Category: Pediatrics
Posted: 12/4/2020 by Cathya Olivas Michels, MD
(Updated: 2/8/2026)
Click here to contact Cathya Olivas Michels, MD
Several studies have described factors associated with peri-intubation cardiac arrest in the adult population. Factors such as pre-intubation hypotension, elevated BMI, and elevated shock index (HR/SBP) have been associated with cardiac arrest following intubation in adult ED patients. Given the differences in anatomy and physiology in children, one may expect risk factors for peri-intubation cardiac arrest to differ in children.
A number of studies have examined factors associated with peri-intubation cardiac arrest in the pediatric population, but these have remained limited to the inpatient setting. These studies have found that, in hospitalized and PICU patients, the factors of hemodynamic instability, hypoxemia, history of difficult airway, pre-existing cardiac disease, and higher number of intubation attempts are associated with peri-intubation cardiac arrest. A paucity of literature exists on this airway complication in pediatric ED patients.
Pokrajac et al. provide the first study on risk factors for peri-intubation cardiac arrest in pediatric ED patients. These authors conducted a retrospective nested case-control study of pediatric patients (ages <18 years) who presented to a tertiary children’s hospital in San Diego from 2009-2017. Cases included patients who had a cardiac arrest within 20 minutes after the start of endotracheal intubation. Authors selected a number of predictors to examine, including age-adjusted hemodynamic variables, capillary refill, pulse oximetry, patient characteristics, intubation-related factors, and pre-intubation interventions.
The authors found the following:
- Demographic characteristics:
o Patients with peri-intubation cardiac arrest were significantly younger (<1 year of age), shorter, and more likely to have history of preexisting pulmonary disease.
- Incident characteristics:
o Patients with peri-intubation cardiac arrest were more likely to have:
-Low or unobtainable SBP or DBP
-Delayed capillary refill time
-Low (<92%) or unobtainable pre-intubation SpO2
-More than 1 intubation attempt than controls
-No paralytic or sedative agent prior to intubation
o Patients with peri-intubation cardiac arrest were NOT more likely to have increases in age-adjusted HR or pediatric shock index in comparison to controls.
o The strongest clinical predictor for peri-intubation cardiac arrest was pre-intubation hypoxia or unobtainable SpO2. This fact is supported by children’s increased metabolic rate and thus increased oxygen consumption. This physiologic finding explains the shorter amount of time it takes children to develop acute hypoxia, particularly in the peri-intubation setting.
Bottom line: If planning to intubate a pediatric patient in the ED, keep in mind that pre-intubation systolic or diastolic hypotension, delayed capillary refill time, multiple intubation attempts, and hypoxia in particular may increase the risk for peri-intubation cardiac arrest. Consider providing apneic oxygenation to minimize hypoxemia prior to intubation.
Heffner, A. C., Swords, D. S., Neale, M. N. & Jones, A. E. Incidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation 84, 1500–1504 (2013).
Hill, K. Cardiac Arrests Associated with Tracheal Intubations in PICUs: A Multicenter Cohort Study. The Journal of Emergency Medicine 51, 617–618 (2016).
Kim, W. Y. et al. Factors Associated with the Occurrence of Cardiac Arrest after Emergency Tracheal Intubation in the Emergency Department. PLoS ONE 9, e112779 (2014).
Pokrajac, N. et al. Risk Factors for Peri-intubation Cardiac Arrest in a Pediatric Emergency Department Pediatric Emergency Care Publish Ahead of Print, (2020).
Category: Pediatrics
Keywords: vaginitis, vaginal discharge (PubMed Search)
Posted: 11/20/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
To determine if the child is prepubescent, look for the lack of pubic hair, clitoral size, configuration of the hymen, breast development, and axillary hair growth. A Tanner stage of 1 would be consistent with prepuberty.
The proper positioning for the physical exam will allow the child to be comfortable and the examiner to obtain an adequate view including up to one-third of the vagina.
If the child is small enough, they can lay in the parent’s lap. For a larger child, you can have the parent sit in the bed with the patient or stand near the child’s head. Engage child life if available.
The frog leg position with gentle downward and outward traction of the labia at the 5- and 7-o’clock positions provides the optimal view.
The knee to chest position is helpful when further evaluation is needed.
A rectovaginal exam is useful for evaluation of masses or foreign body only and is not routinely needed. Place the examiner’s little finger in the rectum and the other hand on the abdomen and palpate.
