Category: Critical Care
Posted: 10/9/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
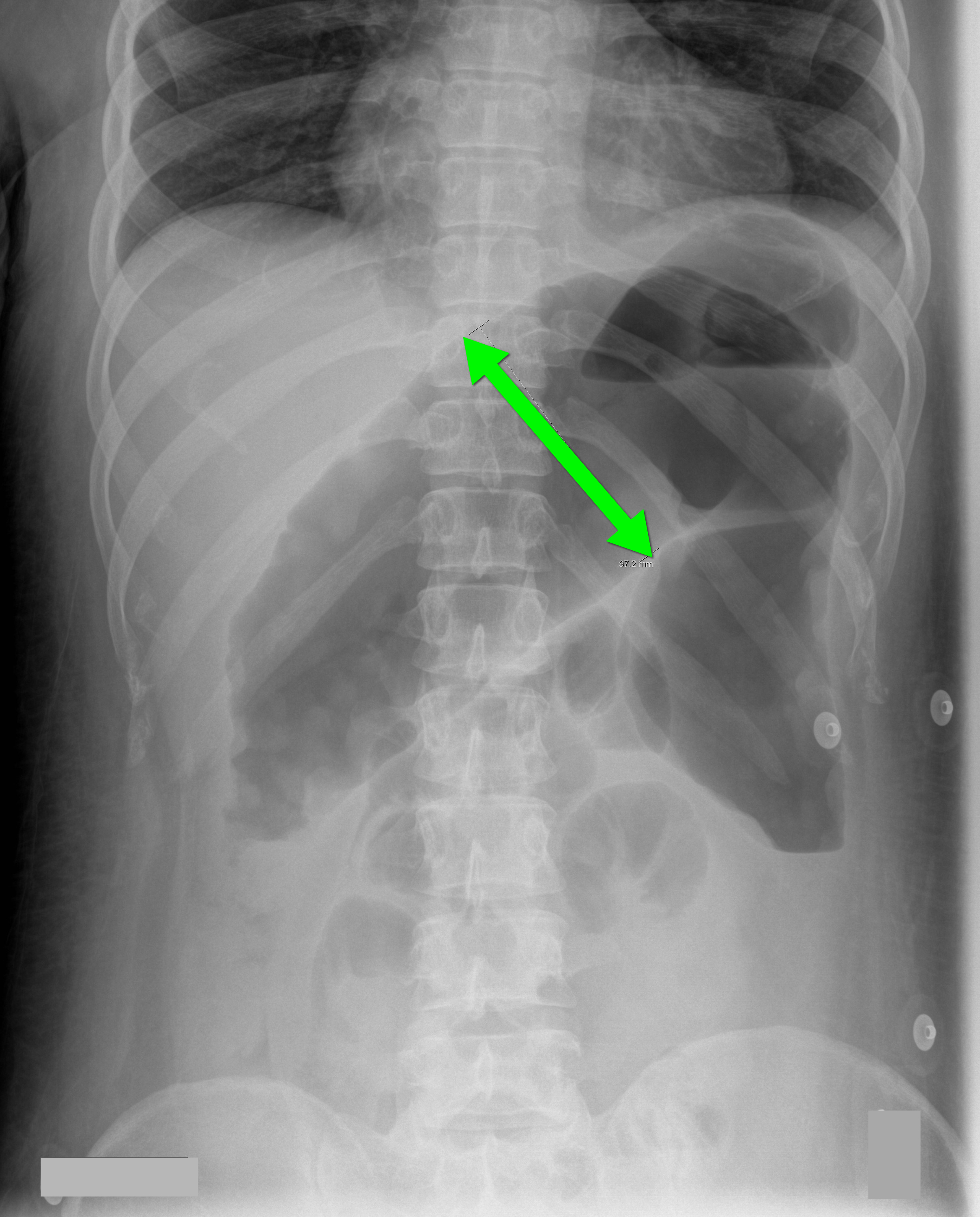
70 year-old male recently treated for community-acquired pneumonia presents with bloody diarrhea, fever, and severe abdominal pain. Abdominal Xray is shown below. Diagnosis?

