Category: Neurology
Keywords: MRA, MRV, non-contrast, contrast-enhanced, gadolinium, time-of-flight, TOF (PubMed Search)
Posted: 6/8/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Gadolinium - To Use or Not Use?
| Non-Contrast MRA/MRV | Contrast-Enhanced MRA/MRV | |
| How Does It Work? | * Time-of-flight (TOF) is a commonly used sequence * Relies on flow of blood into imaging plane * Difference between signal of blood and suppressed background tissue | * Similar to CT angiography/venography * Higher intravascular signal purely from gadolinium-based contrast, not dependent on flow
|
| Pros | * Does not require contrast
| * Generally better image quality * Shorter acquisition time |
| Cons | * Slow, turbulent, or retrograde flow may result in signal loss * Over-estimates stenosis * Longer acquisition time | * RIsks associated with contrast use * Timing of image acquisition important |
| Applications | * Patients with allergy to gadolinium, renal dysfunction, pregnancy * Evaluation of intracranial vessels and cerebral venous system | * Evaluation of stenoses and occlusions of the neck vessels and their origins at the aortic arch
|
Follow me on Twitter @ EM_NCC
Category: Neurology
Keywords: magnetic resonance imaging, MRI, T1, T2, FLAIR, DWI, ADC (PubMed Search)
Posted: 5/11/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Want to learn more about how to read a brain MRI? Here are the basics:
Stay tuned for more pearls in this series on brain MRI!
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: dizzy, dizzinesss, acute vestibular syndrome, triggered episodic vestibular syndrome, spontaneous episodic vestibular syndrome, HINTS, Dix-Hallpike (PubMed Search)
Posted: 4/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
What Do You Mean By Dizzy?
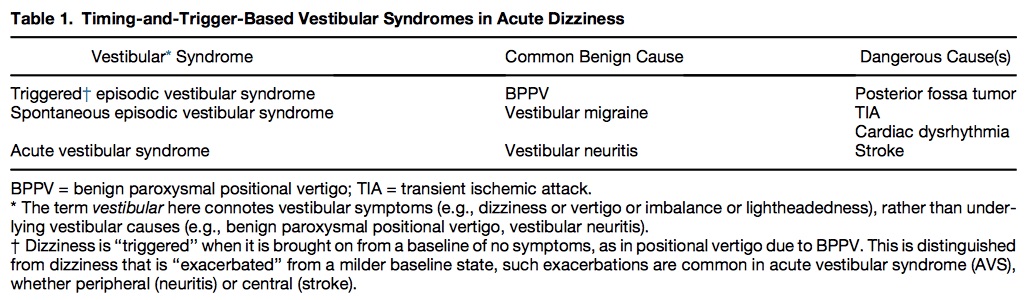
Table 1 shows common benign and serious causes of these vestibular syndromes.
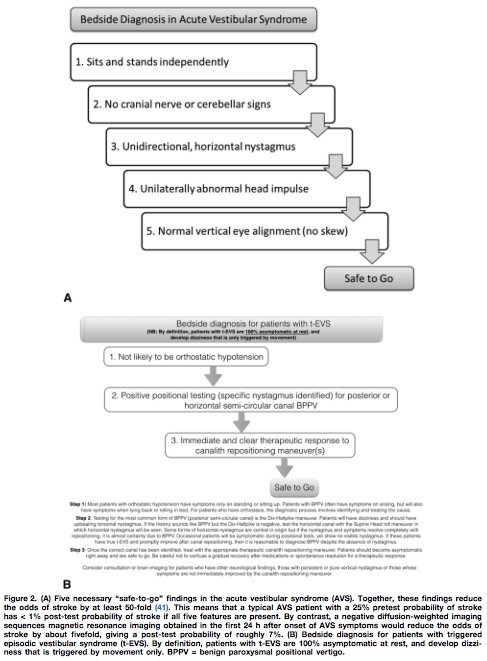
Utilizing the HINTS battery or the Dix-Hallpike maneuver, a “safe to go” algorithm for acute vestibular syndrome and triggered episodic vestibular syndrome is outlined in Figure 2.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Up-gaze paresis, ophthalmoparesis, hydrocephalus, shunt malfunction (PubMed Search)
Posted: 3/9/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Sunset Eye Sign
Category: Neurology
Keywords: cerebral venous thrombosis, CVT, venography, CTV, MRV (PubMed Search)
Posted: 2/10/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: CT venography is good for diagnosing CVT, but MRI/MRV is superior for detection of isolated cortical venous thromboses and assessing parenchymal damage.
