Category: Cardiology
Posted: 9/7/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
PARADIGM Shift in Heart Failure
- Angiotensin-converting enzymes inhibitors (ACE-I) are cornerstone for treatment of heart failure (HF) given the multiple trials which have shown their positive risk reduction in cardiovascular death.
- Studies looking at the effect of angiotensin-receptor blockers (ARBs) on mortality have been inconsistent; thus ARB's have been recommended as 2nd-line for those who have unacceptable side effects to ACE-I.
- A recent double-blinded RCT (PARADIGM-HF) ~8400 patients with class II-IV HF w/ ejection fraction <40% were treated with enalapril (standard therapy) versus novel therapy with neprilysin (neutral endopeptidase) inhibitor combined with an ARB.
- Primary outcomes were death from cardiovascular causes and hospitalization for HF; The RCT was ceased early (~27 months) because of an overwhelming benefit with the new agent.
- At study closure death occurred 26.5% in the standard group versus 21.8% in the novel group. The risk of HF hospitalization was decreased 21% with novel therapy.
- In early studies the use of a neprilysin inhibitor combined with an ARB has shown superior effects to current standard therapy (ACE-I), however long-term effects of this novel therapy are yet to be determined.
McMurray J, Packer M, Desai A, et al. Angiotension-Neprilysin Inhibition versus Enalapril in Heart Failure. NEJM August 30, 2014.
Category: Cardiology
Keywords: Sick Sinus Syndrome (PubMed Search)
Posted: 8/31/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Sick Sinus Syndrome
- Sick sinus syndrome (SSS) is a cardiac conduction disorder characterized by symptomatic dysfunction of the sinoatrial (SA) node.
- SSS usually manifests as sinus bradycardia, sinus arrest, or sinoatrial block, and is sometimes accompanied by supraventricular tachydysrhythmias.
- Symptoms of SSS include: syncope, dizziness, palpitations, exertional dyspnea, fatigability from chronotropic incompetence, heart failure, and angina.
- Clinically significant SSS typically requires pacemaker implantation. Approximately 30% to 50% of pacemaker implantation in the United States list SSS as the primary indication.
- 2 large, prospective cohorts with an average follow-up of 17 years, observed the incidence of SSS increases with age, does not differ between men and women, and is lower among blacks than whites.
- Risk factors for SSS included greater BMI & height, elevated NT-proBNP level & cystatin C level, longer QRS interval, lower heart rate, hypertension, and right bundle branch block.
Jensen P, Gronroos N, et al. Incidence of and Risk Factors for Sick Sinus Syndrome in the General Population. Journal of the American College of Cardiology. Vol 64 Issue 6, pages 531-538
Category: Cardiology
Keywords: GRACE score (PubMed Search)
Posted: 8/24/2014 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
GRACE Score
- The Global Registry of Acute Coronary Events (GRACE) is an international database tracking outcomes of patients presenting with acute coronary syndromes (ACS).
- GRACE score is calculated based on 8 variables: Age, HR, systolic BP, creatinine, killip class, ST-segment deviation on EKG, cardiac biomarkers, and cardiac arrest on admission.
- Several reports have shown that the GRACE score is a better predictor of clinical outcome (risk of death or the combined risk of death or myocardial infarction at 6 months) than the TIMI score.
- A recent study evaluated the relationship between GRACE score & severity of coronary artery disease (CAD) angiographically evaluated by Gensini score in patients with NSTE-MI.
- Results showed that the GRACE score has significant relation with the extent & severity of CAD as assessed by angiographic Gensini score.
- GRACE score was shown to be important both for determining the severity of the CAD and predicting death within 6 months of hospital discharge from NSTE-MI.
Cakar M, Sahinkus S, et al. Relation between the GRACE score and severity of atherosclerosis in acute coronary syndrome. Journal of Cardiology. 2014 Vol 63, Issue 1, Pgs 24-28.
Category: Cardiology
Keywords: Nonatherosclerotic Coronary Artery Disease (PubMed Search)
Posted: 8/17/2014 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
Nonatherosclerotic Coronary Artery Disease
- Nonatherosclerotic coronary artery disease (NACAD) is a term used to describe a category of diseases, which include: spontaneous coronary artery dissection (SCAD), coronary fibromuscular dysplasia (FMD), ectasia, vasculitis, embolism, vasospasm, or congenital anomaly.
- NACAD is an important cause of myocardial infarction (MI) in young women, but is often missed on coronary angiography.
