Category: Toxicology
Keywords: toxins, misperceived for edible, food containers (PubMed Search)
Posted: 2/4/2026 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD

Poisonings due to storage in a secondary container reported to the National Poison Data System, 2007–2017. Carpenter J., Murray B. et al., Clinical Toxicology, 2021.59(6), 521–527.
Poisoning following exposure to chemicals stored in mislabelled or unlabelled containers: a recipe for potential disaster. Millard YC, Slaughter RL, et al. New Zealand Med J. 26 September 2014, Vol 127 No 1403.
Unintentional poisoning from decanted toxic household chemicals. Von Fabeck K, Boulamery A, et al. Clin Toxicol (Phila). 2023 Mar;61(3):186-189.
Antifreeze on a freezing morning: ethylene glycol poisoning in a 2-year-old. Hann G, Duncan D, et al. BMJ Case Rep. 2012 Mar
Epidemiology of Accidental Poisoning Caused by Storage of Non-Food Substances in Food Containers and unmarked Bottles/Containers. Geller RJ, Kezirian R, Bangar P, Strong D, Carlson T. Children’s Hospital Central California; California Poison Control System (CPCS). https://www.tandfonline.com/doi/pdf/10.1080/15563650903076924
Category: Toxicology
Keywords: Water beads, foreign body ingestion, gastrointestinal obstruction (PubMed Search)
Posted: 1/7/2026 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
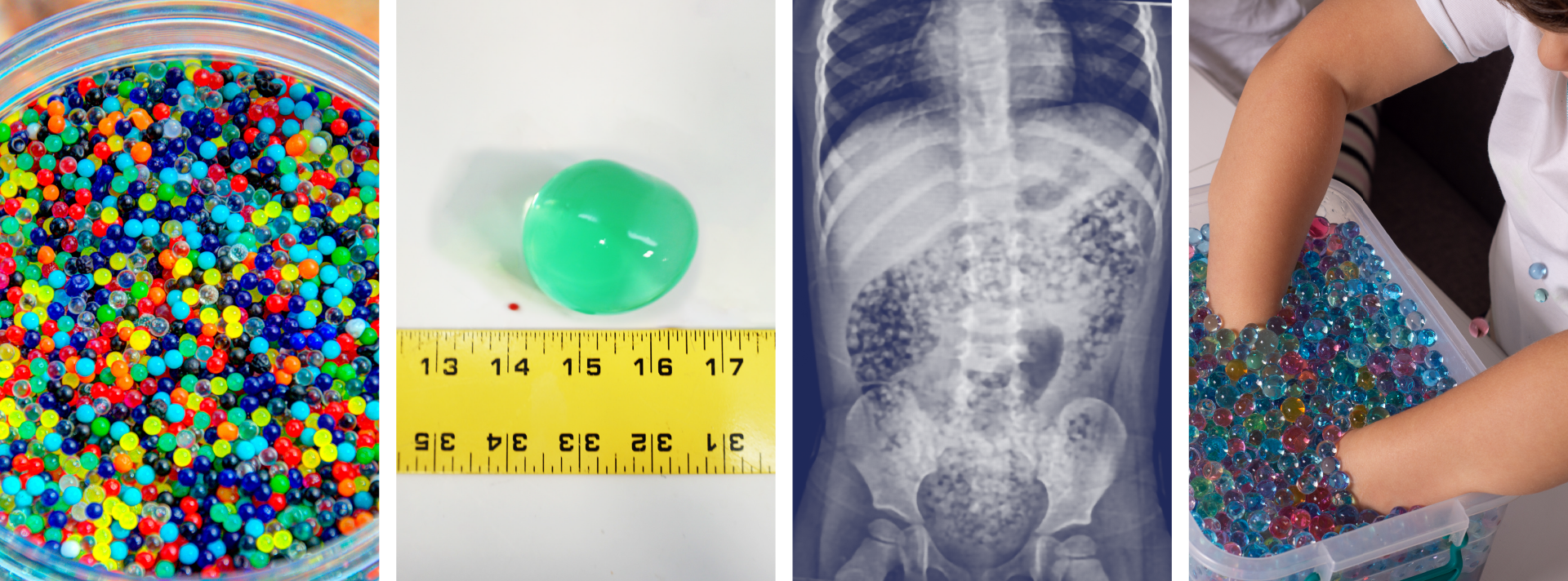
Water beads are a colorful, fun, popular, and widely available product found in children’s toys, stress squeeze balls, arts and crafts supplies, plant hydration products, air fresheners, and first aid ice packs.