Answer: Toxic Megacolon
Toxic megacolon (TM) is an acute colitis with segmental or total colonic dilation (>6cm) plus systemic toxicity.
Actual incidence is unknown, but it is believed that TM is rising because of increasing cases of Clostridium difficile and the aging population.
The most common etiologies are ulcerative, chron, and pseudomembranous colitis, but other causes exist and can be categorized as:
The diagnosis is made based on clinical evidence of colitis plus evidence of colonic dilation on abdominal XR (diameter > 6cm, loss of haustra, or free intraperitoneal air secondary to perforation) or CT scan (demonstrating dilation or perforation).
Treatment includes:
Autenrieth, D et al. Toxic Megacolon Inflammatory Bowel Dis. 2011 Aug 29.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 10/2/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Thrombotic Thrombocytopenic Purpura (TTP)
Kessler CS, et al. Thrombotic thrombocytopenic purpura: A hematological emergency. J Emerg Med 2012; 43:538-44.
Category: Critical Care
Posted: 9/25/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Intubated patients may occasionally meet certain criteria for extubation while in the Emergency Department. Extubation is not without its risk, however, as up to 30% of patients have respiratory distress secondary to laryngeal and upper airway edema, with some patients requiring re-intubation.
Prior to extubation, Intensivists use a brief “cuff-leak” test (deflation of the endotracheal balloon to assess the presence or absence of an air-leak around the tube) to indirectly screen for the presence of upper airway edema and ultimately the risk of re-intubation. The cuff-leak test is performed by deflating the endotracheal balloon followed by one or more of the following maneuvers:
Ochoa et al. performed a systematic review to determine the accuracy of the “cuff-leak” test to predict upper airway edema prior to extubation. The authors concluded that a positive cuff-leak test (i.e., absence of an air-leak) indicates an elevated risk of upper airway obstruction and re-intubation. A negative cuff-leak test (i.e., presence of an air-leak), however, does not reliably exclude the presence of upper airway edema or the need for subsequent re-intubation.
Bottom line: No test prior to extubation reliably predicts the absence of upper airway edema. Patients extubated in the Emergency Department require close observation with airway equipment located nearby.
Ochoa, ME et al. Cuff-leak test for the diagnosis of upper airway obstruction in adults: A systematic review and meta-analysis. Intensive Care Med (2009) 35:1171–1179
Follow me on Twitter @criticalcarenow or Google+ (+Haney Mallemat)
Category: Critical Care
Posted: 9/18/2012 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
The Lung Transplant Patient in Your ED
Fuehner T, et al. The lung transplant patient in the ICU. Curr Opin Crit Care 2012; 18:472-8.
Category: Critical Care
Posted: 9/11/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
40 year-old male with severe uncontrolled hypertension presents with altered mental status (head CT below). The CXR is from the same patient. What's the connection?
