Category: Critical Care
Keywords: ventilator, extubation, critical care, respiratory, SBT (PubMed Search)
Posted: 12/22/2025 by Zachary Wynne, MD
(Updated: 12/23/2025)
Click here to contact Zachary Wynne, MD
The emergency department serves many critically ill patients that require airway management and mechanical ventilation. Most of these patients go on to require ICU care. However, some patients require only brief intubation and should be appropriate candidates considered for emergency physician-driven extubation. Early extubation can minimize the risks associated with mechanical ventilation for patients such as ventilator associated pneumonia (VAP), ventilator induced lung injury (VILI), and others. Additionally, in setting of high levels of ED boarding and limited ICU resources, extubating appropriate candidates in the ED can reduce boarding times and improve patient flow.
Who?
Screening Checklist
Testing
Prepare - depending on institution, may require consultation with the hospital intensivist
Perform - see this video courtesy of Respiratory Skills - LSC on performing extubation
Category: Critical Care
Keywords: Ventilator, autoPEEP, asthma, COPD, obstructive lung disease (PubMed Search)
Posted: 10/28/2025 by Zachary Wynne, MD
Click here to contact Zachary Wynne, MD
Bottom line:
If a ventilated patient exhibits at least one of: persistent end expiratory flow, unequal inspiratory and expiratory flow-time areas, or ineffective breath triggers; autoPEEP must be evaluated by performing an end-expiratory hold.
If present, ventilator settings should be changed to maximize exhalation time.
In critically ill patients with obstructive lung disease, intubation and mechanical ventilation is often a last resort as it does not fix the underlying pathology of small airway disease. While many complications can arise, the most feared complication is autoPEEP.
What is autoPEEP?
AutoPEEP is excess air trapping in the lungs because the patient has insufficient time to fully exhale. Patients at highest risk include those with obstructive lung pathology due to their increased resistance (from bronchospasm) and sometimes increased compliance (such as in emphysema).
However, it is possible for any patient to develop autoPEEP depending on the amount of time they have to exhale. As respiratory rate increases, the expiratory time decreases proportionally if inspiratory time is kept constant. Ultimately, autoPEEP