Conservative therapy includes 2-3 weeks of limited activity and walking with partial weight bearing restrictions and crutches. May also include bed rest with the affected lower extremity positioned with the hip and knee in flexion to ensure minimal tension of the muscles attaching to the ASIS. This is considered for minimally displaced fractures in younger children.
Surgical management generally consists of ORIF with a lag screw, and is generally recommended for patients with fracture fragments > 3cm or severely displaced fragments that cause compression of the lateral cutaneous nerve resulting in meralgia parasthetica.
Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30(3):127-31.
Kautzner J, Trc T, Havlas V. Comparison of conservative against surgical treatment of anterior-superior iliac spine avulsion fractures in children and adolescents. Int Orthop. 2014;38(7):1495-8.
Category: Pediatrics
Keywords: lactated ringer, LR, normal saline, NS (PubMed Search)
Posted: 10/25/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Bottom line: Balance fluid resuscitation with LR was not associated with improved outcomes compared to NS and pediatric sepsis. Selective LR use necessitates a prospective trial to definitively determine comparative effects among crystalloids.
1. Weiss SL, Keele L, Balanmuth F, Vendetti N, Ross R, Fitzgerald JC, Gerber JS. Crystalloid Fluid Choice and Clinical Outcomes in Pediatric Sepsis: A Matched Retrospective Cohort Study. J Pdatr.207 Mar:182:304-310.
2. Balamuth F, Kittick M, McBride P, Woodford AL, Vestal N, Casper TC, Metheney M, Smith K, Atkin NJ, Baren JM, Dean JM, Kuppermann N, Weiss SL. Pragmatic Pediatric Trial of Balanced versus Normal Saline Fluid in Sepsis: The PRoMPT BOLUS Randomized Controlled Trial Pilot Feasibility Study. Acad Emerg Med. 2019 Jun 10
Category: Pediatrics
Keywords: UTIcalc, SBI, serious bacterial infection, febrile infant, urinary tract infection (PubMed Search)
Posted: 9/13/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Question: In febrile children younger than 2 years, what combination of clinical and laboratory variables best predicts the probability of a urinary tract infection?
Given that urinary tract infections (UTI) are the most common source of serious or invasive bacterial infections in young febrile infants, early identification and treatment has the potential to reduce poor outcomes. Wouldn't it be great if there was an easy way to identify patients at highest risk?
Researchers from the Children’s Hospital of Pittsburgh formulated a calculator (UTICalc) that first estimates the probability of urinary tract infection (UTI) based on clinical variables and then updates that probability based on laboratory results.
Bottom line:
The UTICalc calculator can be used to guide to tailor testing and treatment in children with suspected urinary tract infection with the hope of improving outcomes for children with UTI by reducing the number of treatment delays.
Go ahead and give it a click!! https://uticalc.pitt.edu/
Shaikh N, Hoberman A, Hum SW, Alberty A, Muniz G, Kurs-Lasky M, Landsittel D, Shope T. Development and Validation of a Calculator for Estimating the Probability of Urinary Tract Infection in Young Febrile Children. JAMA Pediatr. 2018 Jun 1;172(6):550-556.
Category: Pediatrics
Keywords: NV exam, neurovascular, upper extremity injury, orthopedics, hand, fracture, supracondylar (PubMed Search)
Posted: 5/24/2019 by Mimi Lu, MD
(Updated: 8/23/2019)
Click here to contact Mimi Lu, MD
Category: Pediatrics
Posted: 5/24/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Presentation:
- Prepubertal females are especially susceptible to urethral prolapse
- Can present incidentally is a painless mass found during bathing or on exam
- More commonly presents as urogenital bleeding, dysuria, or (rarely) urinary retention
Evaluation:
- Appears as a partial or circumferential "donut" of bright red, often friable prolapsed mucosa
- Typically occurs in the setting of UTI, cough, or constipation
- Need to rule out complications: UTI, urethral necrosis, and urinary retention
Treatment:
- Medical management start with sitz baths twice daily and addressing causative factors (treatment constipation, UTI, etc.)