These jelly-like small super-absorbent polymer balls are similar to the material found in diapers and absorb water expanding 100-800 percent of original size.
Pediatric ingestion is by far the most common poisoning exposure route but insertion into ears and nose and aspiration can occur and has led to serious adverse effects. More than 8000 water bead-related ingestion injuries have been treated in U.S. Emergency Departments.
Over the past 10 years, U.S. Poison Centers reported 19,660 exposures with 55% occurring in 2023 alone. In the majority of cases, no clinical effects (~88%) were seen, however in >11% of cases mild to moderate effects (abdominal discomfort, nausea, and vomiting) were reported and severe effects including complete bowel obstruction, necrosis, and surgical intervention in 0.11%. The Consumer Product Safety Commission reported at least one death of a 10-month-old girl in 2023 due to water bead ingestion.
Ingested water beads quickly pass into the small intestines where they continue to expand over the next few days and can become large enough (especially in children less than 2 year of age) to be unable to pass through the ileocecal valve causing small bowel obstruction requiring surgical intervention.
There is little data to guide management after ingestion. The majority of cases have no clinical effects and home observation is appropriate for asymptomatic for patients greater than 2 years. Recommendations from a report of case series and literature review , in patients less than 2 years of age with evidence of ingestion and symptomatic patients include hospitalization, imaging with US or CT, and close monitoring. CT, ultrasound, and endoscopy are not 100% reliable and often do not visualize these intraluminal foreign bodies.
In December 2025, the CPSC approved new federal safety standards for water beads toys setting limits on maximum expansion size of beads and amount of allowable acrylamide.
Risks of Water Bead Ingestion. Reeves PT, Pasman EA Pediatrics February 2025; 155 (2): e2024069447. 10.1542/peds.2024-069447
Water bead injuries by children presenting to emergency departments 2013-2023: An expanding issue. ?Pasman EA, Khan MA, et al. J Pediatr Gastroenterol Nutr. 2024 Sep;79(3):752-757. doi: 10.1002/jpn3.12333. Epub 2024 Jul 24. PMID: 39045753.
Pediatric water bead-related visits to United States emergency departments, Joynes HJ, Kistamgari S, et al. The American Journal of Emergency Medicine, Volume 84, 2024, Pages 81-86, ISSN 0735-6757, https://doi.org/10.1016/j.ajem.2024.07.048.
Water beads: Expanding toy and ‘new’ problem for paediatric surgeons and community. Bollettini, T., Mogiatti, M., et al. J Paediatr Child Health, 61: 204-208. 2025. https://doi.org/10.1111/jpc.16730
Aspiration of superabsorbent polymer beads resulting in focal lung damage: a case report. Alharbi N, Dabbour M. BMC Pediatr. 2020 May 29;20(1):262. doi: 10.1186/s12887-020-02168-9. PMID: 32471401; PMCID: PMC7257448.
Category: Toxicology
Keywords: Nitrous Oxide, Whippit, unregulated psychotropic, inhalant abuse (PubMed Search)
Posted: 12/2/2025 by Kathy Prybys, MD
(Updated: 12/3/2025)
Click here to contact Kathy Prybys, MD

Vohra V, Matthews H, Stroh-steiner G. Notes from the field: Recreational Nitrous Oxide Use-Michigan, 2019-2023. MMWR Morb Mort Wkly Rep 2025;74:210-212. DOI: http://dx.doi.org/10.15585/mmwr.mm7412a3.
Gummin D, Mowry J, Beuhler MC, et.al (17 Dec 2024): 2023 Annual Report of the National Poison Data System® (NPDS) from America’s Poison Centers®: 41st Annual Report, Clinical Toxicology, DOI: 10.1080/15563650.2024.2412423
Yockey RA, Hoopsick RA. US Nitrous Oxide Mortality. JAMA Netw Open. 2025;8(7):e2522164. doi:10.1001/jamanetworkopen.2025.22164.
https://www.fda.gov/food/alerts-advisories-safety-information/fda-advises-consumers-not-inhale-nitrous-oxide-products. FDA Advises Consumers Not to Inhale Nitrous Oxide Products 6/4/2025
Category: Toxicology
Keywords: Cyanide, antidote, hydroxycobalmin, drug shortage (PubMed Search)
Posted: 11/5/2025 by Kathy Prybys, MD
(Updated: 2/9/2026)
Click here to contact Kathy Prybys, MD
Cyanide is one of the deadliest known poisons causing immediate toxic effects and lethality within seconds to minutes. Exposures are rare, most commonly by inhalational route (HCN gas) from structural fires due to combustion of synthetic materials or from ingestion of cyanide salts. Cyanide toxicity can also occur from dermal or parental (sodium nitroprusside) exposure.