Bonneville F. Imaging of cerebral venous thrombosis. Diagn Interv Imaging. 2014;95:1145-1150.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Traumatic brain injury, psychiatric disorders, anxiety, depression (PubMed Search)
Posted: 1/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line:
Scholten AC, Haagsma JA, Cnossen MC, et al. Prevalence and risk factors of anxiety and depressive disorders following traumatic brain injury: a systematic review. J Neurotrauma. 2016 Jan 5. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Stroke, NIH stroke scale, NIHSS (PubMed Search)
Posted: 12/9/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
A recent study compared the original NIHSS with the shortened 11, 8, and 5 item versions.4
Bottom Line: The original 15-item NIHSS should still be used to evaluate patients’ stroke severity.
The reliability of the NIHSS has been found to improve with personal and videotaped training.
Follow me on Twitter @ EM_NCC
Category: Neurology
Keywords: serotonin syndrome, SSRI, cyproheptadine (PubMed Search)
Posted: 11/11/2015 by WanTsu Wendy Chang, MD
(Updated: 11/12/2015)
Click here to contact WanTsu Wendy Chang, MD
Last month we discussed causes of serotonin syndrome including common ED medications such as cyclobenzaprine (Flexeril), tramadol (Ultram), metoclopramide (Reglan), and ondansetron (Zofran).
Let’s conclude this series and discuss how to treat serotonin syndrome:
This concludes our 3-part series on serotonin syndrome!
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: serotonin syndrome, SSRI, SNRI, MAOI, TCA (PubMed Search)
Posted: 10/14/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Last month we discussed symptoms of serotonin syndrome and its diagnosis by the Hunter Criteria. Let's move on to what causes serotonin syndrome.
Serotonin Syndrome - What Causes It?

** Stay tuned for the conclusion on management of serotonin syndrome **
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: serotonin syndrome, SSRI, autonomic hyperactivity, hyperreflexia, clonus, Hunter Criteria (PubMed Search)
Posted: 9/9/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Serotonin Syndrome - What is It?
** Stay tuned for part 2 on what causes serotonin syndrome **
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: insular ribbon sign, MCA stroke, early CT sign of stroke (PubMed Search)
Posted: 8/12/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
Neuroimaging Tip - Loss of the Insular Ribbon Sign
Category: Neurology
Keywords: CSF shunts, VP shunt, VA shunt, LP shunt (PubMed Search)
Posted: 7/8/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Cerebrospinal Fluid (CSF) Shunts
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Guidelines, intracerebral hemorrhage, ICH score, communication (PubMed Search)
Posted: 6/10/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
What is the ICH Score?
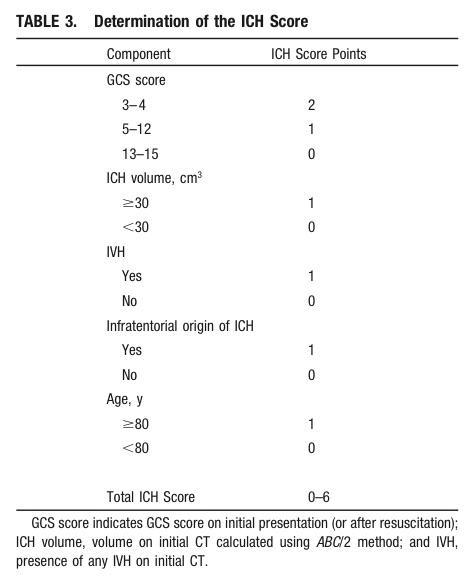
Take Home Point: Communicate the severity of your ICH patient by using either the composite ICH Score or by including details such as the patient's GCS, estimated volume of ICH, presence of IVH, and supra- vs. infratentorial origin.
1) Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015 May 28. [Epub ahead of print]
2) Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH Score: A simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32(4):891-897.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Glasgow Coma Scale, GCS, traumatic brain injury, TBI, survey (PubMed Search)
Posted: 5/13/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Are We Using the Glasgow Coma Scale Reliably?
| Reported by Responders | |
| Patient population in which GCS is used | Traumatic brain injury (96%) Other neurological disorders (78%) |
| Intended purpose of GCS | Classification of severity of injury (51%) Serial evaluation of patient over time (33%) Clinical decision making (44%) Prognostication (17%) |
| Application of stimulus | Both arms and legs (62%) Only arms (37%) |
| Type of stimuli used | Nail bed pressure (57%) Lateral side of finger (22%) Supra-orbital nerve pressure (52%) Trapezius or pectoralis pinch (50%) Sternal rub (53%) Retromandibular stimulation (24%) Earlobe stimulation (16%) |
| Reporting of GCS | Description in words, e.g. no eye opening, no motor (19%) Numerical report, e.g. E1V1M1 (46%) Sum score, e.g. EVM=3 (35%) |
Bottom line: There are variations in the application, assessment, and reporting of the GCS. A standardized approach is needed for it to be a reliable assessment and communication tool.
Reith FCM, Brennan PM, Maas AIR, Teasdale GM. Lack of standardization in the use of the Glasgow Coma Scale: Results of international surveys. J Neurotrauma. 2015; May 7. [Epub ahead of print]
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH score, prognostication, early decisions to limit medical treatment (PubMed Search)
Posted: 4/8/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
Prognostication in intracerebral hemorrhage - A self-fulfilling prophecy?
The ICH Score is a validated outcome prediction model for intracerebral hemorrhage (ICH) developed from clinical and neuroimaging characteristics on presentation.
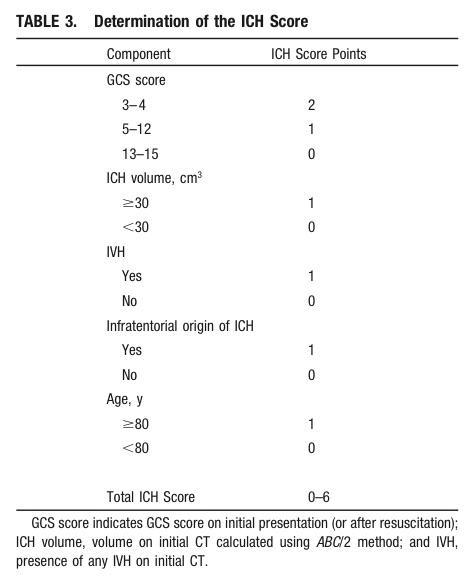
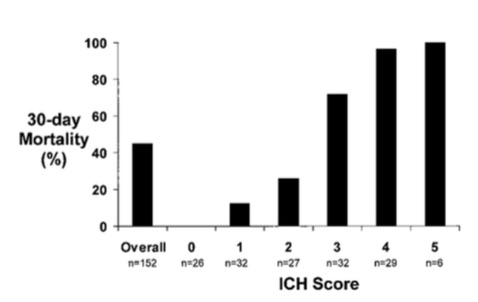
While predictive models are often used in clinical care for prognostication, is it a self-fulfilling prophecy to make early decisions to limit medical treatments based on these models?
Morgenstern et al. conducted an observational study across 5 hospitals looking at 30-day mortality of patients with ICH with initial GCS <12 who received full medical care for at least 5-days following symptom onset.
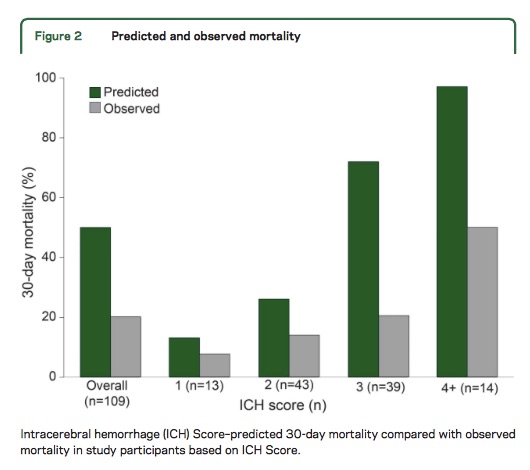
Take Home Point: The ICH Score is a useful tool for stratifying patient severity, but one should be cautious in using the model to provide specific numerical values as outcome predictions.