- Can add either topical corticosteroid (hydrocortisone) or estrogen (Estrace or Premarin 0.01% twice daily)
- Urology follow-up necessary as many will require surgical resection of prolapsed mucosa
Category: Pediatrics
Keywords: closed head injury, concussion, CHI (PubMed Search)
Posted: 4/12/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Over 630,000 children visit the ED every year with a diagnosis of concussion
Predictors of persistent post-concussive symptoms (PPCS):
Appromixately 1/3 of pediatric patients will have PPCS lasting over 2 weeks
Likelihood of PPCS increases to >50% in those with risk factors identified in the ED
Every state has a youth concussion law. The basic tenants are a) immediate removal from play b) written clearance from health professional to return to play c) education for athlete, parents, coaches.
Category: Pediatrics
Keywords: CCHD, congenital cardiac lesions, congenital heart disease (PubMed Search)
Posted: 2/23/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
The hyperoxia-hyperventilation test (aka 100% Oxygen Challenge test) is used to differentiate the cause of central cyanosis in the sick neonate. The majority of neonatal cyanosis is caused by either cardiac or respiratory pathology.
Classically the test is performed as follows:
1. An ABG is obtained with the neonate breathing room air
2. The patient is placed on 100% FiO2 for 10 minutes
3. A repeat ABG is performed looking for an increase in PaO2 to >150 mmHg
- If the hypoxia is secondary to a respiratory cause, the PaO2 should increase to >150 mmHg.
- If the hypoxia is secondary to a congenital cardiac lesion (i.e. secondary to a right-to-left cardiac shunt) the PaO2 is not expected to rise significantly.
In practice, many physicians instead use pulse oximetry and monitor the SpO2 pre and post administration of 10 minutes of 100% FiO2.
- If after 10min of 100% FiO2, if SpO2 is not ? 95% (some resources use 85%) then the central cyanosis is likely secondary to intracardiac shunt.
- When this occurs, presume the sick neonate is symptomatic from a congenital cardiac lesion and initiate prostaglandin E-1 (PGE1) at 0.05-0.01 mcg/kg/min. Use caution as PGE1 may cause apnea.
Category: Pediatrics
Keywords: ADEM (PubMed Search)
Posted: 1/11/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Acute Disseminated Encephalomyelitis (ADEM) is primarily a pediatric disease and can cause a wide variety of neurologic symptoms. As such, should always be in the differential for pediatric patient presenting with vague neurologic symptoms including altered mental status. It is an immune-mediated, demyelinating disease that can affect any part of the CNS; usually preceding a viral illness or rarely, immunizations.
The average age of onset is 5-8 years of age with no gender predilection. It usually has a prodromal. That includes headache, fever, malaise, back pain etc. Neurological symptoms can vary and may present with ataxia, altered mental status, seizures, focal symptoms, behavioral changes or coma.
MRI is the primary modality to diagnose this condition. Other possible indicators may be mild pleocytosis with lymphocyte predominance, and elevated inflammatory markers such as ESR, CRP. These findings, however, are neither sensitive nor specific.
First-line treatment for ADEM is systemic corticosteroids, typically 20-30 mg/kg of methylprednisolone for 2-5 days, followed by oral prednisone 1-2 mg/kg for 1-2 weeks then 3-6-week taper. For steroid refractory cases, IVIG and plasmapheresis may be considered.
ADEM usually has a favorable long-term prognosis in the majority of patients. However, some may experience residual neurological deficits including ataxia, blindness, clumsiness, etc.
Take home points:
Gray, M.P. & Goralick, M.H. (2016). Acute disseminated encephalomyelitis (6th ed, volume 32). Milkwaukee, WI
Category: Pediatrics
Keywords: PECARN, traumatic brain injury, head injury, concussion (PubMed Search)
Posted: 10/12/2018 by Mimi Lu, MD
(Updated: 11/9/2018)
Click here to contact Mimi Lu, MD
Category: Pediatrics
Keywords: West syndrome, seizures (PubMed Search)
Posted: 9/21/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Originally described a Dr. West in 1841 – it is a rare (~1200 cases annually) seizure disorder in young kids, generally less than 1 year old. Very subtle appearance, often with only bending forward or ‘jerking’ of the extremities as opposed to Brief Resolved Unexplained Event (BRUE) or tonic-clonic in description. The spasms can be thought of as a syndrome, where 70% of those have an undiagnosed rare metabolic/genetic disease.
A prompt evaluation, including labs, EEG, MRI, metabolic and genetic studies is vital in helping to establish a diagnosis which can have a profound impact on the patients prognosis. Examples might include Tuberous Sclerosis, Pyridoxine Dependent Seizures among over 50 others.