The preferred first line antidote is hydroxycobalamin (vitamin B12) available as Cyanokit, which has higher affinity for cyanide than cytochrome oxidase and binds to form harmless cyanocobalamin and is renally excreted. Limited studies reveal good survival rates in noncardiac arrest patients. Hydroxycobalamin has minimal side effects (red skin and urine, increased BP) and is well-tolerated with safer and simpler mechanism of action than Nithiodote (original antidote), containing sodium nitrite (CN preferentially binds methemoglobin to form cyanomethemoglobin) and thiosulfate (provides sulfur to convert cyanide to thiocynate for excretion). Sodium nitrite has numerous adverse effects causing hypotension and methemoglobin (contraindicated in smoke inhalation victims due to concern for carbon monoxide poisoning, G6PD deficiency, preexisting amenia), and hypersensitivity reactions. Sodium thiosulfate has less side effects and augments cyanide excretion but is considered less effective due to its slow onset, short half-life, low volume of distribution, and poor intracellular penetration.
As of August 2025, the American Society of Health -System Pharmacists (ASHP) Drug Shortage lists Cyanokit as “limited availability” in the U.S. as manufacturing was suspended due to investigation of ongoing quality defect with concern for sterility and endotoxin content. Impacted batches were released and their numbers are listed in an FDA bulletin (see references). Healthcare providers should weigh the potential benefit of using Cyanokit against the risk of infection. Infusion set with 0.2 micron in line filter can be temporarily used for administration of Cyanokit 5 mg hydroxycobalmin to prevent potential infection.
Surviving Cyanide Poisoning: A case report highlighting the role of early antidote use. Hopes BC, Slob EM, et al. Toxicology Reports, Volume 15, December 2025.
Challenges in the diagnosis of acute cyanide poisoning. Parker-Cote JL, Rizer J, et al. Clin Toxicol. 2018 Jul:56(7):609-617.
American Society of Health -System Pharmacists (ASHP) Drug Shortage Detail-Hydroxocobalmin for injection 9/22/2025.
February 6, 2025 Manufacturer letter to healthcare professional https://www.fda.gov/media/185400/download
Category: Toxicology
Keywords: Sudden sniffing death, Inhalants, Fluoridated Hydrocarbons (PubMed Search)
Posted: 6/27/2019 by Kathy Prybys, MD
(Updated: 7/5/2019)
Click here to contact Kathy Prybys, MD
Volatile inhalants such as glue, lighter fluid, spray paint are abused by "sniffing" (from container), "huffing" (poured into rag), or "bagging" (poured into bag). "Dusting" is the abuse of canned air dust removal products. These inexpensive easliy accessible products are so dangerous that manufacturers include product warnings regarding lethal consequences from misuse and even may indicate that a bitterant is added to discourage use. Common duster gases include the halogenated hydrocarbons, 1,1-difluoroethane or 1,1,1-trifluroethane which are highly lipid soluble and rapidly absorbed by alveolar membranes and distributed to CNS. Desired effect of euphoria and disinhibition rapidly occur but unwanted side effects include confusion, tremors, ataxia, pulmonary irritation, asphyxia and, rarely, coma.
"Sudden sniffing death" is seen within minutes to hours of use and is due to ventricular arrhythmias and cardiovascular collapse. Available experimental evidence postulates the following mechanisms: Inhibition of cardiac sodium, calcium, and repolarizing potassium channels hERG and I(Ks) causing reduced conduction velocity and altered refractory period leading to reentry arrythmias or myocardial "sensitiization" to catecholamines resulting in after depolarizations and enhanced automaticity. Treatment should include standard resuscitation measures but refractory arrythmias to defibrillation have been reported and use of amiodarone and beta blockers should be considered.
Bottom Line:

Sudden death involving inhalation of 1, 1-difluoroethane (HFC-152a) with spray cleaner: three case reports. K Sakai, K Maruyama-Maebashi, et.al. Forensic science Int. Volume 206, Issues 1–3, 20 March 2011.
Esmolol in treatment of severe arrhythmia after tricholoroethylene poisoning. Mortiz F. de La Chapelle, et al. Intensive Care Med. 2000 Feb;26(2):256.
