Category: Neurology
Keywords: Image, CT scan, head trauma (PubMed Search)
Posted: 1/10/2011 by Rob Rogers, MD
Click here to contact Rob Rogers, MD
FILE RESEND. This was tested via email and will hopefully work. I apologize for errors - Dlemkin (webmaster)
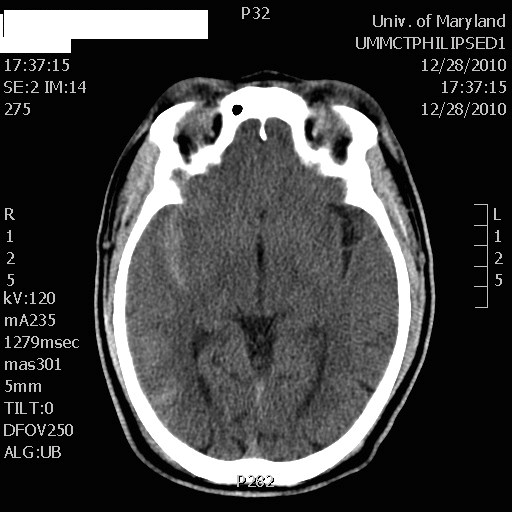
What is the diagnosis? (DON'T LOOK DOWN AT THE ANSWER)
50 year-old male prisoner s/p assault, + LOC
CT shows right-sided traumatic subarachnoid hemorrhage
Category: Neurology
Keywords: nihss, nih stroke scale, posterior stroke, anterior stroke (PubMed Search)
Posted: 1/5/2011 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: seizure, seizure disorder, felbamate, antiepileptics (PubMed Search)
Posted: 12/29/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: lacunar infarct, stroke (PubMed Search)
Posted: 12/22/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: MS, multiple sclerosis, lhermitte's phenomenon, sensory symptom (PubMed Search)
Posted: 12/15/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: transverse myelitis, spinal cord, demyelinating, neurologic condition (PubMed Search)
Posted: 12/8/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: MS, multiple sclerosis, oligoclonal banding, brain MRI, ovoid plaques (PubMed Search)
Posted: 12/1/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: vertigo, cerebellar stroke, stroke, dizziness (PubMed Search)
Posted: 11/24/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: pseudotumor cerebri, idiopathic intracranial hypertension, headache, lumbar puncture (PubMed Search)
Posted: 11/17/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
-- CSF reforms within 6 hours, making its removal short-term, unless there is a CSF leak.
-- LP can be challenging in obese patients and uncomfortable for patients, in general.
-- LP complications such as low pressure headaches, CSF leak, CSF infection, and intraspinal epidermoid tumors.
Category: Neurology
Keywords: movement disorders, chorea, athetosis, fasiculations, dystonia (PubMed Search)
Posted: 11/10/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: sah, subarachnoid hemorrhage, hunt and hess scale, intracranial hemorrhage (PubMed Search)
Posted: 11/3/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Optimal management of subarachnoid hemorrhage requires prognostic understanding and effective communication with neurology and neurosurgical consultants, as well as the patient and their family members.
It is therefore often helpful to utilize and reference the widely recognized Hunt and Hess Scale in grading symptoms of ruptured cerebral aneurysm and subarachnoid hemorrhage severity:
For your convenience, an online Hunt and Hess Scale calculating tool can be found at:
http://www.mdcalc.com/hunt-and-hess-classification-of-subarachnoid-hemorrhage-sah
The following historical references retrieved from http://www.strokecenter.org/trials/scales/hunt_hess.html:
Category: Neurology
Keywords: csf, meningitis, lumbar puncture, subarachnoid hemorrhage, herpes simplex encephalitis (PubMed Search)
Posted: 10/28/2010 by Aisha Liferidge, MD
(Updated: 10/30/2010)
Click here to contact Aisha Liferidge, MD
Classic Cerebrospinal Fluid Characteristics
Category: Neurology
Keywords: concussion, traumatic brain injury, minor traumatic brain injury (PubMed Search)
Posted: 10/20/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: stroke, cerebral edema, tPA, hemorrhage, NIHSS (PubMed Search)
Posted: 10/13/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
--- High NIH Stroke Scale scores.
--- Large areas of infarct.
--- Cerebellar infarcts.
--- Extended time to tPA administration.
--- Previous stroke.
--- Older age.
Category: Neurology
Keywords: diplopia, cranial nerve palsy, monocular diplopia, binocular diplopia (PubMed Search)
Posted: 10/6/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: chlorhexidine, arachnoiditis, lumbar puncture, neurotoxicity (PubMed Search)
Posted: 8/27/2010 by Dan Lemkin, MS, MD
(Updated: 9/29/2010)
Click here to contact Dan Lemkin, MS, MD
Chlorhexidine (CHG) has rapidly become the antiseptic of choice for most skin preparation prior to any percutaneous procedures including:
The Chlorprep(R) label notes: "DO NOT USE FOR LUMBAR PUNCTURE OR IN CONTACT WITH THE MENINGES" (attached)
Authors of the British Royal College of Anaesthetists 3rd National Audit Project provided some guidance for the use of chlorhexidine for spinal procedures
Further: Correspondance from the Journal of Regional Anesthesia and Pain Medicine
"Dr. David Hepner published a correspondence in the April 2007 issue of Anesthesiology that stated the expert panel for Regional Anesthesia and Pain Medicine “felt strongly that although the US Food and Drug Administration has not approved chlorhexidine before lumbar puncture, it has a significant advantage over povidone iodine because of its onset, efficacy, and potency” and commented that “interestingly, povidone iodine is also not approved for lumbar puncture."
Chlorhexidine off-label use is supported in academic literature. Due to specific labeling prohibiting use, a formal institutional policy to support such use may be indicated.
Cook TM, Fischer B, Bogod D, et. al. Antiseptic solutions for central neuraxial blockade: which concentration of chlorhexidine in alcohol should we use? British Journal of Anaesthesia.2009. 103(3):456-457
http://bja.oxfordjournals.org/cgi/content/extract/103/3/456
http://www.apsf.org/newsletters/html/2008/fall/02_ltrchlorprep.htm
http://www.apsf.org/newsletters/html/2008/fall/10_fdaquest.htm
Category: Neurology
Keywords: ulnar nerve, median nerve, radial nerve (PubMed Search)
Posted: 9/22/2010 by Aisha Liferidge, MD
(Updated: 2/22/2011)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: radial nerve palsy, saturday night palsy, honeymoon palsy, wrist drop (PubMed Search)
Posted: 9/15/2010 by Aisha Liferidge, MD
(Updated: 9/18/2010)
Click here to contact Aisha Liferidge, MD
Category: Neurology
Keywords: median nerve block, nerve blok, median nerve (PubMed Search)
Posted: 9/8/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
How to Perform a Median Nerve Block
Category: Neurology
Keywords: ulnar nerve block, ulnar nerve, nerve block (PubMed Search)
Posted: 9/1/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