The use of a vaginal speculum is rarely needed in prepubertal children; if it is needed, perform the exam under anesthesia.
McCaskill A, Inabinet CF, Tomlin K, Burgis J. Prepubertal Genital Bleeding: Examination and Differential Diagnosis in Pediatric Female Patients. J Emerg Med. 2018 Oct;55(4):e97-e100. doi: 10.1016/j.jemermed.2018.07.
Loveless M, Myint O. Vulvovaginitis- presentation of more common problems in pediatric and adolescent gynecology. Best Pract Res Clin Obstet Gynaecol. 2018 Apr;48:14-27. doi: 10.1016/j.bpobgyn.2017.08.014. Epub 2017 Sep 5. PMID: 28927766.
Manning S. Genital Complaints at the Extremes of Age. Emerg Med Clin North Am. 2019 May;37(2):193-205. doi: 10.1016/j.emc.2019.01.003. PMID: 30940366.
Category: Pediatrics
Keywords: pain management, ketamine (PubMed Search)
Posted: 11/6/2020 by Prianka Kandhal, MD
Click here to contact Prianka Kandhal, MD
Silva LOJ, Lee JY, Bellolio F, Homme JL, Anderson JL. Intranasal ketamine for acute pain management in children: A systematic review and meta-analysis. American Journal of Emergency Medicine. 2020 (38)1860-1866. doi: 10.1016/j.ajem.2020.05.094
Category: Pediatrics
Posted: 10/31/2020 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
The current COVID-19 pandemic and known aerosolized transmission has triggered many ED process changes, including the discouragement of utilizing nebulizers to administer inhaled bronchodilators such as albuterol for concern of spread. Historically, both patients and providers preferred the use of nebulizers as they are easier to use and the belief was that they were more effective than meterd dose inhalers. However, evidence based data has consistently shown that for both adult and pediatric patients that when MDI's are used WITH a spacer:
Albuterol: 2.5 mg nebulizer solution = 3-5 MDI puffs
Albuterol: 5 mg nebulizer solution = 5-10 MDI puffs
Ipratropium: 0.25 mg nebulizer solution = 2 MDI puffs
Ipratropium: 0.5 mg nebulizer solution = 4 MDI puffs
Category: Pediatrics
Keywords: GU anomaly, prepubescent (PubMed Search)
Posted: 10/16/2020 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
A labial adhesion is defined as a thin avascular clear plane, a raphe, between the labia minora. These adhesions which can be caused by minor trauma or infection in the absence of estrogen can cause varying degrees of obstruction.
Loveless M, Myint O. Vulvovaginitis- presentation of more common problems in pediatric and adolescent gynecology. Best Pract Res Clin Obstet Gynaecol. 2018 Apr;48:14-27. doi: 10.1016/j.bpobgyn.2017.08.014. Epub 2017 Sep 5. PMID: 28927766.
Bacon JL, Romano ME, Quint EH. Clinical Recommendation: Labial Adhesions. J Pediatr Adolesc Gynecol. 2015 Oct;28(5):405-9. doi: 10.1016/j.jpag.2015.04.010. Epub 2015 Apr 24. PMID: 26162697.
Category: Pediatrics
Keywords: uncomplicated appendicitis (PubMed Search)
Posted: 10/1/2020 by Cathya Olivas Michels, MD
Click here to contact Cathya Olivas Michels, MD
Acute appendicitis is the most common etiology requiring urgent abdominal surgery in children in the United States. Peak incidence occurs in the second decade of life, with male patients being more commonly affected than female patients. Classic manifestations of appendicitis occur in school-aged children and adolescents, but are often absent in younger children. Infants and young children <5 years are more likely to present with nonspecific or atypical findings, resulting in delays in diagnosis and higher rates of perforation.
Diagnosis is aided by clinical factors, lab findings, and ultrasound (+/- CT or MRI if ultrasound is equivocal).
Historically, the standard of care for acute appendicitis has been urgent operative management. However, in the past several years, there has been increasing literature supporting nonoperative management (antibiotics only) in adult patients with acute uncomplicated appendicitis. Additionally, there is a growing body of evidence demonstrating the safety and efficacy of nonoperative management for uncomplicated appendicitis in children.
Hartford and Woodward provide a review of the current literature on the nonoperative management of uncomplicated appendicitis in children. They conclude:
- The majority of recent prospective studies demonstrate early treatment success (0-30 days) of approximately 90% in pediatric patients undergoing nonoperative management.