Bottom line: In pediatric patients less than 1 year old who present to the Emergency Department with a description of spasm-like episodes, consider Infantile Spasms on the differential, and consult your friendly neighborhood Pediatric Neurologist for help in determining a proper disposition.
http://www.childneurologyfoundation.org/disorders/infantile-spasms/
https://www.ninds.nih.gov/Disorders/All-Disorders/Infantile-Spasms-Information-Page
Category: Pediatrics
Keywords: Concussion, minor head injury, traumatic brain injury, mTBI (PubMed Search)
Posted: 9/14/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
The Centers for Disease Control and Prevention recently released guidelines on the diagnosis and management of mild traumatic brain injury (mTBI**) among children. From 2005-2009, children made almost 3 million ED visits for mTBI. Based on a systemic review of the literature, the guideline includes 19 sets of recommendations on the diagnosis, prognosis, and management/treatment of pediatric mTBI.
Key Recommendations:
1. Do not routinely image patients to diagnose mTBI (utilize clinical decision rules to identify children at low risk and high risk for intracranial injury (ICI), e.g. PECARN)
2. Use validated, age-appropriate symptoms scales to diagnose mTBI
3. Assess evidence-based risk factors for prolonged recovery. No single factor is strongly predictive of outcome.
4. Provide patients with instructions on return to activity customized with their symptoms (see CDC Resources below)
5. Counsel patients to return gradually to non-sports activities after no more than 2-3 days of rest.
A wealth for information and tools for provder and families can be found at:
www.cdc.gov/HEADSUP (including evaluation forms and care plans for providers)
www.cdc.gov/traumaticbraininjury/PediatricmTBIGuideline.html
**Although concussion, minor head injury, and mBI are frequently used interchangeably, they have different connotations which allows for misinterpretation and confusion. The guideline recommends the clinical use of the single term mild traumatic brain injury. This is defined as "an acute brain injury resulting from mechanical injury to the head from external physical forces including: (1) 1 or more of the following: Confusion or disorientation, loss of consciousness for 30 minutes or less, posttraumatic amnesia for less than 24 hours, and/or other transient neurologic abnormality such as focal signs, symptoms, or seizure; (2) Glasgow Coma Scale score of 13-15 after 30 minutes post injury or later upon presentation for healthcare
Diagnosis and management of mild traumatic brain injury in children: A systemic review. Lumba-Brown A, Yeates KO, Sarmiento K, Breiding MJ, Haegerich TM, Gioia GA, Turner M, Benzel EC, Suskuer SJ, Giza CC, Joseph M,Broomand C, Weissa B, Gordon W Wright DW, Moser RS, McAvoy K, Ewing-Cobbs L, Duaime AC, Putukian M, Holhouse B, Paulk D, Wade SL, Herig SA, HalsteadM, Keenan H, Choe M, Christia CW, Gusiewic K, Raksin PB, Gregory A, Mucha A, Taylor HG, Callahan JM, DeWtt J, Collins MW, Kirkwood MW, Ragheb J, Ellenbogen RG, Spinks TJ, Ganiats TG, Sabelhaus LJ, Altenhofen K, Hoffman , Getchius T, Gronseh G,Donnell Z, O'Connor RE, Timmons SD JAMA Pediatr 2018 Sept 4.
Category: Pediatrics
Keywords: DKA, cerebral edema, PECARN (PubMed Search)
Posted: 6/22/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Children with diabetic ketoacidosis (DKA) may have brain injuries ranging from mild to severe. The debate over the contribution from intravenous fluids towards poor neurologic outcomes has been ongoing for decades.
PECARN's large multicenter randomized, controlled trial examined the effects of the rate of administration and the sodium chloride content of intravenous fluids on neurologic outcomes in children with diabetic ketoacidosis may finally put the controversy to rest. There was no difference on significant neurologic outcomes based on the rate (fast vs slow) or concentration (0.9% vs 0.45%) of IV fluid administration.
Clinically apparent brain injury occurred in 12 of 1389 episodes (0.9%) of children in DKA.
Any change in the mental or neurological status of the patient should be concerning for life threatening edema and should be treated with mannitol 1g/kg IV bolus or hypertonic saline (3%) 5-10 mL/kg IV over 30 minutes.