- A small retrospective study of women <50 years of age with ACS found that 54.8% had normal arteries, 30.5% atherosclerotic heart disease (ACAD), 13% nonatherosclerotic coronary artery disease (NACAD), and 1.7% unclear etiology.
- NACAD accounted for 30% of MI’s with SCAD & Takotsubo cardiomyopathy accounting for the majority of cases.
Saw J, Aymong E, et al. Nonatherosclerotic Coronary Artery Disease in Young Women. Canadian Journal of Cardiology. 2014/07 Vol 30:Issue 7, pgs 814-819.
Category: Cardiology
Posted: 8/10/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
- Toxic effects of tricyclic antidepressants (TCA) are result of the following 4 pharmacologic properties:
1. Inhibition of norepinephrine & serotonin reuptake --> resultant seizure
2. Anticholinergic activity --> resultant altered mental status, tachycardia, mydriasis, ileus
3. Direct alpha-adrenergic blockade --> resultant hypotension
4. Cardiac myocyte sodium channel blockade --> resultant widened QRS
- A QRS interval greater than 100 milliseconds has ~30% chance of developing seizures and ~15% chance of developing a life-threatening cardiac arrhythmia.
- A QRS interval greater than 160 milliseconds increases the chance of ventricular arrhythmias to greater than 50%.
- Clinical pearl: A very wide complex ventricular rhythm, concomitant hypotension and/or seizure disorder is suspicious for toxic ingestion and standard ACLS algorithm will not suffice, treatment must address the underlying culprit (i.e. TCA --> Tx. fluids, vasopressors, sodium bicarbonate, and intravenous lipid emulsion).
Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J. Jul 2001;18(4):236-41.
Category: Cardiology
Keywords: Hypertrophic Cardiomyopathy (PubMed Search)
Posted: 8/3/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Advances in Hypertrophic Cardiomyopathy (HCM)
- HCM is a genetically transmitted autosomal dominant disorder with two variants: hypertrophic obstructive cardiomyopathy (HOCM), also known as idiopathic hypertrophic subaortic stenosis (IHSS) or asymmetric septal hypertrophy, and non-obstructive hypertrophic cardiomyopathy (HNCM), also known as Yamaguchi syndrome.
- The most serious complication of both variants of HCM is sudden cardiac death (SCD) and end-stage heart failure, which rapidly progresses to cardiac death after its occurrence.
- Beta-blockers (1st line) and non-dihydropyridine calcium channel blockers are effective at improving clinical symptoms (syncope, dyspnea, chest pain, and exertional intolerance, etc.) however neither alone nor combined halt the progressive LV remodeling and prevent end-stage heart failure.
- Cardiac transplantation is the only treatment available for end-stage heart failure, but must occur before the onset of pulmonary hypertension, kidney malfunction, and thromboembolism for success.
- Class Ia anti-arrhythmic, disopyramide has been shown to be effective for symptomatic improvement (NYHA classification), but does not improve overall LV function or hypertrophy.
- A recent study found that another class Ia anti-arrhythmic, cibenzoline has been shown not only to reduce symptoms, but also improved LV diastolic dysfunction and induced a regression of LV hypertrophy. In this study cibenzoline has halted the progression of HCM to end-stage heart failure.
Hamada M, Ikeda S, et al. Advances in medical treatment of hypertrophic cardiomyopathy. Journal of Cardiology. July 2014 (64):1;1-10.
Category: Cardiology
Posted: 7/27/2014 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
HIV & Atherosclerosis
Advances in antiretroviral treatment has increased the life expectancy of patients with HIV significantly, AIDS-related deaths have fallen by 30% since they peaked in 2005.
HIV infection predisposes to a chronic inflammatory and immunologic dysfunctional state, subsequent highly active antiretroviral treatment (HAART) results in metabolic changes and dyslipidemia.
In the post-HAART era, CAD is now considered to be the main cause of heart failure in HIV-infected patients, superseding the prior most common etiologies myocarditis and opportunistic infections.
The presentation of CAD in HIV-infected patients is largely similar to that in the general population with the exception is that they present at a younger age.
Certain antiretroviral agents specifically protease inhibitors have conventionally been associated with lipid dysfunction, further complicating the HIV-infected patients milieu.
Recent research has shown that a C-C chemokine receptor-type 5 (CCR5) antagonists has emerged as a potential target both as an antiretroviral agent as well as in the process of arresting atherogenesis, but warrants more research.