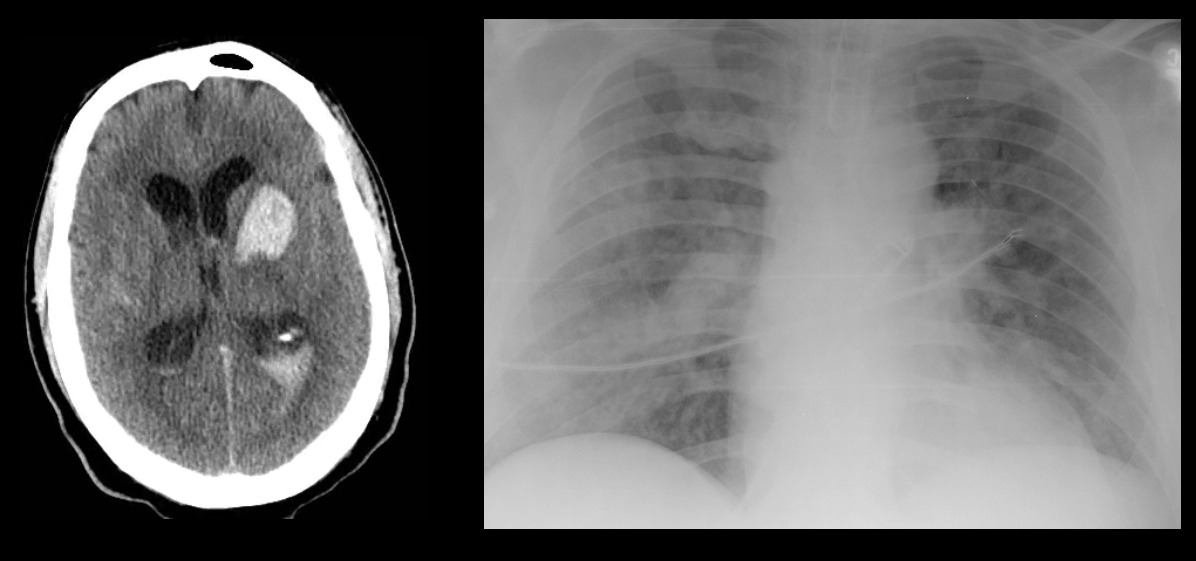
Answer: Neurogenic pulmonary edema (NPE)
NPE is defined as acute pulmonary edema following central nervous system (CNS) insult; NPE has been recognized for over 100 years, but its incidence is underreported due to a lack objective clinical criteria.
The pathophysiology of NPE is poorly understood but it is generally believed that both cardiogenic and non-cardiogenic pulmonary edema play a role. CXR (see above) demonstrates a pattern similar to acute respiratory distress syndrome (i.e., bilateral interstitial infiltrates).
CNS insults that are abrupt, rapidly progressive, and increase intracranial pressure (e.g., subarachnoid hemorrhage, intraparenchymal hemorrhage, traumatic brain injury, subdural, etc.) have the highest risk for NPE. Neural injury leads to sympathetic activation, the release of catecholamines, and one or all of the following:
Treatment of NPE includes:
Davidson, D. et al. Neurogenic pulmonary edema. Crit Care. 2012 Mar 20;16(2):212.
Follow me on Twitter (@criticalcarenow) and Google+ (+haneymallemat)
Category: Critical Care
Posted: 9/4/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Right Heart Failure in the Critically Ill
Greyson CR. Right heart failure in the intensive care unit. Curr Opin Crit Care 2012; 18:424-31.
Category: Critical Care
Posted: 8/28/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A Cochrane review of 37 studies concluded that Succinylcholine (SUC) is superior to Rocuronium (ROC) during rapid sequence intubation.
The authors claim that compared to ROC, SUC has a faster onset of action (45 vs. 60 seconds) and overall a shorter duration of action (10 vs. 60 minutes).
Dr. Reuben Strayer wrote a letter to the journal editors and stated that these findings should be interpreted carefully; he highlighted that most of the studies in the review used doses of ROC less than 0.9 mg/kg (most studies used 0.6mg/kg).
Dr. Strayer asserted that ROC’s onset of action is dose dependent; when using doses of 1.2 mg/kg, ROC’s onset is indistinguishable from that of SUC. He also stated another major benefit of ROC is the lack of adverse effects that SUC possesses (hyperkalemia and malignant hyperthermia).
What are your thoughts on this? Go to http://www.facebook.com/Criticalcarenow and take the poll (there are 5 choices). Results will be posted next week.
Seupaul RA, Jones JH. Evidence-based emergency medicine. Does succinylcholine maximize intubating conditions better than rocuronium for rapid sequence intubation? Ann Emerg Med. 2011 Mar;57(3):301-2. Epub 2010 Nov 18.
Strayer RJ. Rocuronium versus succinylcholine: Cochrane synopsis reconsidered. Ann Emerg Med. 2011 Aug;58(2):217-8.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Critical Care
Posted: 8/21/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
AKI and Fluid Balance
Bellomo R, et al. An observational study fluid balance and patient outcomes in the Randomized Evaluation of Normal vs. Augmented Level of Replacement Therapy trial. Crit Care Med 2012; 40:1753-60.