Long, B; Koyfman, A. Emergency medicine myths: cerebral edema in pediatric diabetic ketoacidosis and intravenous fluids. J. Emerg. Med; 2017:53(2),212-221.
Category: Pediatrics
Keywords: augmentin, conjunctivitis, AOM, otitis media (PubMed Search)
Posted: 6/8/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Although conjuncitivitis outside of the neonatal period is commonly caused by viruses, there are times when antibiotics are warranted due to bacterial infections, such as conjuncitivits-otitis syndrome.
Bottom line: Every patient with conjunctivitis should have an examination of his/her TMs, as your management may change.
Teoh DL, Reynolds S. Diagnosis and management of pediatric conjunctivitis. Pediatric Emergency Care: 2003; 19(1), pp. 48-55.
Bodor FF, Marchant CD, Shurin PA, Barenkamp SJ. Bacterial etiology of conjunctivitis-otitis media syndrome. Pediatrics: 1985; 76(1), pp.26-28.
Bodor FF. Conjunctivitis-Otitis Syndrome. Pediatrics: 1982; 69(6), 695-698.
Category: Pediatrics
Keywords: Kawasaki's disease, SJS, TEN, dermatitis (PubMed Search)
Posted: 2/9/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Case: 5 year old presents to the ED with 2 weeks of fever. She has extensive cracked, bleeding lips and a rash on her hands and feet. She was recently diagnosed with “walking pneumonia” and hand, foot and mouth disease this week. Her pediatrician sent her in for further workup after she was found to have an elevated CRP on outpatient labs. A similar picture appears in the link below:
What's the diagnosis?
The diagnosis of Mycoplasma pneumonia-induced rash and mucositis (MIRM) was recently termed in the 2015 Journal of American Academy of Dermatology. It is characterized by mucocutaneous eruptions with prominent mucosal involvement. 94% of patients in the reviewed cases had extensive oral lesions that can range from erosions, ulcers or vesiculobullous lesions. 82% of patients had ocular involvement characterized by purulent bilateral conjunctivitis. In 63% of cases, patients were found to have urogenital lesions. Almost all of these patients had prodromal symptoms of cough and fever preceding the eruption by 1 week. The disease was found to be most prominent with young (11.9 ± 8.8 years) and with a 66% male predominance. The treatment is antibiotics such as azithromycin and oral corticosteroids with a minority of patients requiring IVIG. These patients have a good prognosis.
Bottom Line: Consider MIRM in patients with extensive mucosal disease that do not completely fit the criteria of Kawasaki’s or Stevens-Johnson Syndrome/ Toxic Epidermal Necrolysis.
Reference:
Canavan TN, Mathes EF, Frieden I, Shinkai K. Mycoplasma pneumoniae-induced rash and mucositis as a syndrome distinct from Stevens-Johnson syndrome and erythema multiforme: a systematic review. J Am Acad Dermatol. 2015
Feb;72(2):239-45.
Category: Pediatrics
Posted: 1/12/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Pediatrics
Keywords: URI, AOM, wait-and-see, antibiotic stewardship (PubMed Search)
Posted: 11/24/2017 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
As we are approaching the winter in the northern hemisphere, the number of visits for ear pain or respiratory symptoms are expected to increase. The occurrence of acute otitis media (AOM) will also increase, but are these two disease processes related?
Drs. Heikkinen and Chonmaitree published a systematic review of previously reported studies regarding the correlation of these two disease processes (1). As far back as 1990, studies have shown that up to 94% of pediatric patients diagnosed with AOM have concomitant upper respiratory infection (URI) type symptoms at time of diagnosis (2). The viral infections most commonly associated with AOM are respiratory syncytial virus, influenza virus, and adenovirus (3).
The most commonly taught risk factors for developing AOM include young age, male gender, multiple siblings, day care attendance, and passive smoking. These factors are also related to the development of upper respiratory symptoms, and the development of AOM should be thought of as a complication of the upper respiratory infection (4).
Koivunen et al noted the highest incidence of AOM at day 3 after the onset of an URI, and the median time to diagnosis was day 4 (5). If you see a patient in day 2-4 of an URI, who has started to develop an ear effusion, but not clinical AOM, you may want to consider a “Wait-to-see” treatment option if the patient meets treatment criteria (https://em.umaryland.edu/
(1) Heikkinen T, Chonmaitree T. Importance of Respiratory Viruses in Acute Otitis Media. Clinical Microbiology Reviews. 2003;16(2):230-241.