Ng B, MacPherson P, et al. Heart failure in HIV infection: focus on the role of atherosclerosis. Current Opinion in Cardiology. Issue: Volume 29(2) pgs. 174-179 March 2014.
Category: Cardiology
Keywords: ARVD (PubMed Search)
Posted: 7/20/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
ECG Risk Predication in ARVD
Arrhythmogenic right ventricular dysplasia (ARVD) is a genetically determined cardiomyopathy characterized by fibrofatty replacement of the right ventricle (RV) predisposing to ventricular arrhythmias, heart failure, and sudden cardiac death (SCD).
Twelve-lead electrocardiography (ECG) is an easily obtainable and noninvasive risk stratification tool for major adverse cardiac event (MACE); defined as a composite of cardiac death, heart transplantation, survived sudden cardiac death, ventricular fibrillation, sustained ventricular tachycardia, or arrhythmic syncope.
ARVD ECG findings that predict adverse outcome are not well known.
A multicenter, observational, long-term study, found ECG findings were quite useful for risk stratification of MACE, specifically:
- Repolarization criteria
- Inferior leads T wave inversions
- Precordial QRS amplitude ratio of ≤0.48
- QRS fragmentation
Saguner A, Ganahi S, et al. Usefulness of Electrocardiographic Parameters for Risk Prediction in Arrhythmogenic right ventricular dysplasia. American Journal of Cardiology. May 15, 2014. Vol 113, Issue 10,1728-34.
Category: Cardiology
Keywords: Ventricular Arrhythmias, Myocardial Infarction (PubMed Search)
Posted: 7/13/2014 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
Ventricular Arrhythmias Associated with Myocardial Infarction
Therapeutic advances and management of acute myocardial infarction (AMI) has lead to a decreasing incidence of ventricular arrhythmias (VA)
VA remains a life-threatening occurrence after AMI, and all patients should be monitored closely during this vulnerable period
VA occurs more frequently inpatients with STEMI versus non-STEMI
Of those who develop VA’s, features associated with poor outcomes include:
· Late occurrence
· Sustained monomorphic VT
· Concurrent heart failure
· Cardiogenic shock
· Failure or lack of revascularization
Liang J, Prasad A, et al. Temporal Evolution and Implications of Ventricular Arrhythmias Associated With Acute Myocardial Infarction. Cardiology in Review: 21 (6) Nov/Dec 2013.
Category: Cardiology
Keywords: Magnesium, cardiovascular disease, arrhythmia (PubMed Search)
Posted: 7/6/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Role of Magnesium in Cardiovascular Disease
* Magnesium (Mg2+) is an essential element that is obtained via dietary intake of leafy green vegetables, legumes, nuts/seeds, and whole grains; it is relatively deficient in the American diet.
* Mg2+ is critical for the normal physiological functioning of the vascular smooth muscle, endothelial cells, and myocardium. Several epidemiological and clinical studies have linked Mg2+ in the pathogenesis of cardiovascular disorders (CVD).
* Mg2+ is well known for its antiarrhythmic properties via modulation of myocardial excitability and in the pathogenesis and treatment of cardiac arrhythmias (polymorphic ventricular tachycardia/torsades de pointes & digoxin toxicity).
* Mg2+ supplementation has also been shown to cause significant decrease in ventricular ectopic beats and nonsustained ventricular tachycardia in NYHA class II–IV heart failure patients.
* A recent meta-analysis by Qu et al examined the association between dietary Mg2+ intake, serum Mg2+ levels, and the risk of total CVD events; the greatest reduction in CVD events was observed for intake between 150-400 mg/d.
* Given the magnitude of CVD and Mg2+-deficient diet in the US, there is a critical need to further investigate the interrelationship between Mg2+ and CVD events. Additionally increasing Mg2+ intake in the diet to maintain high normal serum Mg2+ level is both physiologic and judicious.
Dhaval K, Krishnaswami V, et al. Role of Magnesium in Cardiovascular Diseases. Cardiology in Review. Vol22 (4) pgs. 153-192 July/August 2014
Category: Cardiology
Keywords: IVUS, CAD, vulnerable plaques (PubMed Search)
Posted: 6/29/2014 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
IVUS Plaque Correlation to Cardiovascular Death
Several non-invasive studies are currently utilized for the identification of coronary artery disease (i.e. coronary CTA, intravascular ultrasound- IVUS, etc.)