- Factors associated with failure of nonoperative management in pediatric appendicitis: longer duration of symptoms (>48 hours), younger age (<5 years), and presence of appendicolith.
- Nonoperative management has been associated with
o Lower healthcare costs at 1 year
o Fewer disability days at 1 year
o No significantly different rate of complicated appendicitis
- Most trials to date involve a 24-48 hour initial course of broad spectrum IV antibiotics followed by oral antibiotics for a total of >/= 7 days as nonoperative management. Currently, there is no consensus on antibiotic regimen.
Bottom Line: Given the current evidence, nonoperative management may be a viable treatment option for low risk pediatric patients with uncomplicated appendicitis. The literature is not conclusive, thus we as medical providers in conjunction with our surgical colleagues, should consider numerous factors when discussing treatment options for acute appendicitis with patients and their families.
Hartford, E. A. & Woodward, G. A. Appendectomy or Not? An Update on the Evidence for Antibiotics Only Versus Surgery for the Treatment of Acute Appendicitis in Children. Pediatric Emergency Care 36, 6 (2020).
2.
Minneci, P. C. et al. Association of Nonoperative Management Using Antibiotic Therapy vs Laparoscopic Appendectomy With Treatment Success and Disability Days in Children With Uncomplicated Appendicitis. JAMA 324, 581 (2020).
3.
Minneci, P. C. et al. Effectiveness of Patient Choice in Nonoperative vs Surgical Management of Pediatric Uncomplicated Acute Appendicitis. JAMA Surg 151, 408 (2016).
Category: Pediatrics
Keywords: prepubertal vaginal bleeding, mass (PubMed Search)
Posted: 9/18/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
- Urethral prolapse will appear as a protrusion of the distal urethra through the urinary meatus causing a “doughnut” sign.
- Risk factors include trauma, UTI, anatomical differences, and increased intraabdoiminal pressure from cough or constipation. There is a higher incidence in people of African descent.
- The chief complaint may include urethral mass and vaginal bleeding.
- There is a bimodal age distribution (prepuberty and postmetapause) due to a relative estrogen deficiency.
-Treatment is with estrogen cream and sitz baths for 4- 6 weeks.
McCaskill A, Inabinet C, Tomlin K et al. Prepubertal Genital Bleeding: Examination and Differential Diagnosis in Pediatric Female Patients. The Journal of Emergency Medicine 2018; 55(4): 97-100.
Category: Pediatrics
Keywords: button battery, pediatrics, esophageal injuries (PubMed Search)
Posted: 9/4/2020 by Prianka Kandhal, MD
Click here to contact Prianka Kandhal, MD
Ingestion of a button battery is a can't-miss diagnosis with a very high risk for causing severe esophageal injury. There are about 3000 button battery ingestions per year, and this is increasing because electronics are becoming more and more prevalent.
Severe damage to the esophagus occurs within 2 hours. On your lateral view, the end with narrowing is the negative end, which triggers a hydrolysis reaction that results in an alkaline caustic injury and, ultimately, liquefactive necrosis.
Children can present with nonspecific symptoms and if the ingestion was not witnessed, they are at high risk for delays in diagnosis. Additionally, in the community setting, there can be further delays in definitive treatment (endoscopic removal) due to difficulty in calling teams in or transporting to other facilities.
Anfang et al. looked into ways to mitigate damage to esophageal tissue. They did an in vitro study on porcine esophageal tissue, measuring the pH with different substances applied. They tried apple juice, orange juice, gatorade, powerade, pure honey, pure maple syrup, and carafate. They then repeated the study in vivo on piglets with button batteries left in the esophagus and ultimately did gross and histological examination of the esophageal tissue.
Honey and carafate demonstrated protective effects both in vitro and in vivo. They neutralized pH changes, decreased full-thickness esophageal injury, and decreased outward extension of injury into deep muscle.
Take Home Point: If a child is found to have a button battery in the esophagus, while definitive management is still emergent endoscopic removal, early and frequent ingestion of honey (outside of the hospital) and Carafate (in the hospital) may help reduce the damage done to the tissue in the interim. The authors recommend 10ml every 10 minutes.
Anfang RR, Jatana KR, Linn RL, et al. pH-Neutralizing Esophageal Irrigations as a Novel Mitigation Strategy for Button Battery Injury. The Laryngoscope. 2019; 129:49-57.