Deaths Involving 1,1-Difluoroethane at the San Diego County Medical Examiner's OfficeVance C., Swalwell C., et al. Journal of Analytical Toxicology, Volume 36, Issue 9, November/December 2012.
Category: Toxicology
Keywords: Hypoglycemia, Drug induced (PubMed Search)
Posted: 5/16/2019 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Drug-induced hypoglycemia is an important cause of hypoglycemia which should be considered in any patient presenting with altered mental status. In one study, drug-induced hypoglycemia represented 23% of all hospital admissions attributed to adverse drug events. Risk factors for developing hypoglycemia include older age, renal or hepatic insufficiency, concurrent use of insulin or sulfonylureas, infection, ethanol use, or severe comorbidities. The most commonly cited drugs associated with hypoglycemia include:
*In Glipizide users, there was 2-3 fold higher odds of hypoglycemia with concurrent use of sulfamethoxale-trimethoprim, fluconazole, and levofloxacin compared with patients using Cephalexin.
**Tramadol potentially induces hypoglycemia by effects on hepatic gluconeogenesis and increasing insulin release and peripheral utlizilation. Was seen in elderly at initiation of therapy within first 30 days.
BOTTOM LINE:
Take care in prescribing drugs known to increase risk of hypoglycemia in elderly patients, with comorbidities, or those already taking medications associated with hypoglycemia.
Drug induced hypoglycemia, A Systematic Review. Hassan M. et al. J Clin Endo & Metab. 94(3) March 2009. 741-45.
Hypogylcemia after antimicrobial drug prescription for older patients using sulfonylureas. Parekh TM, Raji M, et al. JAMA Intern Med. 2014. 1605-12.
Tramadol Use and the Risk of Hospitalization for Hypoglycemia in Patients with Noncancer Pain. Fournier J, Azoulay L. et al. Jama Intern Med. 2015;175(2):186-193.
Hypoglycemic effects of tramadol analgesia in hospitalized patients: a case-control study. Golightly LK. Simendinger BA. et al. J Diabetes Metab Disord. 2017;16:30.
Category: Toxicology
Keywords: Scromboid, Histamine (PubMed Search)
Posted: 3/28/2019 by Kathy Prybys, MD
(Updated: 3/29/2019)
Click here to contact Kathy Prybys, MD
Scromboid (histamine fish poisoning) can be easily misdiagnosed since its' clinical presentation can mimic that of allergy. Seen most frequently in the summer and occurring with Scombroideafish (tuna, mackerel, bonito, skipjack) but also with large dark meat fish (sardines and anchovies) and even more commonly with nonscromboid fish such as mahi mahi and amber jack. In warm conditions when fish is improperly refrigerated, bacterial histidine decarboxylase converts muscle histidine into histamine which quickly accumulates. Histamine is heat stable and not destroyed with cooking.
Bottom Line:
Scromboid poisoning is due to histamine ingestion and is often misdiagnosed as allergic reaction. It is preventable with proper fish storage.
Severe scombroid fish poisoning: an underrecognized dermatologic emergency. Jantschitsch C, Kinaciyan T, et al. J Am Acad Dermatol 2011; 65:246–7.
Histamine fish poisoning: a common but frequently misdiagnosed condition. Attaran RR, Probst F. Emerg Med J 2002;19:474–5.
Category: Toxicology
Keywords: CT, Overdose, Pills (PubMed Search)
Posted: 2/21/2019 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
The primary tenet of poisoning treatment is to separate the patient from the poison. Gastric decontamination has been the cornerstone of poisoning treatment throughout history and methods include induced emesis, nasogastric suctioning, EGD or gastrostomy retrieval, activated charcoal, and whole bowel irrigation. Current guidelines for gastic decontamination are limited to few clinical situations. The detection of residual life threatening poisons in the stomach would be of value in predicting who might benefit from gastric decontamination in overdose.
Plain radiographs have variable sensitvity in detecting radioopaque pills. Computed tomography (CT) has been successful and gained wide acceptance in the detection of drug in body packers. In a recent study, authors studied the usefulness of non-contrast abdominal computed tomography for detection of residual drugs in the stomach in patients presenting over 60 minutes from acute drug overdose:
BOTTOM LINE:
Non-contrast CT may help to predict which patients would benefit from gastric decontamination in acute life-threatening drug poisonings.
Position paper update: gastric lavage for gastrointestinal decontamination. Benson B, Hoppu K, et al. Clin Toxicol. 2013;51:140–146.