Few studies have quantified which of those with CAD (i.e. coronary plaques) are considered high-risk or unstable plaques
A recent study utilizing IVUS looked at autopsies over a 2 year-period comparing near-infrared detection of high-risk plaques and cardiovascular related deaths
IVUS findings associated with CAD are classified into 3 categories: echo-attenuation, echolucent zone, and spotty calcification
Echo-attenuated plaques, especially superficial echo-attenuation, was found to be a significant and reliable finding suggestive of vulnerable plaques and future cardiovascular death
Pu J, Mintz G, et al. Insights into echo-attenuated plaques, echolucent plaques, and plaques with spotty calcification. JACC Vol 63, No 2, 2014.
Category: Cardiology
Keywords: Brain-heart syndrome, Neurogenic Stress Cardiomyopathy (PubMed Search)
Posted: 4/27/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
Category: Cardiology
Posted: 4/21/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Subcutaneous Defibrillator
- The implantable cardioverter-defibrillator (ICD) has evolved from devices through epicardial patch electrodes introduced by thoracotomy to transvenous leads advanced to the right ventricle
- Transvenous ICD (T-ICD) reduced the morbidity associated w/thoracotomy implants, however involves potential complications including: hemopericardium, hemothorax, pneumothorax, lead dislodgement, lead malfunction, device-related infection, and venous occlusion
- Subcutaneous ICD (S-ICD) offers the advantage of eliminating the need for intravenous & intracardiac leads. Clinical trials have proven its effectiveness in detecting and treating ventricular fibrillation/tachycardia; however its major disadvantage is its inability to provide bradycardia rate support and anti-tachycardia pacing to terminate ventricular tachycardia
- No study has directly compared the T-ICD & the S-ICD, however clinical data suggests that its use be considered in relatively younger patients (i.e., age <40 years), those at increased risk for bacteremia, patients with indwelling intravascular hardware at risk for endovascular infection, or in patients with compromised venous access
Aziz S, Leon A, et al. The Subcutaneous Defibrillator. JACC Vol 63, Issue 15, Pages 1473-1479
Category: Cardiology
Keywords: Out of hospital cardiac arrest, OHCA, Prehospital airway management (PubMed Search)
Posted: 4/13/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
Optimal out of hospital cardiac arrest (OHCA) airway management strategies remain unclear. In the US, 80% of OHCA patients receive prehospital airway management, most commonly endotracheal intubation (ETI). There is growing enthusiasm for use of supra-glottic airways (SGA) by EMS because of ease of insertion, and the thought that use of SGA reduces interruptions in chest compressions. More recently, studies have suggested improved survival without the insertion of any advanced airway device at all.
A recent secondary analysis of OHCA outcomes in the Cardiac Arrest Registry to Enhance Survival (CARES) compared patients receiving endotracheal intubation (ETI) versus supra-glottic airway (SGA), and also patients receiving [ETI or SGA] with those receiving no advanced airway.
Of 10,691 OHCA, 5591 received ETI, 3110 SGA, and 1929 had no advanced airway. Unadjusted neurologically-intact survival was: ETI 5.4%, SGA 5.2%, no advanced airway 18.6%. Compared with SGA, ETI achieved higher sustained ROSC, survival to hospital admission, hospital survival, and hospital discharge with good neurologic outcome. Moreover, compared with [ETI or SGA], patients who received no advanced airway attained higher survival to hospital admission, hospital survival, and hospital discharge with good neurologic outcome.
Conclusion: In CARES, patients receiving no advanced airway exhibited superior outcomes than those receiving ETI or SGA. When an advanced airway was used, ETI was associated with improved outcomes compared to SGA.
McMullan J, Gerecht R, Bonomo J, et al. Airway management and out-of-hospital cardiac arrest outcome in the CARES registry. Resuscitation. 2014;85(5):617–622. doi:10.1016/j.resuscitation.2014.02.007.