can lead to rapidly increasing intrathoracic pressures causing decreased preload leading to hemodynamic instability and potentially cardiac arrest. These elevated pressures also place the patient at significant risk of barotrauma/volutrauma.
How do I find it?
There are several signs on the ventilator waveforms for autoPEEP. Some patients may only exhibit one of the following signs of autoPEEP. They are demonstrated in the attached pictures in various ventilator modes.
Image A. Persistent end expiratory flow on the flow-time curve (middle curve) - demonstrated by the expiratory limb of the flow curve not returning to zero (remains negative)
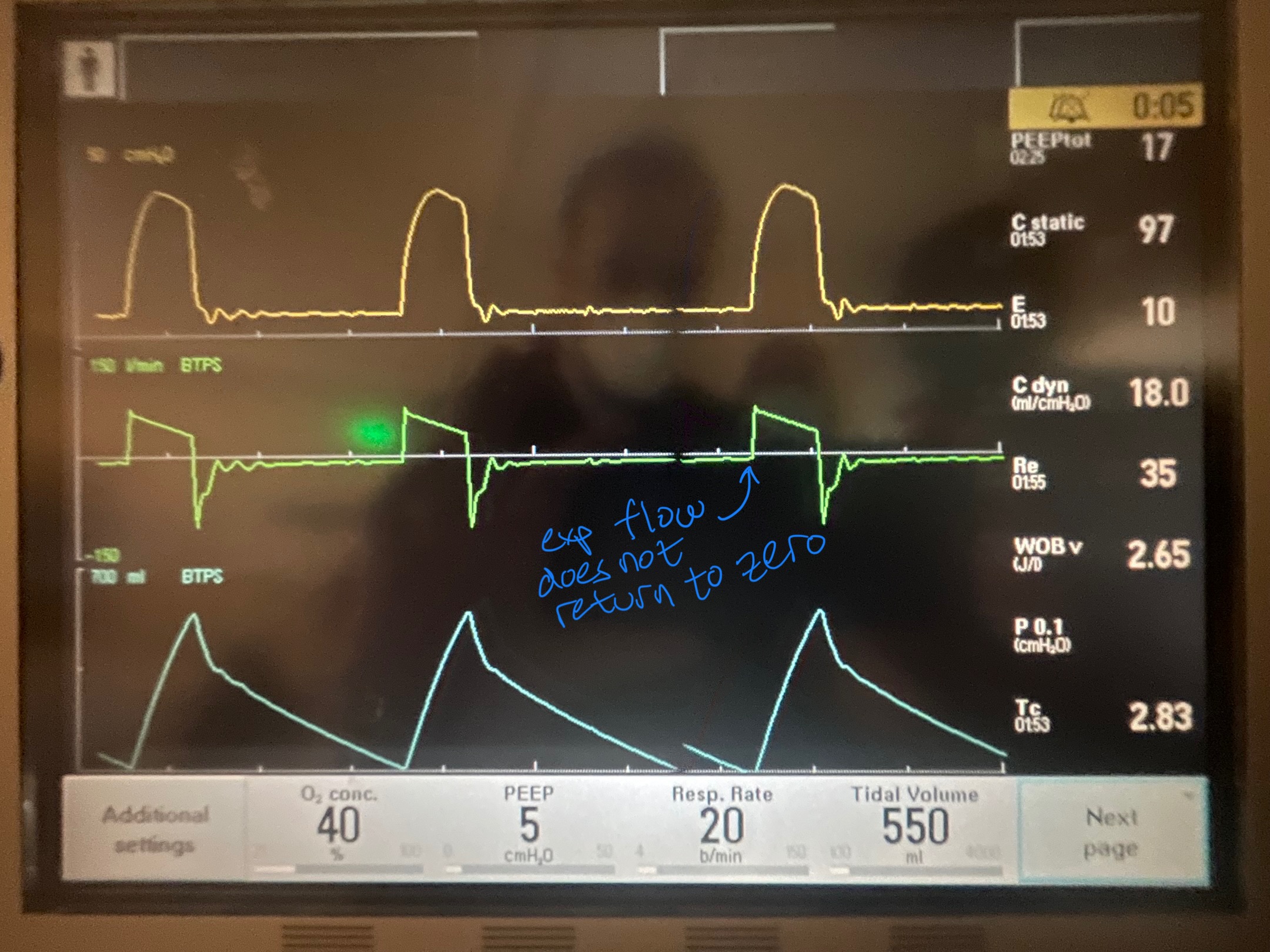
Image B. Unequal inspiratory and expiratory volumes on the flow-time curve (area of flow curve inspiratory limb does not equal area of flow curve expiratory limb)
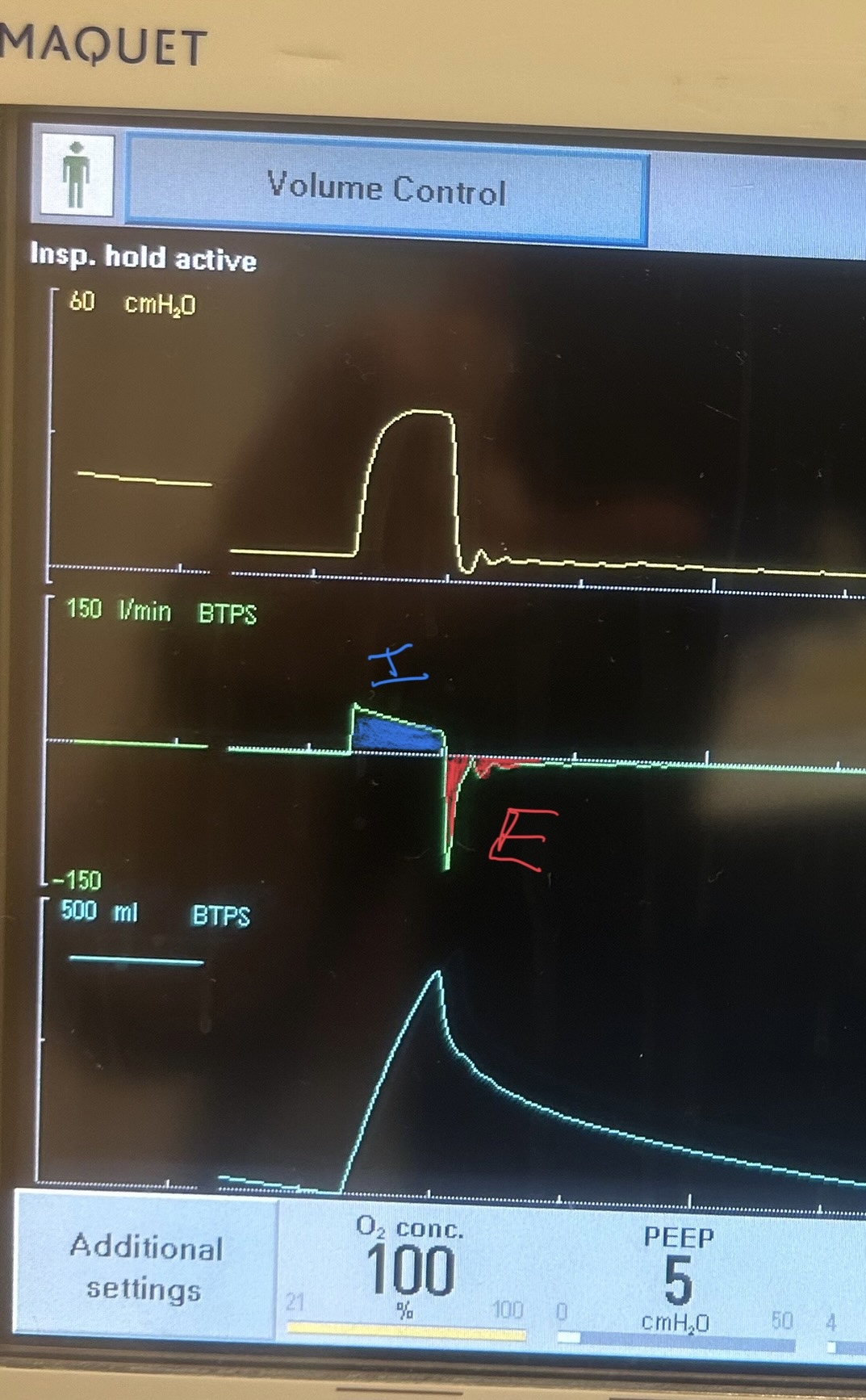
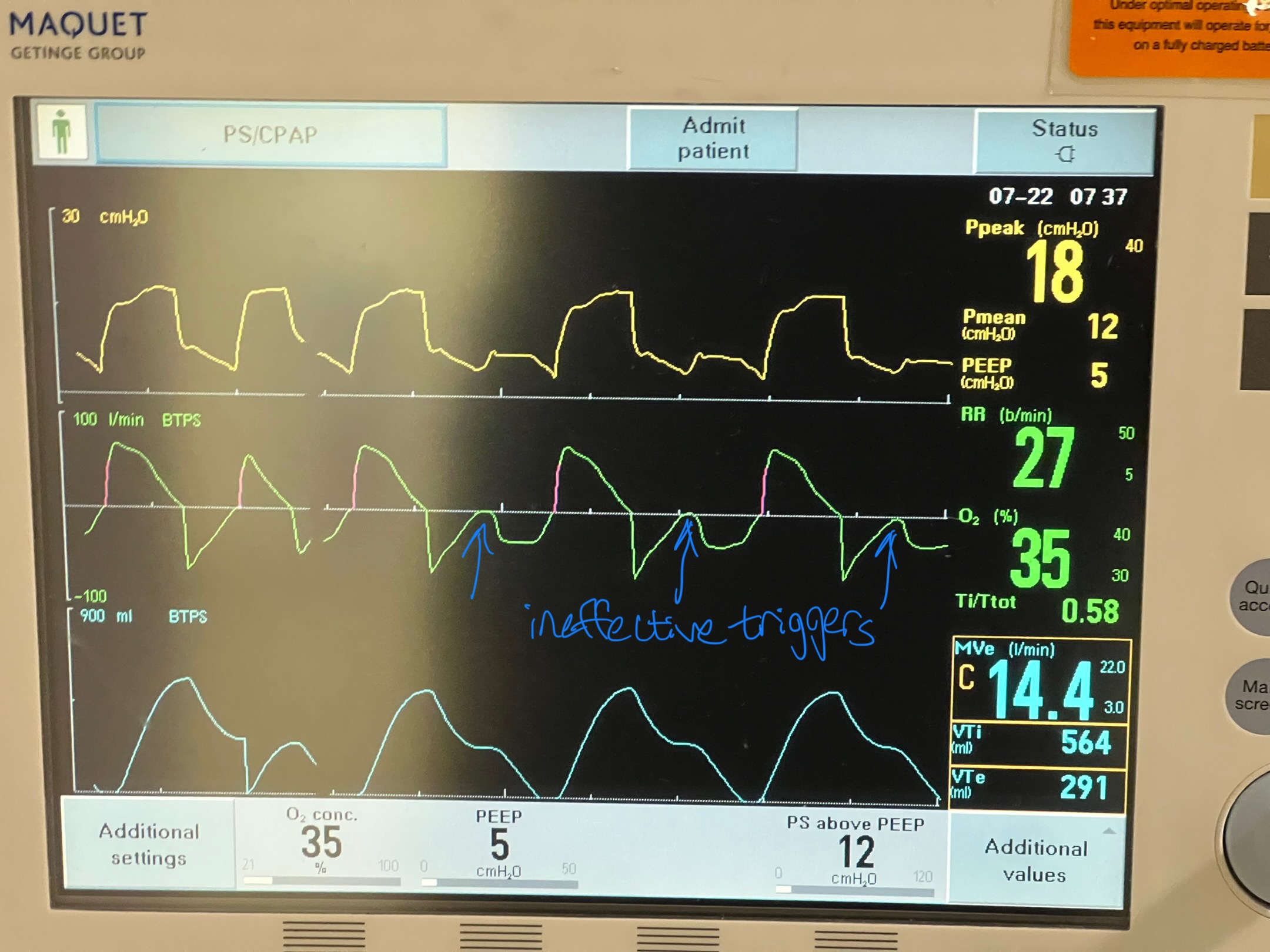
Image C. Ineffective triggering (seen on flow-time curve; patient has to perform more work to reach trigger threshold when autoPEEP is present; they are sometimes unable to trigger a breath)
If any of these are present, an end-expiratory hold maneuver should be performed.