American Academy of Clinical Toxicology & European Association of Poisons Centres and Clinical Toxicologists (2005) Position Paper: Single-Dose Activated Charcoal, Clinical Toxicology, 43:2, 61-87.
Are ingested lithium sulphate tablets visible on x-ray? A one-year prospective clinical survey. Höjer J, Svanhagen AC. 2012. Clinical Toxicology, 50:9, 864-865.
The usefulness of non-contrast abdominal computed tomography for detection of residual drugs in the stomach of patients with acute drug overdose, Yong Sung C, Seung-Whan C, et al. 2019. Clinical Toxicology.
Category: Toxicology
Keywords: Methylene Blue (PubMed Search)
Posted: 1/24/2019 by Kathy Prybys, MD
(Updated: 1/31/2019)
Click here to contact Kathy Prybys, MD
Most clinicians are familiar with use of methylene blue for the treatment of methemoglobinemia, as a urinary analgesic, anti-infective, and anti-spasmodic agent, or for its use in endoscopy as a gastrointestinal dye, but this compound also has a role as a rescue antidote in life threatening poisonings causing refractory shock states and other shock states.
Bottom Line:
Methylene blue should be considered when standard treatment of distributive shock fails.

Methylene Blue for Distributive Shock: a Potential New Use of An Old Antidote. Jang DH, Nelson LS, Hoffman RS. J Med Toxicol. 2013;9(3):242-9.
Methylene blue used in treatment of refractory shock resulting from drug poisoning. Fischer J. Taori G. et al. Clin Toxicol 2014 Jan;52(1) 63-65.
Calcium channel antagonist and beta blocker overdoses: antidotes and adjunct therapies. Graudins A, Lee HM, Druda D. Br J Clin Pharmacol. 2016 Mar 81(3):453-61.
A Review of Methylene Blue Treatment for Cardiovascular Collapse. Lo A, Jean CY, et al. Journal of Emerg Med. May 2014. Vol 46 (6): 670-679.
A Systematic Analysis of methylene Blue for Drug-Induced Shock. Warrick BJ, Tataru AP, Smolinske S. Clin Toxicol 2016 Aug;54(7):547-55.
Category: Toxicology
Keywords: Hyperemesis, Cannabinoid (PubMed Search)
Posted: 10/18/2018 by Kathy Prybys, MD
(Updated: 10/19/2018)
Click here to contact Kathy Prybys, MD
CHS Treatment:
Bottom line: Patient education should be provided on the paradoxical and recurrent nature of the symptoms of CHS to discourage relapse of use often stemming from false preception of beneficial effects of cannabis on nausea.
Cannabinoid hyperemesis: a case series of 98 patients. Simonetto DA, Oxentenko AS, et al,Mayo Clin Proc. 2012;87(2):114–9
Cannabinoid hyperemesis syndrome: potential mechanisms for the benfit of capsaicin and hot water hydrotherapy in treatment. Richards JR, Lapoint JM, et al. Clin Tox(phila) 2018 Jan :56(1): 15-24.
Cannabinoid Hyperemesis Syndrome: Public Health Implications and Novel Model Treatment Guidelines. West J Emerg Med. 2018 Mar:19(2):380-386.
Category: Toxicology
Keywords: Anticholinergic, Plant (PubMed Search)
Posted: 9/20/2018 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
A 19 year old male presents confused and very agitated complaining of seeing things and stomach pain. His friends report he ingested a naturally occurring plant to get high a few hours ago but is having a "bad trip". His physical exam :
Temp 100.3, HR 120, RR 14, BP 130/88. Pulse Ox 98%.
Skin: Dry, hot , flushed
HEENT: Marked mydriasis 6mm
Lungs: Clear
Heart: Tachycardic
Abdomen: Distended tender suprapubic with absent bowel sounds,
Neuro: Extremely agitated pacing, no muscular rigidity.
What has he ingested and what is the treatment?
 Datura stramonium, aka: Jimson Weed, flowers in the summer with white to violet trumpet petals, green irregular toothed leaves, and a green thorny round walnut sized seed pod (aka: thorn apple) the base of the stem. In the fall, the seed pods turn brown and split open to reveal chambers that are packed with dozens of small black seeds containing the anticholinergic tropane alkaloids, atropine, hyoscyamine, and scopolamine.