Hemphill JC, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH Score. A simple, reliable grading scale for intracerebral hemorrhage. Stroke 2001;32:891-897.
Morgenstern LB, Zahuranec DB, Sanchez, BN, et al. Full medical support for intracerebral hemorrhage. Neurology 2015;84:1-6.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: cardiac arrest, subarachnoid hemorrhage, intracerebral hemorrhage, ischemic stroke, seizure (PubMed Search)
Posted: 2/25/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Neurologic causes of cardiac arrest have not been well described. Two recent retrospective studies looked at the epidemiology and clinical features of these patients.
Hubner P. et al.
Arnaout M. et al.
Neurologic causes of cardiac arrest are uncommon presentations that may be difficult to distinguish from cardiac etiology of cardiac arrest. If history and clinical presentation suggests a neurologic cause, obtain a non-contrast head CT for evaluation.
Hubner P, Meron G, Kurkciyan I, et al. Neurologic causes of cardiac arrest and outcomes. J Emerg Med. 2014;47(6):660-667.
Arnaout M, Mongardon N, Deye N, et al. Out-of-Hospital Cardiac Arrest from Brain Cause: Epidemiology, Clinical features, and Outcome in a Multicenter Cohort. Crit Care Med. 2015;43(2):453-460.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: acute ischemic stroke, magnesium, neuroprotectant, IMAGES, FAST-MAG (PubMed Search)
Posted: 2/12/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Magnesium, another failed neuroprotectant?
Stroke is a leading cause of adult disability and the second leading cause of death worldwide. Currently available therapies for acute ischemic stroke are based on restoring perfusion to the ischemic penumbra. However, they are only moderately effective.
A series of pathological cascades leading to neuronal death are triggered in acute ischemia. Thus it may be logical to suggest that if one can interrupt the propagation of these cascades, perhaps part of the brain tissue can be protected and salvaged.
Magnesium has been shown in various animal models to have pluripotent neuroprotective properties. It is also widely available, simple to administer, and has a favorable risk profile. A prior study of magnesium in acute ischemic stroke (IMAGES) did not show a benefit when the agent was administered a median 7.4 hours after symptom onset. However, a subgroup of patients treated within 3 hours of symptom onset showed possible benefit.
The Field Administration of Stroke Therapy - Magnesium (FAST-MAG) trial, funded by the NIH, looked at magnesium administered within 2 hours after symptom onset on the degree of disability at 90 days after stroke as measured by the modified Rankin scale.
Magnesium was not found to have any benefit in functional outcome at 90 days.
This study was unique in several ways:
However, despite this study being very well executed, demonstrating the feasibility of conducting a phase 3 trial with targeted intervention within the hyperacute window, it is another neuroprotective agent that failed to translate from the laboratory bench to the clinical realm.
Potential explanations for the discrepancies between preclinical and clinical outcomes of neuroprotective agents thus far include discrepancies on outcome measures, functional assessments, pre-morbid conditions, therapeutic windows, and drug-dosing schedules between animal studies and clinical trials.
Take Home Point: Magnesium does not have any clear benefit in acute ischemic stroke at this time.
Muir KW, Lees KR, Ford I, et al. Magnesium for acute stroke (Intravenous Magnesium Efficacy in Stroke trial): a randomised controlled trial. Lancet. 2004;363(9407):439-445.
Saver JL, Starkman S, Eckstein M, et al. Prehospital use of magnesium as neuroprotection in acute stroke. N Engl J Med. 2015;372(6):528-536.