Category: Cardiology
Posted: 3/31/2014 by Semhar Tewelde, MD
(Updated: 4/6/2014)
Click here to contact Semhar Tewelde, MD
Perinatally Infected HIV & Cardiovascular Disease
*Perinatally HIV-infected adolescents are susceptible to aggregate atherosclerotic cardiovascular disease risk, but few studies have quantified risk or developed a scoring system
*A recent study of perinatally HIV-infected adolescents calculated coronary artery and abdominal aorta PDAY (Pathobiological Determinants of Atherosclerosis in Youth) scores using modifiable risk factors: HTN, HLD, smoking, obesity and hyperglycemia
*Significant predictors of a high coronary arteries and abdominal aorta scores include: male sex, Hx AIDS-defining condition, long duration of ritonavir-boosted protease inhibitor, and no prior use of tenofovir
*PDAY scores may be useful in identifying high-risk youth who may benefit from early lifestyle or clinical interventions given their trend of increased aggregate atherosclerotic cardiovascular disease risk factor burden
Patel K, Et al. Aggregate Risk of Cardiovascular Disease Among Adolescents in Perinatally Infected with the Human Immunodeficiency Virus. Circulation Vol 129(11) 18 March 2014, p1204-1212.
Category: Cardiology
Keywords: Cardiac arrest, LVAD, CPR, Chest compressions (PubMed Search)
Posted: 3/23/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
The number of patients with left ventricular assist devices (LVADs) is increasing and development of optimal resuscitative strategies is becoming increasingly important. Despite a lack of evidence, many device manufacturers and hospitals have recommended against performing chest compressions because of fear of cannula dislodgment or damage to the outflow conduit.
A recent retrospective analysis of outcomes in LVAD patients who received chest compressions for cardiac arrest did not support the theory that LVADs would be harmed by conventional resuscitation algorithms.
The study was a limited case series of only 8 LVAD patients over a 4 year period. All patients received compressions and device integrity was subsequently assessed by blood flow data from the LVAD control monitor or by examination on autopsy. Although more research is necessary to determine the utility and effectiveness of compressions in this population, none of the patients in this study had cannula dislodgment and half of the patients had return of neurologic function.
Shinar Z, Bellezzo J, Stahovich M, et al. Chest compressions may be safe in arresting patients with left ventricular assist devices (LVADs). Resuscitation. 2014. doi:10.1016/j.resuscitation.2014.01.003.
Category: Cardiology
Posted: 3/16/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
The HEART Score
Acute coronary syndrome defines a spectrum of diseases (unstable angina, NSTEMI, STEMI), without clear ECG abnormalities the diagnosis and disposition can be challenging
Several scoring systems have attempted to risk stratify patients: TIMI, PURSUIT, and GRACE
The TIMI & PURSUIT scores were designed to identify higher-risk patients and long-term mortality
A pilot/observational study has utilized a novel scoring system to risk stratify low to intermediate risk patients
The HEART (History, ECG, Age, Risk factors and Troponin) score:
This scoring system is limited given the small study size and requires further study/validation, but may be an easy, quick, and reliable predictor of outcome in chest pain patients
Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. Jun 2008; 16(6): 191–196.
Category: Cardiology
Keywords: Echo, Aortic Dissection (PubMed Search)
Posted: 3/9/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
Early diagnosis and surgical consultation for dissection of the ascending aorta can be life saving. Emergency physicians are increasingly using focused cardiac ultrasound to assess chest pain patients in the ED.
The suprasternal notch view (SSNV), may provide additional information in the assessment of thoracic aortic pathology. A recently performed pilot study aimed to determine the accuracy of using the SSNV, in addition to the more traditional parasternal long axis view in assessing aortic dimensions as well as pathology compared to CTA of the chest.
Using a maximal normal thoracic aortic diameter of 40 mm, diagnostic accuracy in detecting dilation of the aorta was 100%. The study showed that the SSNV is feasible and demonstrates high agreement with measurements made on CTA of the chest.