Datura stramonium, aka: Jimson Weed, flowers in the summer with white to violet trumpet petals, green irregular toothed leaves, and a green thorny round walnut sized seed pod (aka: thorn apple) the base of the stem. In the fall, the seed pods turn brown and split open to reveal chambers that are packed with dozens of small black seeds containing the anticholinergic tropane alkaloids, atropine, hyoscyamine, and scopolamine.
All parts of the plant are toxic and it has long been used in traditional medicine. Toxicity consists of anticholinergic toxidrome: Delirium and agitation, visual hallucinations, dry flushed skin, hyperthermia, mydriaisis, tachycardia, absent bowel sounds, urinary retention, remembered by the pneumonic "Red as a beet, hot as a hare, dry as a bone, blind as a bat, mad as a hatter, the bowel and bladder lose their tone, and the heart runs alone" . Toxicity is usually 12 hours but can be quite prolonged.
Treatment consists of :
-Gastric decontamination with activated charcoal and whole bowel irrigation for seed ingestion (seeds get caught up in gastric folds prolonging toxicity)
-IV Physostigmine, a reversible short acting acetylcholinesterase inhibitor increases acetylcholine at the synaptic clef, crosses the blood brain barrier, and is antidotal. Physostigmine has been demonstrated to be more effective and without significant complications when compared with benzodiazepines for the diagnosis and treatment of anticholinergic agitation and delirium. Usual dose is 0.5-2 mg with repeat dosages as needed.
Category: Toxicology
Keywords: Weakness (PubMed Search)
Posted: 8/2/2018 by Kathy Prybys, MD
(Updated: 8/31/2018)
Click here to contact Kathy Prybys, MD
A 68 year old male presents to the ED complaining of weakness to his legs. He states today his yard chores took him over 2 hours to complete instead of the usual 15-20 minutes due need to take frequent breaks for rest due to leg pain. He denied any chest pain or shortness of breath. Past medical history included hypercholesteremia, HTN, and CAD. He is taking aspirin and recently started on rosuvastatin.
His physical exam was unremarkable.
Results showed normal EKG and CBC. Bun was 70, Creatinine was 3.4, and CPK of 1025.
This patient has statin induced rhabdomyolysis and acute renal failure.
Take Home Points:
Category: Toxicology
Keywords: Sulfonylureas, Octreotide (PubMed Search)
Posted: 7/19/2018 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Sulfonylureas are commonly used oral hypoglycemic agents for type II diabetes. Agents on the market include glipizide (Glucotrol), glyburide (Micronase, Glynase, Dibeta) and glymepiride (Amaryl). These agents exert their effect by stimulation of insulin release from the pancreatic beta islet cells. Following overdose, hypoglycemia is usually seen within a few hours of ingestion and can be prolonged and profound. First line treatment for rapid correction of severe hypoglycemia is administration of an intravenous bolus of concentrated dextrose. However, use of dextrose infusion in attempt to maintain euglycemia is problematic as it can cause further release of insulin and rebound hypoglycemia. Octreotide ia a long acting synthetic somatostain analogue, blocks insulin secretion and has been shown to prevent recurrence of hypogylcemia better than placebo.
Bottom Line:
Comparison of Octreotide and standard therapy versus standard therapy alone for treatment of sulfonylurea-induced hypoglycemia, Fasano CJ, O’Malley, et al. Ann Emerg Med. 2008 Apr;51(4): 400-406.
Octreotide for the treatment of sulfonylurea poisoning. Glatstein M. et al. Clin Toxicol 2012;50:795-804.
Category: Toxicology
Keywords: Methylene Blue (PubMed Search)
Posted: 5/17/2018 by Kathy Prybys, MD
(Updated: 5/18/2018)
Click here to contact Kathy Prybys, MD
Methylene Blue is a dye that was synthesized in the late 1800s as an antimalarial drug. After the emergence of chloroquine its use loss favor partly due to unpopular side effects of temporarily turning the urine, other body fluids, and the sclera blue. Methylene blue is primarily known as a highly effective fast acting antidote for methemboglobinemia. Over the past few years, it has become an important therapeutic modality with expanding uses in cardiac surgery and critical care. As a potent inhibitor of nitric oxide mediated guanylate cyclase induced endothelium vascular smooth muscle relaxation, it has been shown to be effective in increasing arterial blood pressure and cardiac function in several clinical states, such as septic shock and calcium channel blocker poisoning.
BOTTOM LINE:
Methylene blue should be considered for treatment of refractory shock from calcium channel and beta blocker poisoning.
Clinical improvement in refractory hypotension and reduction of vasopressor dose has been described in several poisoning cases.