Category: Pediatrics
Keywords: Female GU, abdominal pain, missed period (PubMed Search)
Posted: 8/21/2020 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Definition: Congenital anomaly where the hymen is completely obstructing the vaginal opening
Demographic: Incidence 0.05-0.1% of females
History: Most are asymptomatic and diagnosed on physical exam or incidentally when there is lack of menarche. Symptoms in adolescents can include: Abdominal pain (50%), urinary retention (20%), abnormal menstruation (14%), dysuria (10%), frequency, renal failure, UTI and back pain.
Physical exam: bulging, blueish hymenal membrane
Complications: Late detection can lead to infections, fertility problems, endometriosis, hydronephrosis, and rarely renal failure
ED treatment: If abdominal pain is significant or there is urinary obstruction, a urinary foley can be placed. GYN should be consulted.
Definitive treatment: Hymenectomy, hymenotomy, carbon dioxide laser treatments or foley insertion through the hymen (done by a specialist).
Lee K, Hong J, Jung H et al. Imperforate Hymen: A Comprehensive Systematic Review. J Clin Med 2019; 8(56): 1-14.
Category: Pediatrics
Keywords: MVC, neck injury, neurological injury (PubMed Search)
Posted: 7/24/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
There is no well validated clinical decision rule similar to NEXUS or the Canadian Cervical Spine rule in children for clearing the cervical spine. Clinical clearance versus imaging first is a complicated decision. Certain risk factors may predispose children to injury and should be taken into account when deciding about clinical clearance versus imaging (XR).
High Risk Criteria for Cervical Spine Injury in Pediatrics
| Mechanism
| High risk MVC Intrusion > 12 inches at the occupant site Intrusion > 18 inches at any site Partial or complete ejection Death in the same passenger compartment Vehicle telemetry consistent with high speed Fall > 10 feet Nonaccidental trauma Diving injury |
| History
| Down’s Syndrome 22.q11.2 deletion Klippel-Fiel syndrome |
| Physical Exam
| Altered mental status Intoxication Hypotension Focal neurological exam Neck pain Torticollis |
Gopinathan N, Viswanathan V, Crawford A. Cervical Spine Evaluation in Pediatric Trauma: A Review and an Update of Current Concepts. Indian J Orthop 2018;52(5):489-500.
Leonard J, Browne L and Ahmed F et al. Cervical Spine Injury Risk Factors in Children with Blunt Trauma. Pediatrics 2019;144 (1):e20183221.
Kliegman R, Stanton B, St Geme J et al. Nelson Textbook of Pediatrics. 20th edition Vol 1 and 2. 2016. Elsevier. P 549-550, 3299-3300, 3352.
Category: Pediatrics
Posted: 7/3/2020 by Cathya Olivas Michels, MD
Click here to contact Cathya Olivas Michels, MD
Every year, numerous children die of non-exertional heatstroke after being left in motor vehicles in the United States. Per data obtained from the national nonprofit KidsAndCars.org, the average number of pediatric vehicular heatstroke deaths is 39 per year since 1990. In 2018, this number peaked at 54 pediatric deaths. Prior studies show that the interior temperature of a closed vehicle rises quickly within minutes of closing the doors and windows. This rapid change occurs even on days with cooler ambient temperatures (20s °C/70s °F): the interior temperature of a car may still reach 117F within an hour.
Children, particularly infants and toddlers, are at increased risk for heat illness due to several physiologic and developmental factors:
- Unable to escape hot environments or to self-hydrate
- Lack mature thermoregulatory systems
o Have lower rate of sweat production than adults
- Have higher basal metabolic rates than adults
- Have higher body surface area:mass ratio --> absorb heat faster in hot environments
Bottom line: ED providers can be instrumental in giving anticipatory guidance on vehicular heatstroke in children during the warmer seasons:
- Educate caregivers to “Look before you Lock”
- Suggest that the caregiver place a valuable object (phone, employee badge, handbag) in the back seat when traveling with a child
- Remind caregiver of the dangers of intentionally leaving a child in the car for any reason, even during cooler spring/summer days.
A recent retrospective cohort study (Hammett et al.) of 554 pediatric victims (aged <14 years) who died of heatstroke in a motor vehicle was conducted using KidsAndCars.org data. This study is the largest to date to describe this US subset of pediatric fatalities.
Results:
- Nearly half of the cases occurred when the ambient temperature was >90°F. However, 10% cases occurred when the ambient temperature was < 80°F.
- Most incident cases (~40%) occurred in home parking areas > nonresidential parking areas> daycare centers parking.
- The mean victim age was 16.4 months. Most (99%) victims were less than 5 years of age.