Category: Pediatrics
Keywords: ARDS, oxygenation index, OI, PALICC, acute lung injury, respiratory distress, PARDS (PubMed Search)
Posted: 10/27/2017 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Some pediatric practitioners have adopted the oxygenation index (OI) ([FiO2 × mean airway pressure (Paw) × 100]/ PaO2) or oxygen saturation index (OSI) ([FiO2 × Paw × 100]/ SpO2) to assess hypoxemia in children instead of P/F ratios because of the less standardized approach to positive pressure ventilation in children relative to adults.
OI can be used in pediatric patients to define severity of Acute Respiratory Distress Syndrome (ARDS) in patients receiving invasive mechanical ventilation and assess for potential ECMO treatment.
In contrast, the P/F ratio should be used to diagnose Pediatric ARDS for patients receiving noninvasive continuous positive airway pressure [CPAP] or bilevel positive airway pressure [BiPAP]) with a minimum CPAP of 5 cm H2O.
Oxygen Index (OI) = FiO2 x MAP x 100
---------------------
PaO2
Category: Pediatrics
Keywords: Trauma, hematuria, kidney injury (PubMed Search)
Posted: 10/13/2017 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Pediatrics
Keywords: ARDS, oxygenation index, OI, PALICC, acute lung injury (PubMed Search)
Posted: 9/22/2017 by Mimi Lu, MD
(Updated: 10/27/2017)
Click here to contact Mimi Lu, MD
Since the first description of acute respiratory distress syndrome (ARDS), various consensus conferences (including American-European Consensus Conference (AECC) and the Berlin Conference) have produced definitions focused on adult lung injury but have limitations when applied to children.
This prompted the organization of the Pediatric Acute Lung Injury Consensus Conference (PALICC), comprised of 27 experts, representing 21 academic institutions and eight countries. The goals of the conference were 1) to define pediatric ARDS (PARDS); 2) to offer recommendations regarding therapeutic support; and 3) to identify priorities for future research in PARDS.
Although there were several recommendations from the group, some notable ones, in contrast to the Berlin definition focused on adults, include: 1) use the Oxygenation Index (or, if an arterial blood gas is not available, the Oxygenation Severity Index) rather than the P/F ratio; 2) elimination of the requirement for “bilateral” pulmonary infiltrates (may be unilateral or bilateral) 3) elimination of specific age criteria for PARDS.
Tune in next month for pearls on management for children with PARDS...
Pediatric Acute Respiratory Distress Syndrome: Consensus Recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatric Acute Lung Injury Consensus Conference Group. Pediatr Crit Care Med. 2015 Jun;16(5):428-39
Collaborators: Jouvet P, Thomas NJ, Wilson DF, Erickson S, Khemani R, Zimmerman J, Dahmer M, Flori H, Quasney M, Sapru A, Cheifetz IM, Rimensberger PC, Kneyber M, Tamburro RF, Curley MA, Nadkarni V, Valentine S, Emeriaud G, Newth C, Carroll CL, Essouri S, Dalton H, Macrae D, Lopez-Cruces Y, Quasney M, Santschi M, Watson RS, Bembea M.
Category: Pediatrics
Keywords: allergic reaction, anaphylaxis, auto-injector, epi-pen (PubMed Search)
Posted: 1/27/2017 by Mimi Lu, MD
(Updated: 8/25/2017)
Click here to contact Mimi Lu, MD
Anaphylaxis is a life threatening emergency with mortality of up to 2% [1]. Early recognition is imperative and administration of timely Epinephrine is the single most important intervention [2]. While providers may be hesitant to administer epinephrine in older patients due to fear of precipitating adverse cardiovascular events, they may also hesitate in younger patients due to fear of overdose.
Iimmediate administration with any dose available is recommended because:
Bottom line:
There are no absolute contraindications (including age) for epinephrine in patients with anaphylaxis. Give the initial dose IM into the anterolateral thigh.
1- Bock SA, Muñoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol. 2001 Jan. 107(1):191-3. [Medline].
4- Wood JP, Traub SJ, Lipinski C. Safety of epinephrine for anaphylaxis in the emergency setting. World Journal of Emergency Medicine. 2013;4(4):245-251. doi:10.5847/wjem.j.issn.1920-
