Category: Critical Care
Keywords: Ventilator, autoPEEP, asthma, COPD, obstructive lung disease (PubMed Search)
Posted: 10/28/2025 by Zachary Wynne, MD
Click here to contact Zachary Wynne, MD
Bottom line:
If a ventilated patient exhibits at least one of: persistent end expiratory flow, unequal inspiratory and expiratory flow-time areas, or ineffective breath triggers; autoPEEP must be evaluated by performing an end-expiratory hold.
If present, ventilator settings should be changed to maximize exhalation time.
In critically ill patients with obstructive lung disease, intubation and mechanical ventilation is often a last resort as it does not fix the underlying pathology of small airway disease. While many complications can arise, the most feared complication is autoPEEP.
What is autoPEEP?
AutoPEEP is excess air trapping in the lungs because the patient has insufficient time to fully exhale. Patients at highest risk include those with obstructive lung pathology due to their increased resistance (from bronchospasm) and sometimes increased compliance (such as in emphysema).
However, it is possible for any patient to develop autoPEEP depending on the amount of time they have to exhale. As respiratory rate increases, the expiratory time decreases proportionally if inspiratory time is kept constant. Ultimately, autoPEEP can lead to rapidly increasing intrathoracic pressures causing decreased preload leading to hemodynamic instability and potentially cardiac arrest. These elevated pressures also place the patient at significant risk of barotrauma/volutrauma.
How do I find it?