- Male children were more common victims (54% cases) than female children.
- Most victims (78%) were left unknowingly in vehicles by their caregivers. For those victims left intentionally in vehicles, caregivers’ reasons for leaving the child in the vehicle were the caregivers’ need to attend work or school or desire to allow the child to keep sleeping.
- A single caregiver was most commonly responsible for leaving the child in the vehicle (89% cases), with the victim’s mother being the most often responsible.
https://www.kidsandcars.org/wp-content/uploads/2020/01/Heatstroke-fact-sheet.pdf
Hammett, D. L., Kennedy, T. M., Selbst, S. M., Rollins, A. & Fennell, J. E. Pediatric Heatstroke Fatalities Caused by Being Left in Motor Vehicles. Pediatric Emergency Care, (2020).
Category: Pediatrics
Keywords: weight loss, not eating, small, FTT (PubMed Search)
Posted: 6/19/2020 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Calleo V, Surujdeo R and Thabet A. Emergency Department Management of Patients with Failure to Thrive. EB Medicine. March 2020.
Category: Pediatrics
Posted: 5/29/2020 by Rose Chasm, MD
(Updated: 2/8/2026)
Click here to contact Rose Chasm, MD
Spanish Peditric Academy
AAP News
BMJ 2020;369:m1802
NEJM 2020; 382:1663-1665
Category: Pediatrics
Keywords: seat belt, car seats (PubMed Search)
Posted: 5/15/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
NHTSA recommends that car seats be replaced following a moderate or severe crash. Car seats do not automatically need to be replaced following a minor crash.
A minor crash is one in which ALL of the following apply:
-The vehicle was able to be driven away from the crash site.
-The vehicle door nearest the car seat was not damaged.
-None of the passengers in the vehicle sustained any injuries in the crash.
-If the vehicle has air bags, the air bags did not deploy during the crash
-There is no visible damage to the car seat.
NEVER use a car seat that has been involved in a moderate to severe crash. Always follow manufacturer's instructions.
Car Seat Use After a Crash. https://www.nhtsa.gov/car-
Category: Pediatrics
Keywords: MVC, anticipatory guidance, seatbelts. (PubMed Search)
Posted: 4/17/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
The leading cause of death in the US for those aged 16 to 24 years is motor vehicle collisions (MVCs). Teen drivers are more likely than any other age group to be involved in an MVC that result in injury or fatality. Texting while driving, nighttime driving, inexperienced driving, and driving under the influence of alcohol or drugs may play a role in these collisions.
Can anticipatory guidance related to safe driving be done in the ED? YES!
This study implemented a toolkit that contained a copy of the driving law, a sample parent-teen driving contract and statistics on teen driving injuries. Post toolkit questionnaires showed that both teens and their guardians learned new information.
Bottom line: Engage in anticipatory guidance in the ED with teens and their parents about seatbelt use, the dangers of driving under the influence and local driving laws.
Spears et al. Teen driving education in the pediatric emergency department: effectiveness of a tool kit. Southern Medical Journal 2019; 112(11): 562-565.
Category: Pediatrics
Keywords: pandemic, coronavirus, pediatric (PubMed Search)
Posted: 3/20/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Category: Pediatrics
Keywords: cardiac arrest, prehospital, epinephrine (PubMed Search)
Posted: 2/21/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Matsuyama et al. Pre-Hospital Administration of Epinephrine in Pediatric Patients with Out-of-Hospital Cardiac Arrests. JACC: 75 (2); 2020.
Category: Pediatrics
Keywords: avulsion fracture, orthopedics, pelvic injury, trauma (PubMed Search)
Posted: 2/14/2020 by Mimi Lu, MD
(Updated: 2/15/2020)
Click here to contact Mimi Lu, MD
A 15 y.o. female presents to your emergency department with sudden onset hip pain after winding up to kick a soccer ball during her game today. You see a well-developed female in obvious discomfort, with tenderness to palpation over her lateral hip and pain with passive ROM at the hip. You obtain this x-ray. What is your diagnosis?