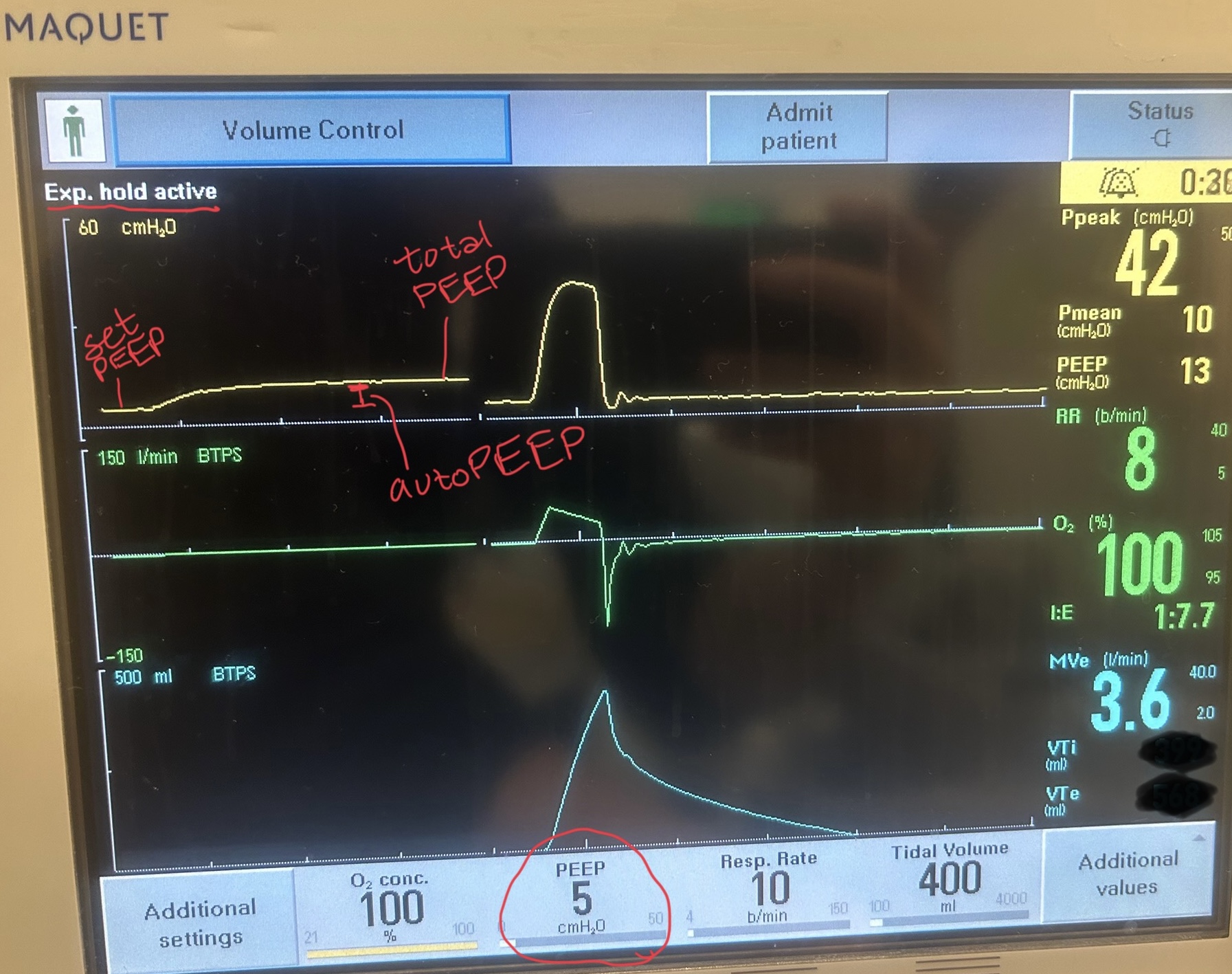
Image D - End-expiratory hold maneuver (done if patient is passive on the ventilator) - the pressure-time curve will begin at ventilator set PEEP and reach total PEEP at the end of the maneuver. The difference between total PEEP and set PEEP is autoPEEP.
If autoPEEP is present, ventilator changes to allow for more exhalation time should be made. The most effective change is by decreasing the respiratory rate though small improvements can be made by changing the inspiratory time and tidal volume. Appropriate bronchodilator therapy, sedation, and treatment of underlying pathology is also critical in these patients.
For more information on autoPEEP, check out this post by Dr. John Greenwood discussing autoPEEP on MarylandCCProject with video demonstrations!
Category: Critical Care
Keywords: Critical Care, oxygen, ventilator, SaO2 (PubMed Search)
Posted: 9/2/2025 by Zachary Wynne, MD
Click here to contact Zachary Wynne, MD
What is the ideal oxygen saturation goal for a mechanically ventilated patient? Literature over the past decade has led away from the perfect 100% oxygen saturation due to its association with worse patient outcomes across many disease states. It is theorized that excess oxygen leads to free radical production causing a lung injury pattern. However, there is no clear guidance for the ideal range of oxygen saturation goals, particularly in the mechanically ventilated patient, despite a meta-analysis and several recent trials.
UK-ROX Trial - JAMA - June 2025
Question: Does an oxygen saturation goal of 88-92% lead to a lower 90-day mortality compared to usual care?
Population: 16,500 mechanically ventilated adult patients in 97 ICU’s across the UK, excluded patients on ECMO
Intervention: Goal oxygen saturation of 88-92%, using the lowest possible FiO2
Control: Usual care, defined as oxygen supplementation at the discretion of the treating physician (no limits set to FiO2 or SaO2)
Outcomes:
Bottom Line:
Ideal oxygenation targets remain elusive. UK-ROX adds to the growing literature of oxygenation targets in mechanically ventilated patients but does not clearly show that lower oxygen saturation targets lead to improved ICU outcomes. In your emergency department ICU boarder, avoid a 100% oxygen saturation to prevent oxygen toxicity associated lung injury and consider an oxygen saturation goal of 90-96% (88-92% if history of COPD).