Recommended dose is 1–2 mg/kg injection with effects seen within 1 hour.
Methylene Blue Used in the Treatment of Refractory Shock Resulting From Drug Poisoning. Fisher J, et al. Clin Toxicol 2914 Jan;52:63-65.
Calicum channel antagonist and beta blocker overdose: antidotes and adjunct therapies. Graudins A, et al. British Journal of Clin Pharm. 2016;81(3):453-461.
Category: Toxicology
Keywords: Intralipid Emulsion (PubMed Search)
Posted: 5/3/2018 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Despite initial excitement for the use of intravenous lipid emulsion (ILE) therapy as an antidote for serious poisonings due to lipohphilic drugs there remains an absence of evidence combined with an incomplete understanding of its efficacy, mechanisms of action, safety, and analytical interferences to recommend its use except in a few clinical scenarios.
The lipid emulsion workgroup performed a comprehensive analysis of four systematic reviews and based recommendations from consensus of expert panelists from the American Academy of Clinical Toxicology, the European Association of Poison Centres and Clinical Toxicologists, the American College of Medical Toxicology, the Asia Pacific Association of Medical Toxicology, the American Association of Poison Control Centers, and the Canadian Association of Poison Control Centers. Toxins evaluated had to have a minimum of three human cases reported in the literature.They concluded that ILE could be indicated for the following clinical situations:
The Bottom Line:
The use of Intravenous Lipid Emulsion in severe poisoning is recommended only for a few poisoning scenarios and was based on very low quality of evidence, and consideration of risks and benefits, adverse effects, laboratory interferences as well as related costs and resources.
Evidence-based recommendations on the use of intravenous lipid emulsion therapy in poisoning. Goseslin S. Hoegeberg L, Hoffman R, et al. Clinical Toxicology, 54:10, 899-923.
What are the adverse effects associated with the combined use of intravenous lipid emulsion therapy and extracorporeal membrane oxygenation in the poisoned patient? Hwee MD, Lee RH, et al. Clinical Toxicology, 53:3, 145-150.
Intravenous Lipid Emulsion Therapy and VA-ECMO rescue therapy for Massive Venlafaxine and Clonazepam Overdose. Thomas A, Ovakim D, et al. J Clin Toxicol 2017 7: 368.
Category: Toxicology
Posted: 4/19/2018 by Kathy Prybys, MD
(Updated: 4/20/2018)
Click here to contact Kathy Prybys, MD
Bradycardias caused by poisoning are due to the toxin's effects on cardiovascular receptors and cellular channels and transport mechanisms and are often refractory to standard ACLS drugs. The most common drug classes responsible for bradycardias are calcium channel and beta blockers and digoxin (cardiac glycosides). Sodium channel blockers, clonidine, and opiates also can cause bradycardias. Antidotes are as follows:
** ILE is recommended only in life threatening poisonings where other accepted therapies have been use first or in cardiac arrest clinical scenarios.
Toxic Bradycardias in the Critically Ill Poisoned Patient. Givens M. Emergency Medicine International. Vol 2012.
The safety of high-dose insulin euglycaemia therapy in toxin-induced cardiac toxicity.Page CB, Ryan NM, et al. Clin Toxicol. 2017 Oct 26:1-6
Category: Toxicology
Keywords: QTc, Dysrhythmias, drug overdose (PubMed Search)
Posted: 3/1/2018 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
A leading cause of cardiac arrest in patients 40 years and younger is due to drug poisoning. Adverse cardiovascular events (ACVE) such as myocardial injury (by biomarker or ECG), shock (hypotension or hypoperfusion requiring vasopressors), ventricular dysrhythmias (ventricular tachycardia/fibrillation, torsade de pointes), and cardiac arrest (loss of pulse requiring CPR) are responsible for the largest proportion of morbidity and mortality overdose emergencies. Clinical predictors of adverse cardiovascular events in drug overdose in recent studies include:
Bottom line:
Obtain ECG and perform continuous telemetry monitoring in overdose patients with above risk factors. Patients with two or more risk factors have extremely high risk of in-hospital adverse cardiovascular events and intensive care setting should be considered.
Clinical risk factors for in-hospital adverse cardiovascular events after acute drug overdose. Manini AF, Hoffman RS, et al. Acad Emerg Med. 2015:22(5):499-507.
Incidence of adverse cardiovascular events in adults following drug overdose. Manini AF, Nelson LS, et al. Acad Emerg Med. 2012;19:843–9.