Category: Critical Care
Posted: 8/14/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Femoral venous access is typically limited to the acute resuscitation of critically-ill patients. Several practice-guidelines recommend avoiding the femoral site, or removal once admitted to the ICU, because of the risk of catheter-related bloodstream infection (CRBI) and deep-vein thrombosis (DVT).
A recent systematic review and meta-analysis (including two randomized-control trials and eight cohort-studies) evaluated the risk of CRBI and DVT for catheters placed in either the internal jugular, subclavian, or femoral-venous sites. No difference in the rate of CRBI or DVT was found between the three sites, although the DVT data was less robust (i.e., contained heterogeneous data).
The authors hypothesized that improvements in sterility during central-line placement (e.g., full-barrier precautions), improved nursing care (e.g., central-line site care), and ultrasound guidance may have led to a reduction in femoral site complications.
Although a prospective randomized-control trial is necessary to confirm these results, this meta-analysis challenges the traditional teaching that femoral central-access should be avoided.
Marik, P. et al. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: A systematic review of the literature and meta-analysis Crit Care Med. 2012 Aug;40(8):2479-85.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Critical Care
Posted: 8/7/2012 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Lung Protective Ventilator Settings Still Underutilized
Needham DM, et al. Lung protective mechanical ventilation and two-year survival in patients with acute lung injury: A prospective cohort study. BMJ 2012;344:e2124.
Category: Critical Care
Posted: 7/31/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Crystalloids (i.e., 0.9% saline and lactated ringers) have been used during resuscitation for more than a century. Their invention, however, was more accidental than intentional.
Crystalloids were first used during the European Cholera epidemic of 1831. Hartog Hamburger later modified this solution in 1896 to the solution we know today as "normal" saline. Hamburger's solution was only intended for in vitro study of RBC lysis and was never intended for clinical use.
Around this time, Sydney Ringer was testing several fluids to use for physiologic studies. Ringer's lab assistant was erroneously substituting tap water for distilled water when preparing these solutions. Ringer later discovered that this tap water contained minerals making the solution "physiologic", isotonic, and safe for human use; Alexis Hartmann later added sodium lactate to create Ringer's Lactate.
Since the invention of crystalloids, many types of resuscitation fluids have been created and studied (i.e., albumins, gelatins, and starches); all have been shown to be more expensive, with no more benefit, and with possibly more harm when compared to crystalloids.
The "perfect" resuscitation fluid still alludes us today, but of all of the solutions marketed crystalloids are arguably the best...despite their accidental history.
Awad, S. et al. The history of 0.9% saline. Clinical Nutrition 2008 Apr;27(2):179-88.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Critical Care
Posted: 7/24/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Steroids and Septic Shock
Sherwin RL, Garcia AJ, Bilkovski R. Do low-dose corticosteroids improve mortality or shock reversal in patients with septic shock? A systematic review and position statement prepared for the American Academy of Emergency Medicine. JEM 2012;43:7-12.
Category: Critical Care
Posted: 7/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Wernicke encephalopathy (WE) is a neurologic disorder secondary to prolonged thiamine deficiency; it is characterized by confusion, ataxia, and ocular abnormalities.
Traditional medical teaching advises against the administration of glucose (or glucose containing fluid) in thiamine deficient patients, without first giving thiamine, as this may precipitate WE.
This teaching is problematic, however, in hypoglycemic patients who require the immediate administration of glucose while simultaneously being suspected of thiamine deficiency (e.g., malnourished alcoholics). Delays in treating hypoglycemia may be more harmful (e.g., seizures, permanent neurologic deficits, etc.) than the risk of WE.
Schabelman et. al performed a literature search to unearth the origins of this teaching. Nineteen papers related to this topic were found consisting of case reports, animal studies, and expert opinion; there were no randomized trials, cohort studies, or case-control studies.
Bottom-line: The available evidence does not support withholding glucose treatment until thiamine can be administered and educators should consider abolishing this dogmatic teaching until better evidence is available.