There are several signs on the ventilator waveforms for autoPEEP. Some patients may only exhibit one of the following signs of autoPEEP. They are demonstrated in the attached pictures in various ventilator modes.
Image A. Persistent end expiratory flow on the flow-time curve (middle curve) - demonstrated by the expiratory limb of the flow curve not returning to zero (remains negative)
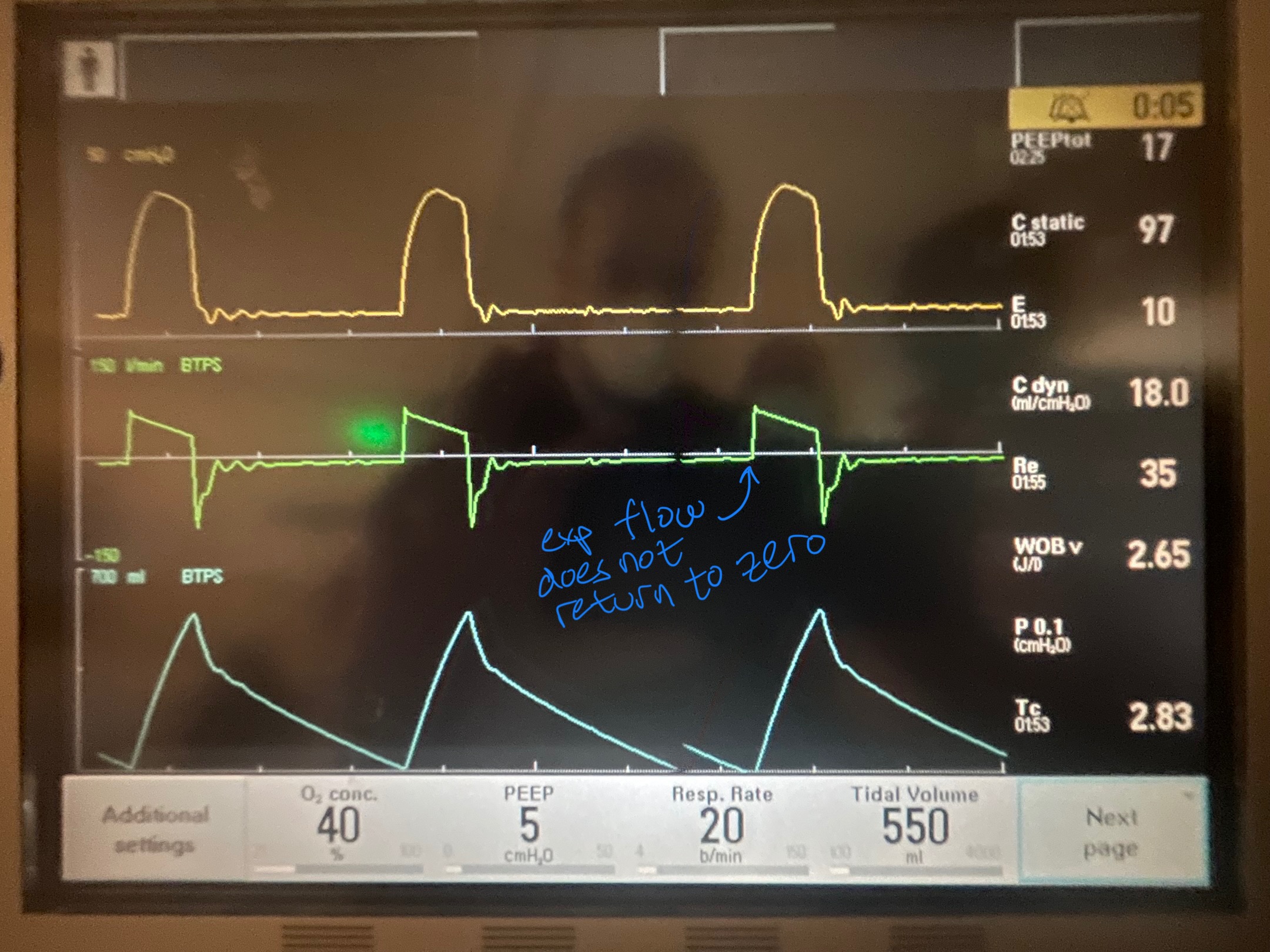
Image B. Unequal inspiratory and expiratory volumes on the flow-time curve (area of flow curve inspiratory limb does not equal area of flow curve expiratory limb)
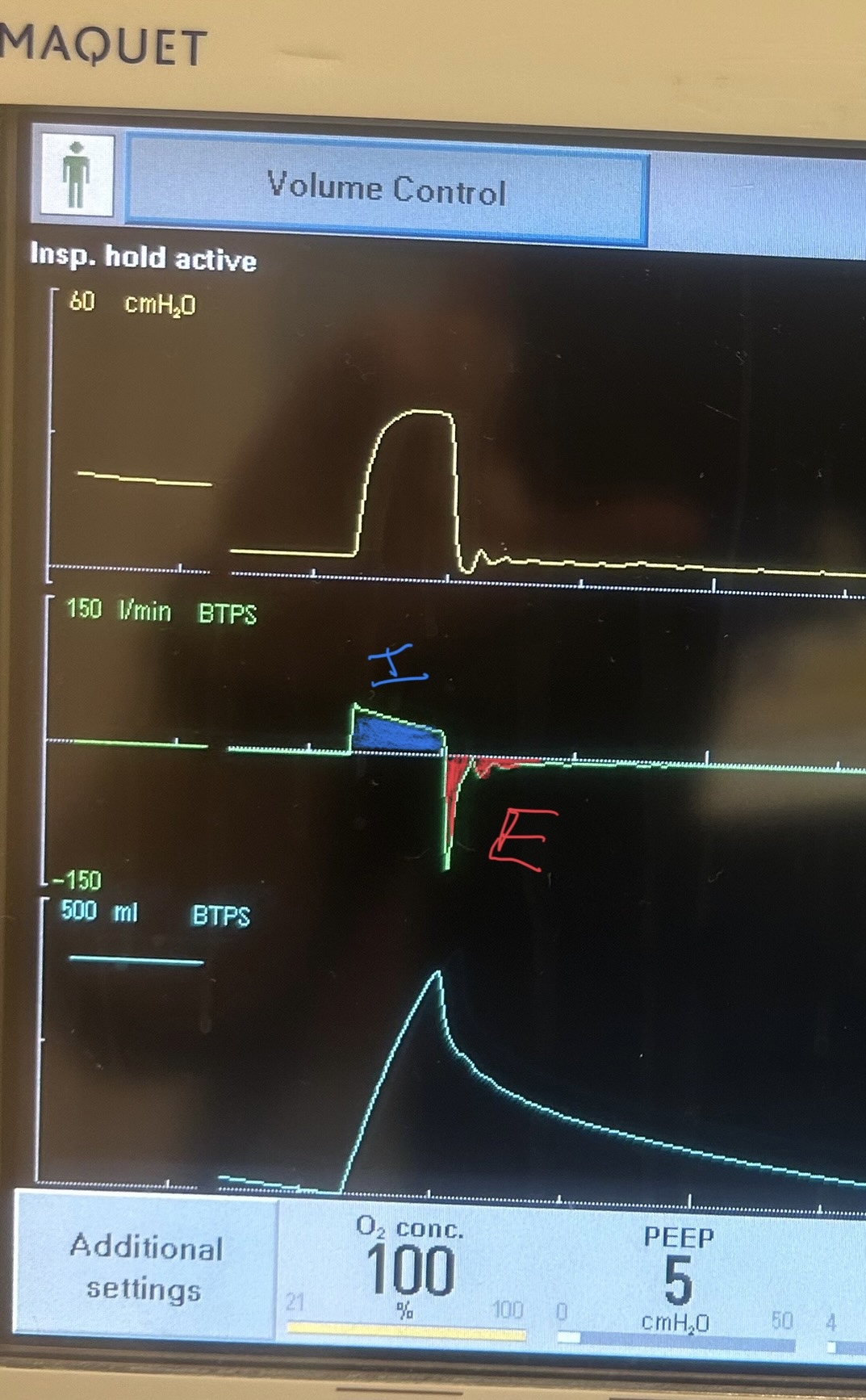
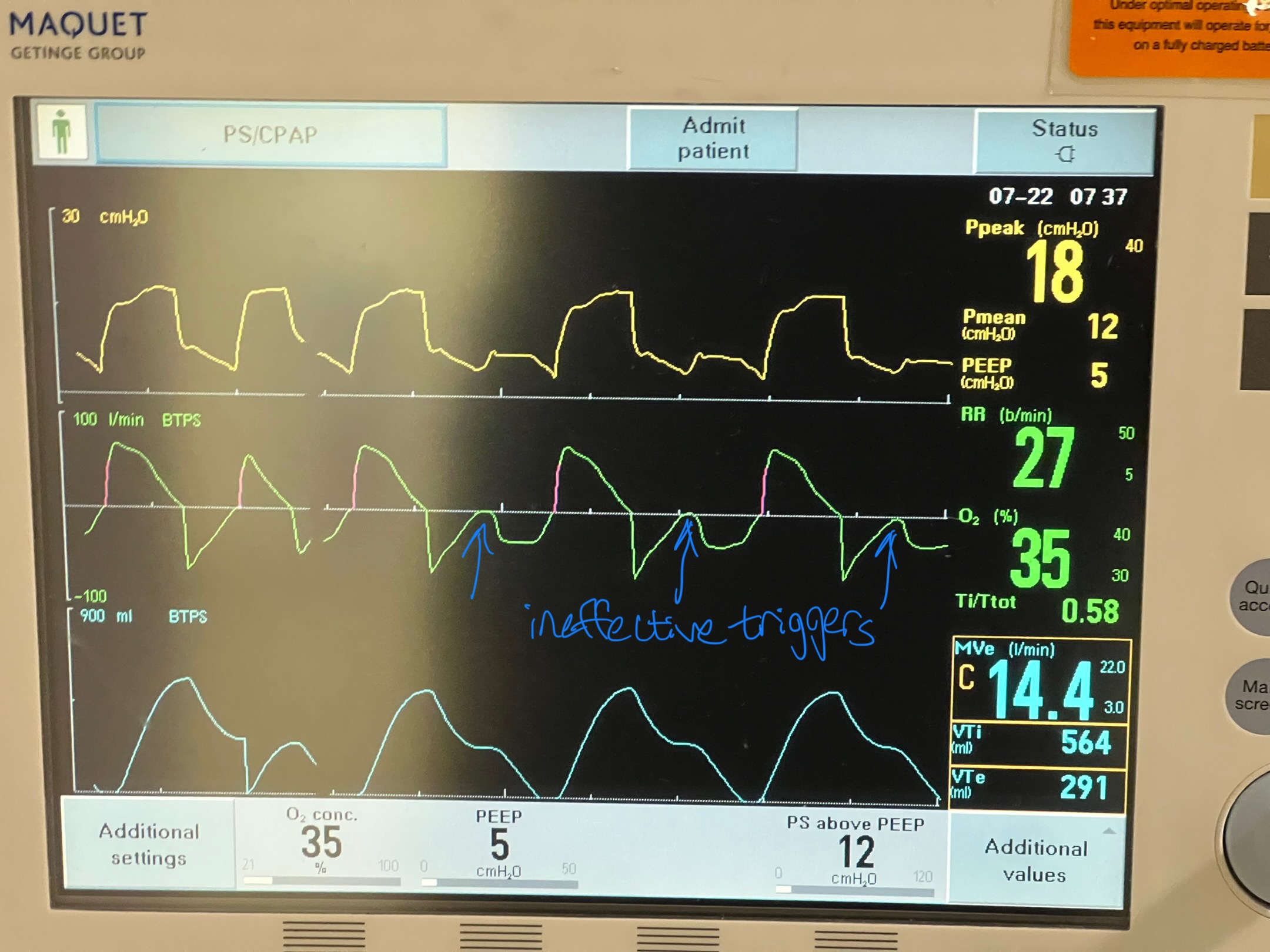
Image C. Ineffective triggering (seen on flow-time curve; patient has to perform more work to reach trigger threshold when autoPEEP is present; they are sometimes unable to trigger a breath)
If any of these are present, an end-expiratory hold maneuver should be performed.