Category: Toxicology
Keywords: Cardiotoxicity, Bupropion, Ventricular dysrhythmia (PubMed Search)
Posted: 2/15/2018 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Bupropion (Wellbutrin, Zyban) is unique monocyclic antidepressant and smoking cessation agent that is structurally similar to amphetamines. Bupropion blocks dopamine and norepinephrine reuptake and antagonizes acetylcholine at nicotinic receptors.
Bottom line:
Bupropion is a common cause of drug induced seizures but in severe overdose can also cause prolonged QTc and wide complex ventricular dysrhythmia that may be responsive to sodium bicarbonate. All patients with an overdose of bupropion should have an ECG performed and cardiac monitoring to watch for conduction delays and life-threatening arrhythmias.
Wide complex tachycardia after bupropion overdose. Franco V. Am J Emerg Med. 2015 Oct;33 (10):1540.
Delayed bupropion cardiotoxicity associated with elevated serum concentrations of bupropion but not hydroxybupropion. Al-Abri SA, Orengo JP, et al. Clin Tox. 2013 Dec ;51(10):1230-4.
QRS widening and QT prolongation under bupropion: a unique cardiac electrophysiological profile. Caillier B. Pilote S. et al. Fundam Clin Pharmacol. 2012 Oct;26(5): 599-608.
Comparison of Resuscitative Protocols for Bupropion Overdose Using Lipid Emulsion in a Swine Model. Fulton LV, Fabrich RA, et al, Military Medicine 181, 5:482, 2016.
Category: Toxicology
Posted: 2/1/2018 by Kathy Prybys, MD
(Updated: 2/2/2018)
Click here to contact Kathy Prybys, MD
47 year old woman presents with cough, headache, weakness, and low grade fever. Her symptoms have been present for several days. Vital signs are temperature 99.9 F, HR 96, RR 16, BP 140/88, Pulse Ox 98%. Physical exam is nonfocal. She is Influenza negative. She is treated with Ibuprofen and oral fluids. Upon discharge she mentions she is having difficulty hearing and feels dizzy. Upon further questioning she admits to ringing in her ears. What tests should you order?
ANSWER: Salicylate and Acetaminophen levels.
Patient admits to taking BC Powder, an over the counter medication to self treat over the past few days. The active ingredients of BC powder are 845 mg of aspirin and 65 mg of caffeine. Her salicylate level is 45 mg/dL. Her other labs are unremarkable. Serial salicylate levels should be obtained every 2-4 hours and correlated with blood pH and clinical findings.
Salicylates commonly cause of ototoxicity. Tinnitus and hearing loss are early signs of salicylate toxicity and occur between 20-45 mg/dL. Other CNS effects are vertigo, hyperventilation, delirium, seizure, lethargy, and coma. Salicylate and acetaminophen are contained in numerous over the counter medications and are often mistakenly considered safe by the public resulting in accidental overdose. Early signs of toxicity can be missed or confused with other illness with serious consequences.
American College of Medical Toxicology. Guidance Document: Management Priorities in Salicylate Toxicity. J Med Tox. 2015;11(1):149-152.
Emergency department management of the salicylate-poisoned patient. O'Malley GF. Emerg Med Clin North Am. 2007 May ;25(2):333-46.
Category: Toxicology
Keywords: Liver dialysis, MARS (PubMed Search)
Posted: 1/18/2018 by Kathy Prybys, MD
(Updated: 1/19/2018)
Click here to contact Kathy Prybys, MD
Acute liver failure carries a high morbidity without liver transplantation. Liver support systems can act as “bridge” until an organ becomes available for the transplant procedure or until the liver recovers from injury. Artificial liver support systems temporally provide liver detoxification utilizing albumin as scavenger molecule to clear the toxins without providing synthetic functions of the liver (coagulation factors). One of the most widely used devices is the Molecular Adsorbent Recirculating System (MARS).This system has 3 different fluid compartments: blood circuit, albumin with charcoal and anion exchange column, and a dialysate circuit that removes protein bound and water soluble toxins with albumin.
Bottom Line
MARS therapy could be a potentially promising life saving treatment for patients with acute poisoning from drugs that have high protein-binding capacity and are metabolized by the liver, especially when concomitment liver failure. Consider consultation and transfer of patients to liver center.
The Molecular Adsorbent Recirculating System (MARS®) in the Intensive Care Unit: A Rescue Therapy for Patients with Hepatic Failure. F Saliba, Critical Care 10.1 (2006): 118.
