Category: Neurology
Keywords: occipital nerve block, migraine, headache (PubMed Search)
Posted: 2/14/2018 by WanTsu Wendy Chang, MD
(Updated: 2/15/2018)
Click here to contact WanTsu Wendy Chang, MD
Zhang H, Yang X, Lin Y, Chen L, Ye H. The efficacy of greater occipital nerve block for the treatment of migraine: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2018;165:129-133.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: RCVS, thunderclap headache, migraine, SAH (PubMed Search)
Posted: 1/10/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider RCVS in the differential of thunderclap headache and in patients who present with worse than usual migraine headache.
Arrigan MT, Heran MKS, Shewchuk JR. Reversible cerebral vasoconstriction syndrome: an important and common cause of thunderclap and recurrent headaches. Clin Radiol. 2017 Dec 21 [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: DAWN, thrombectomy, mismatch, wake-up, stroke, penumbra (PubMed Search)
Posted: 12/13/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The use of neuroimaging to identify an ischemic penumbra that may benefit from thrombectomy may be considered even for patients with time of last known well beyond 6 hours.
Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2017 Nov 11. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: aphasia, stroke, middle cerebral artery, MCA, mimic, NIHSS (PubMed Search)
Posted: 11/8/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Take Home Point: This small but interesting study looked at the incidence of isolated aphasia presenting for concern of stroke. They found that none of their patients had evidence of an infarct, suggesting that strokes affecting language without motor or sensory deficits are uncommon.
Casella G, Llinas RH, Marsh EB. Isolated aphasia in the emergency department: The likelihood of ischemia is low. Clin Neurol Neurosurg 2017:163:24-26.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: traumatic brain injury, TBI, fall, subdural hematoma, SDH, elderly (PubMed Search)
Posted: 10/11/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Traumatic brain injury (TBI) is associated with close to half of major trauma admissions in adults over age 65 in the U.K.
Falls accounted for 85% of all TBIs, while 45% of patients had subdural hematomas (SDH).
More than 3/4 of patients were treated conservatively, though outcomes were not significantly better than those who underwent neurosurgical intervention.
Higher age is associated with higher mortality and greater disability.
Bottom Line: Trauma in older adults is increasing and fall prevention is important in reducing significant injuries.
Hawley C, Sakr M, Scapinello S, et al. Traumatic brain injuries in older adults - 6 years of data for one UK trauma centre: retrospective analysis of prospectively collected data. Emerg Med J 2017;0:1-8.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: seizure, status epilepticus, benzodiazepine, RAMPART, pediatric (PubMed Search)
Posted: 9/13/2017 by WanTsu Wendy Chang, MD
(Updated: 9/14/2017)
Click here to contact WanTsu Wendy Chang, MD
IV vs. Non-IV Benzodiazepines for Cessation of Seizures
Follow me on Twitter @ EM_NCC
Category: Neurology
Keywords: meningitis, CSF, glucose, glucometer (PubMed Search)
Posted: 8/24/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Category: Neurology
Keywords: Terson syndrome, vitreous hemorrhage, intraocular hemorrhage, subarachnoid hemorrhage (PubMed Search)
Posted: 7/12/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
50 YOF with acute onset of worst headache of life associated with nausea and vomiting. Patient is somnolent, will rouse to noxious stimuli and complains of a headache as well as decreased vision.
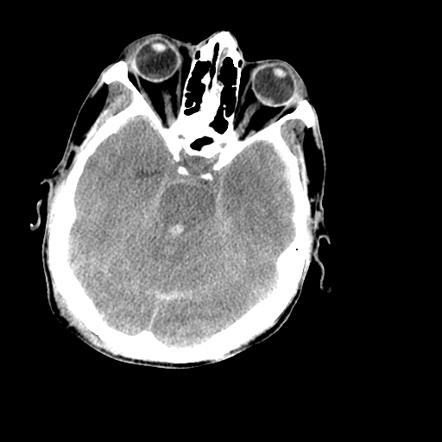
Image courtesy of Dr. Nasir Siddiqui, Radiopaedia.org. From the case rID: 36469
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: seizure, electroencephalogram, EEG, epilepsy, antiepileptic (PubMed Search)
Posted: 6/14/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
What is the role of EEG for first-time seizures in the ED?
Take Home Point: A 30-minute routine EEG in the ED in adults with an uncomplicated first-time seizure revealed a substantial number of epilepsy diagnosis and can change ED management with immediate initiation of antiepileptic medication.
Background:
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: vasogenic cerebral edema, white matter, blood-brain-barrier, steroids (PubMed Search)
Posted: 4/26/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Case image courtesy of Dr David Cuete, Radiopaedia.org, rID: 23178
Follow me on Twitter @EM_NCC!