Schabelman, et al. Glucose before thiamine for Wernicke encephalopathy: a literature review. J Emerg Med. 2012 Apr; 42(4): 488-94
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 7/10/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Anaphylaxis
De Bisschop MB, Bellou A. Anaphylaxis. Curr Opin Crit Care 2012; 18:308-17.
Category: Critical Care
Keywords: hydroxyethyl starch crystalloid, colloid, lactated ringers, normal saline, resuscitation, sepsis, hypotension (PubMed Search)
Posted: 7/3/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Septic patients with hemodynamic instability often require intravenous fluids as part of their resuscitation. Major debate has occurred whether the optimal resuscitation fluids are crystalloids (e.g., normal saline) or colloids (e.g., albumin).
In theory, colloids are more potent intravascular expanders than crystalloids because their oncotic pressure is higher and should increase intravascular volume similarly to larger amounts crystalloid (i.e., colloids require less volume during resuscitation).
Despite these theoretical benefits, the colloid hydroxyethyl starch (HES), has come under scrutiny after prior studies have linked its use with adverse outcomes.
A recent prospective randomized-control trial compared the use of HES to lactated acetate for resuscitating septic patients and found that HES significantly increased both the incidence of renal-replacement therapy and mortality at 90 days (both primary end-points in the study).
Bottom line: There is no convincing data that HES performs superiorly to crystalloid for resuscitation in sepsis and there is increased harm with its use. Furthermore, the increased cost of HES compared to crystalloids does not justify its routine use.
Perner A., et al. Hydroxyethyl Starch 130/0.4 versus Ringer's Acetate in Severe Sepsis. NEJM. 2012 Jun 27.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 6/26/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Acute Kidney Injury and Tumor Lysis Syndrome
McCurdy MT, Shanholtz CB. Oncologic emergencies. Crit Care Med 2012; 40:2212-2222.
Category: Critical Care
Posted: 6/19/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Two recently presented abstracts at the 2012 Society of Critical Care Medicine conference suggest that the combination of vancomycin and piperacillin-tazobactam may lead to acute kidney injury (AKI) in the critically ill. There may also be evidence to suggest that piperacillin-tazobactam alone increases the risk of AKI.
Both abstracts retrospectively compared patients who received either vancomycin alone or the combination of vancomycin and piperacillin-tazobactam. In both studies, the rates of AKI were significantly lower in patients treated with vancomycin alone as compared to patients receiving both vancomycin and piperacillin-tazobactam.
Bottom line: Although the current evidence does not support a change in our clinical practice, more prospective studies exploring this topic are necessary.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Min, et al. Acute Kidney Injury in Patients Recieving Concomitant Vancomycin and Piperacillin/Tazobactam. Critical Care Medicine. December 2011. 39(12); p 200
Hellwig, et. al. Retrospective Evaluation of the Incidence of Vancomycin and/or Piperacillin-Tazobactam Induced Acute Renal Failure. Critical Care Medicine. December 2011. 39(12); p 79
Category: Critical Care
Posted: 6/13/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Use the Measured Sodium Concentration!
Beck, L. Cleveland Clin J Med 2001;68:673.
Category: Critical Care
Posted: 6/4/2012 by Haney Mallemat, MD
(Updated: 6/5/2012)
Click here to contact Haney Mallemat, MD
Consider rhabdomyolyisis secondary to heat exposure as summertime approaches; have a low threshold to screen patients if they are at risk (e.g., people exercising in high-ambient temperatures).
Symptoms include muscle tenderness, cramping, and swelling with associated weakness. Patients with altered mental status (e.g., heat stroke) should be examined for limb induration, skin discoloration (i.e., ischemia), or compartment syndrome.
Complications:
Treatment
Khan, F. Y. Rhabdomyolysis: a review of the literature. The Netherlands journal of medicine, 67(9), 272 – 283.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Critical Care
Posted: 5/29/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Severe UGIB
Srygley FD, et al. Does this patient have a severe upper gastrointestinal bleed? JAMA 2012;307:1072-9.