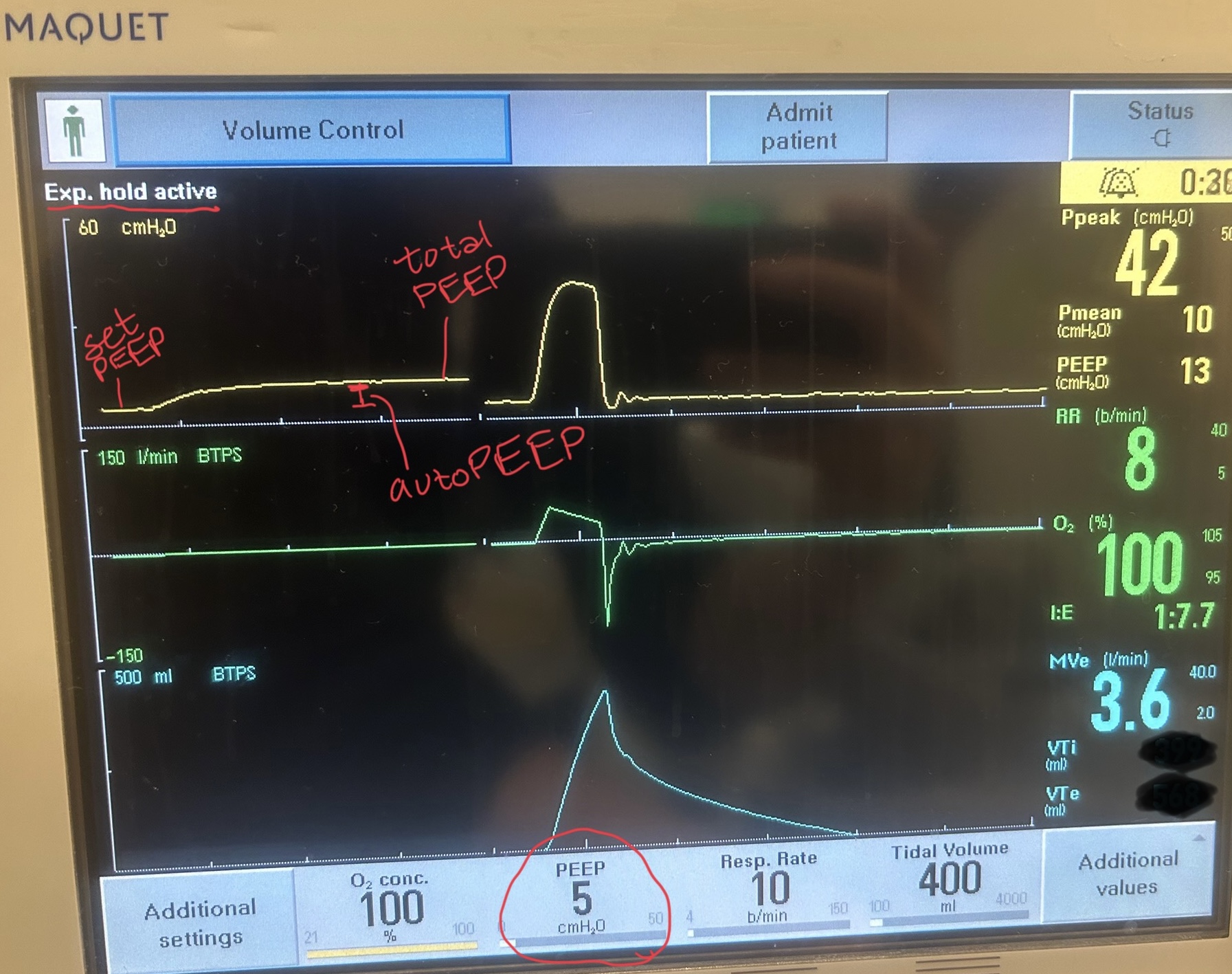
Image D - End-expiratory hold maneuver (done if patient is passive on the ventilator) - the pressure-time curve will begin at ventilator set PEEP and reach total PEEP at the end of the maneuver. The difference between total PEEP and set PEEP is autoPEEP.
If autoPEEP is present, ventilator changes to allow for more exhalation time should be made. The most effective change is by decreasing the respiratory rate though small improvements can be made by changing the inspiratory time and tidal volume. Appropriate bronchodilator therapy, sedation, and treatment of underlying pathology is also critical in these patients.
For more information on autoPEEP, check out this post by Dr. John Greenwood discussing autoPEEP on MarylandCCProject with video demonstrations!