Cheng YD, Al-Khoury L, Zivin JA. Neuroprotection for ischemic stroke: two decades of success and failure. NeuroRx. 2004;1(1):36-45.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: traumatic brain injury, progesterone, neuroprotectant, clinical trials, PROTECT III, SYNAPSE (PubMed Search)
Posted: 1/14/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Is progesterone yet another disappointing neuroprotectant?
Traumatic brain injury (TBI) affects more than 1.7 million persons in the U.S. annually. The incidence of TBI is increasing globally, especially in developing countries. Despite improvement in trauma systems and critical care, the morbidity and mortality associated with severe TBI remain high.
Progesterone has been shown in preclinical and phase 2 randomized clinical trials to have pluripotent neuroprotective properties and improve mortality in TBI.
Two multicenter phase 3 trials were recently completed and published in the December 25th issue of the New England Journal of Medicine. However, their results were disappointing.
Both studies used the Glasgow Outcome Scale (GOS) or Extended Glasgow Outcome Scale (GOS-E) at 6 months as their primary outcome. The GOS and GOS-E capture the degree of recovery from brain injury in terms of disability, stratified into levels by death, vegetative state, severe disability, moderate disability, and good recovery.
Progesterone was not found to have any benefit in functional outcome at 6 months.
Both of these studies were well designed and conducted. However, they were based on small effect sizes of the phase 2 trials. In addition, they had very favorable outcome rates in the placebo group, thereby making it hard to demonstrate a benefit by their sample sizes.
There has been a long history of failed neuroprotectant trials likely due to the complex and variable injury mechanisms involved in TBI. The currently available outcome measures are also insensitive to the targeted mechanistic endpoints. More research is needed to understand not only potential therapies but also how to select appropriate patients for these therapies.
Take Home Point: Progesterone does not have any clear benefit in TBI at this time.
Wright DW, Yeatts SD, Silbergleit R, et al. Very early administration of progesterone for acute traumatic brain injury. N Engl J Med. 2014;371(26):2457-2466.
Skolnick BE, Maas AI, Narayan RK, et al. A clinical trial of progesterone for severe traumatic brain injury. N Engl J Med. 2014;371(26):2467-2476.
Category: Neurology
Keywords: clinical decision support, clinical decision rules, head CT, mild traumatic brain injury (PubMed Search)
Posted: 12/10/2014 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Does clinical decision support help reduce head CT utilization in mild traumatic brain injury related ED visits?
Are we utilizing clinical decision rules adequately to help us appropriately select patients for CT imaging?
Can clinical decision support (CDS) help us reduce head CT utilization in mTBI related ED visits?
Take Home Point:
Clinical decision support may be a useful tool to help reduce CT utilization in mild TBI related ED visits.
Ip IK, Raja AS, Gupta A, et al. Impact of clinical decision support on head CT use in patients with mild traumatic brain injury in the emergency department. Am J Emerg Med 2014; Nov 13 [epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: anisocoria, Horner syndrome, third nerve palsy, tonic pupil (PubMed Search)
Posted: 11/12/2014 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Anisocoria, or unequal pupil sizes, is a common condition. Approximately 20% of the normal population have physiologic anisocoria. However, pathologic anisocoria indicates disease of the iris, parasympathetic pathway or sympathetic pathway. A systematic approach to the evaluation of anisocoria can help differentiate between etiologies that range from benign to life threatening.
The most important question in the evaluation of anisocoria is whether both pupils are normally reactive to light or is one (or both) poorly reactive. If both pupils are reactive, the smaller pupil is abnormal and the lesion is likely in the sympathetic pathway because pupillary constriction (parasympathetic pathway) is intact. If one pupil is poorly or non-reactive (and there is no relative afferent pupillary defect), the larger pupil is abnormal and the lesion is likely in the parasympathetic pathway.
DDx of anisocoria with normally reactive pupils:
DDx of anisocoria with poorly or non-reactive pupil:
Kedar S, Biousse V, Newman NJ. Approach to the patient with anisocoria. In: UpToDate, Brazis, PW (Ed), UpToDate, Waltham, MA, 2014. (Accessed on November 12, 2014.)
Lam BL, Thompson HS, Corbett JJ. The prevalence of simple anisocoria. Am J Ophthalmol 1987;104(1):69-73.