Category: Neurology
Keywords: Glasgow Coma Scale, GCS, motor GCS, mGCS, Simplified Motor Scale, SMS (PubMed Search)
Posted: 4/12/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The motor GCS and Simplified Motor Scale (SMS) have similar discrimination when compared with the total GCS, and may be easier to use.
Chou R, Totten AM, Carney N, et al. Predictive Utility of the Total Glasgow Coma Scale Versus the Motor Component of the Glasgow Coma Scale for Identification of Patients with Serious Traumatic Injuries. Ann Emerg Med. 2017 Jan 11. [Epub ahead of print].
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: headache, migraine, intravenous fluids, IVF (PubMed Search)
Posted: 3/8/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: aphasia, fluency, comprehension, repetition, Broca's aphasia, Wernicke's aphasia, conduction aphasia (PubMed Search)
Posted: 2/8/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Types of aphasia [Online image]. Retrieved February 8, 2017 from https://www.aphasia.org/
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: concussion, driving performance, cognitive impairment (PubMed Search)
Posted: 1/11/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Schmidt JD, Hoffman NL, Ranchet M, et al. Driving after concussion: Is it safe to drive after symptoms resolve? J Neurotrauma. 2016 Dec 13. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: pharmacist, thrombolysis, door-to-needle time, acute ischemic stroke (PubMed Search)
Posted: 12/14/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Impact of an ED pharmacist on time to thrombolysis in acute ischemic stroke
Montgomery K, Hall AB, Keriazes G. Impact of an emergency medicine pharmacist on time to thrombolysis in acute ischemic stroke. Am J Emerg Med 2016;34:1997-9.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: subarachnoid hemorrhage, mimic, pseudosubarachnoid hemorrhage, cerebral edema (PubMed Search)
Posted: 11/9/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Patient found pulseless after submersion in water for 20 minutes. After ROSC, patient’s GCS was 3 and pupils are dilated and nonreactive.

Kim JM, Eom TH. The pseudosubarachnoid hemorrhage: clinical implications of subarachnoid hemorrhage misdiagnosis. Pediatr Emerg Care. 2016 May 12. [Epub ahead of print]
Category: Neurology
Keywords: Brain Trauma Foundation, BTF, guideline, traumatic brain injury, TBI (PubMed Search)
Posted: 10/12/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Updated Guidelines for Traumatic Brain Injury
The Brain Trauma Foundation (BTF) Guidelines for the Management of Severe Traumatic Brian Injury (TBI) was recently updated and published in September 2016.
Updated recommendations include:
For the executive summary and complete guidelines, go to https://braintrauma.org/guidelines/guidelines-for-the-management-of-severe-tbi-4th-ed#/
Category: Neurology
Keywords: eyelid apraxia, eye opening apraxia (PubMed Search)
Posted: 9/14/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Category: Neurology
Keywords: Uncal herniation, ipsilateral hemiplegia, Kernohan's notch, Kernohan's sign (PubMed Search)
Posted: 8/10/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD

Diagram modified from "Localised Neurological Disease and Its Management A Intracranial". clinicalgate.com/localised-neurological-disease-and-its-management-a-intracranial/. Accessed 10 Aug 2016.
Follow me on Twitter @EM_NCC
Category: Neurology
Keywords: Large vessel occlusion stroke, endovascular intervention, Field Assessment Stroke Triage for Emergency Destination, FAST-ED, NIHSS, Rapid Arterial Occlusion Evaluation, RACE, Cincinnati Prehospital Stroke Severity scale, CPSS (PubMed Search)
Posted: 7/13/2016 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
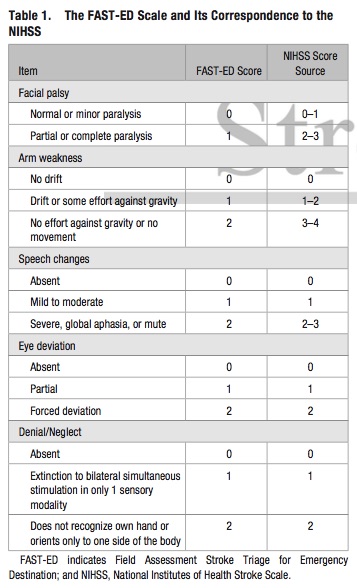
Bottom Line: Additional assessment of gaze deviation, aphasia and neglect, as included in the FAST-ED scale, increases the accuracy of predicting LVOS.
Follow me on Twitter @EM_NCC