Martin DS, Gould DW, Shahid T, Doidge JC, Cowden A, Sadique Z, Camsooksai J, Charles WN, Davey M, Francis-Johnson A, Garrett RM, Grocott MPW, Jones J, Lampro L, Mackle DM, O'Driscoll BR, Richards-Belle A, Rostron AJ, Szakmány T, Warren A, Young PJ, Rowan KM, Harrison DA, Mouncey PR; UK-ROX Investigators. Conservative Oxygen Therapy in Mechanically Ventilated Critically Ill Adult Patients: The UK-ROX Randomized Clinical Trial. JAMA. 2025 Aug 5;334(5):398-408. doi: 10.1001/jama.2025.9663. PMID: 40501321; PMCID: PMC12163715.
Category: Critical Care
Keywords: Sedation, propofol, dexmedetomidine, RASS (PubMed Search)
Posted: 7/8/2025 by Zachary Wynne, MD
Click here to contact Zachary Wynne, MD
The presence of an endotracheal tube by itself does not mandate sedation and many patients require no sedatives while intubated in the ICU. However, patients intubated in the emergency department usually require initial sedation while still paralyzed from RSI. Sedation can also help facilitate procedures and imaging in critically ill patients during initial management.
Current literature has found increased mortality and length of ventilator requirement in oversedated ED patients. The target sedation level for the general population remains a goal RASS (Richmond Agitation-Sedation Scale) of 0 to -1. Society of Critical Care Medicine guidelines from early 2025 recommend dexmedetomidine over propofol as the preferred sedative for light sedation and reducing delirium risk in intubated critically ill patients. A recent trial re-examined other clinical outcomes between these two common sedative agents.
A2B Randomized Clinical Trial - JAMA 2025
Clinical Question: Does alpha 2 adrenergic receptor agonist sedation (dexmedetomidine or clonidine) reduce duration of mechanical ventilation in mechanically ventilated patients compared to a propofol based regimen (usual care)?
Where: 41 UK ICU’s from December 2018 to October 2023
Who: 1438 adults receiving mechanical ventilation for less than 48 hours, receiving propofol and opioid for sedation/analgesia, expected to require mechanical ventilation for greater than 48 hours
Intervention: protocol driven sedation to reach a RASS score of -2 to +1 (either dexmedetomidine, clonidine, or propofol). Of note, propofol could be added to achieve deeper sedation goal if deemed necessary by care team.
Outcomes:
Bottom Line:
While either dexmedetomidine or propofol, with appropriate use of opiates for pain management, are appropriate agents in non-paralyzed mechanically-ventilated patients, propofol may be a more appropriate choice in patients with greater agitation while boarding in the emergency department. However, close attention is needed to avoid the overly deep analgosedation associated with increased mortality. Maintain a goal RASS of 0 to -1 with frequent re-evaluation of your ICU boarders.
Walsh TS, Parker RA, Aitken LM, McKenzie CA, Emerson L, Boyd J, Macdonald A, Beveridge G, Giddings A, Hope D, Irvine S, Tuck S, Lone NI, Kydonaki K, Norrie J, Brealey D, Antcliffe D, Reay M, Williams A, Bewley J, Creagh-Brown B, McAuley DF, Dark P, Wise MP, Gordon AC, Perkins GD, Reade MC, Blackwood B, MacLullich A, Glen R, Page VJ, Weir CJ; A2B Trial Investigators. Dexmedetomidine- or Clonidine-Based Sedation Compared With Propofol in Critically Ill Patients: The A2B Randomized Clinical Trial. JAMA. 2025 Jul 1;334(1):32-45. doi: 10.1001/jama.2025.7200. PMID: 40388916; PMCID: PMC12090071.
Lewis K, Balas MC, Stollings JL, et al. A focused update to the clinical practice guideline for the prevention and management of pain, anxiety, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2025 Mar 1;53(3):e711-e727.
Stephens RJ, Ablordeppey E, Drewry AM, Palmer C, Wessman BT, Mohr NM, Roberts BW, Liang SY, Kollef MH, Fuller BM. Analgosedation Practices and the Impact of Sedation Depth on Clinical Outcomes Among Patients Requiring Mechanical Ventilation in the ED: A Cohort Study. Chest. 2017 Nov;152(5):963-971. doi: 10.1016/j.chest.2017.05.041. Epub 2017 Jun 21. PMID: 28645462; PMCID: PMC5812748.