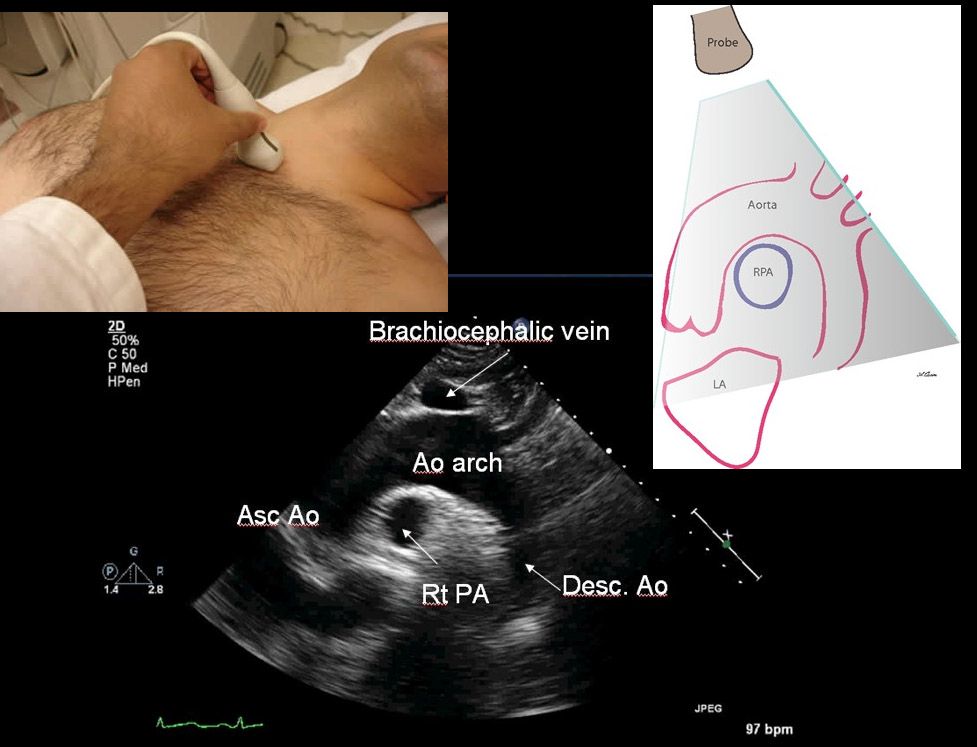
Kinnaman KA, Rempell JS, Kimberly HH, et al. Accuracy of Suprasternal Notch View Using Focused Cardiac Ultrasound to Evaluate Aortic Arch Measurements. YMEM. 2013;62(S):S81. doi:10.1016/j.annemergmed.2013.07.042. Image: http://echocardiographer.org/TTE.html
Category: Cardiology
Keywords: PEA (PubMed Search)
Posted: 2/27/2014 by Semhar Tewelde, MD
(Updated: 3/2/2014)
Click here to contact Semhar Tewelde, MD
Pulseless Electrical Activity (PEA)
ACLS algorithm for PEA focuses on memorizing the “ H's & T's" without a systematic approach on how to evaluate & treat the possible etiologies
A modified approach to PEA focuses on “cause-specific” interventions utilizing two simple tools: ECG and Bedside Ultrasound (US)
Simplified PEA Algorithm
♦1st obtain the ECG and assess the QRS-complex length (narrow vs. wide)
♦ A narrow QRS-complex suggests a mechanical problem: RV inflow or outflow obstruction
Utilize bedside US to assess for RV collapsibility vs. dilation
A collapsed RV suggests tamponade, tension PTX or mechanical hyperinflation
A dilated RV suggests PE
The above listed etiologies all have a preserved/hyperdynamic LV Tx begins w/aggressive IVF’s followed by “cause-specific” therapy: pericardiocentesis, needle decompression, forced expiration/vent management, and thrombolysis respectively
♦ A wide QRS-complex suggests a metabolic (hyperK/acidosis/toxins), ischemic, or LV problem
Utilize bedside US to assess for LV hypokinesis/akinesis
For metabolic/toxic etiologies treat w/calcium chloride and sodium bicarbonate +/- vasopressors
For ischemia and LV failure treat w/cardiac cath. vs. thrombolysis +/- vasopressors/inotropes
♦Trauma and several other etiologies of PEA that are seldom forgotten in any critically ill patient (hypothermia, hypoxia, and hypoglycemia) are not included in this algorithm.
Littmann L, Bustin D, Haley M. A Simplified and Structured Teaching Tool for the Evaluation and Management of Pulseless Electrical Activity. Med Princ Pract 2014; 23:1-6
Category: Cardiology
Keywords: ACS, Stress Test (PubMed Search)
Posted: 2/23/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
1. Banerjee A, Newman DR, Van den Bruel A, Heneghan C. Diagnostic accuracy of exercise stress testing for coronary artery disease: a systematic review and meta-analysis of prospective studies. International Journal of Clinical Practice. 2012;66(5):477–492.
2. Walker J, Galuska M, Vega D. Coronary disease in emergency department chest pain patients with recent negative stress testing. West J Emerg Med. 2010;11(4):384–388.
3. Nerenberg RH, Shofer FS, Robey JL, Brown AM, Hollander JE. Impact of a negative prior stress test on emergency physician disposition decision in ED patients with chest pain syndromes. The American journal of emergency medicine. 2007;25(1):39–44.