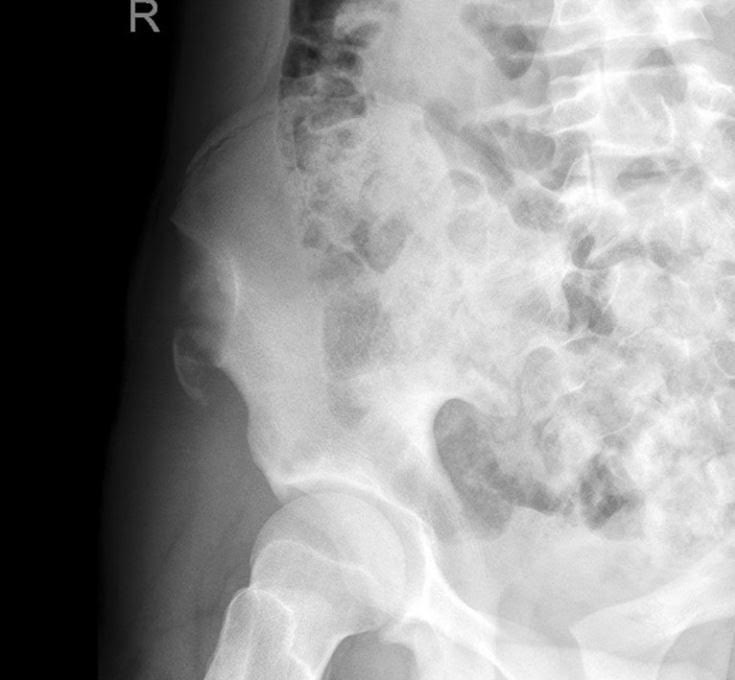
Answer: Avulsion fracture of the anterior superior iliac spine.
Injury:
An avulsion fracture of the anterior superior iliac spine is an uncommon injury seen almost exclusively in adolescent athletes.
They mostly result from a sudden, forceful, and/or unbalanced contraction of the attached musculotendinous unit (sartorius muscle or tensor fascia lata) during the starting phase of running, jumping, kicking, etc.
The most implicated sports include soccer, running, and ice hockey.
History/Exam:
The patient may report sudden shooting pain referred to the involved tuberosity.
Physical exam may include localized edema and tenderness to palpation and pain on passive ROM at the hip.
Anatomy:
The iliac crest is the weakest component of the pelvic ring during adolescence.
The avulsed fragment is usually displaced distally and laterally.
Treatment:
Conservative therapy includes 2-3 weeks of limited activity and walking with partial weight bearing restrictions and crutches. May also include bed rest with the affected lower extremity positioned with the hip and knee in flexion to ensure minimal tension of the muscles attaching to the ASIS. This is considered for minimally displaced fractures in younger children.
Surgical management generally consists of ORIF with a lag screw, and is generally recommended for patients with fracture fragments > 3cm or severely displaced fragments that cause compression of the lateral cutaneous nerve resulting in meralgia parasthetica.
Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30(3):127-31.
Kautzner J, Trc T, Havlas V. Comparison of conservative against surgical treatment of anterior-superior iliac spine avulsion fractures in children and adolescents. Int Orthop. 2014;38(7):1495-8.
Category: Pediatrics
Keywords: ENT, post tonsillectomy bleeding, T and A (PubMed Search)
Posted: 1/17/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Tonsillectomy and adenoidectomy (T&A) is the second most common ambulatory surgery performed in the US. Children younger than 3 years, children with craniofacial disorders or sleep apnea are typically admitted overnight as studies have shown an increase rate of airway or respiratory complications in this population.
The most common late complications include bleeding and dehydration. Other complications include nausea, respiratory issues and pain.
Post-operatively, the overall 30-day emergency department return rate is up to 13.3%. Children ages 2 and younger were more likely to present to the ED. There is significantly higher risk of dehydration for children under 4 years. Children over the age of 6 had significantly higher bleeding risk and need for reoperation for hemorrhage control.
Lindquist NR, Feng Z and Mukerji SS. Age-related causes of emergency department visits after pediatric adenotonsillectomy at a tertiary pediatric referral center. International Journal of Pediatric Otorhinolaryngology 2019; 127: 109668.
Category: Pediatrics
Keywords: Urinary retention, formulas (PubMed Search)
Posted: 12/20/2019 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Urinary retention in pediatrics is defined as the inability to void for more than 12 hours in the presence of a palpable bladder or a urine volume greater than expected for age.
Maximum urine volume calculation for age: (age in years + 2) x 30ml.
Causes of urinary retention include mechanical obstruction, infection, fecal impaction, neurological disorders, gynecological disorders and behavioral problems.
The distribution is bimodal occurring between 3 and 5 years and 10 to 13 years.
Nevo A, Mano R, Livne P, Sivan B and Ben-Meir. Urinary Retention in Children. Urology 2014; 84(6):1475-1479.
