Category: Critical Care
Keywords: Insulin infusion, diabetes mellitus, diabetic ketoacidosis, DKA, subcutaneous, long-acting (PubMed Search)
Posted: 6/29/2022 by Kami Windsor, MD
(Updated: 9/21/2022)
Click here to contact Kami Windsor, MD
Background: It is classically taught that the tenets of DKA management are IV fluids, electrolyte repletion, and an insulin infusion that is titrated until approximately 2 hours after anion gap closure, when long-acting subcutaneous insulin is administered if the patient is tolerating oral intake. It has been previously found that earlier administration of subcutaneous long-acting insulin can shorten the time to anion gap closure, while other small studies have noted similar efficacy in subcutaneous insulin compared to IV in mild/moderate DKA.
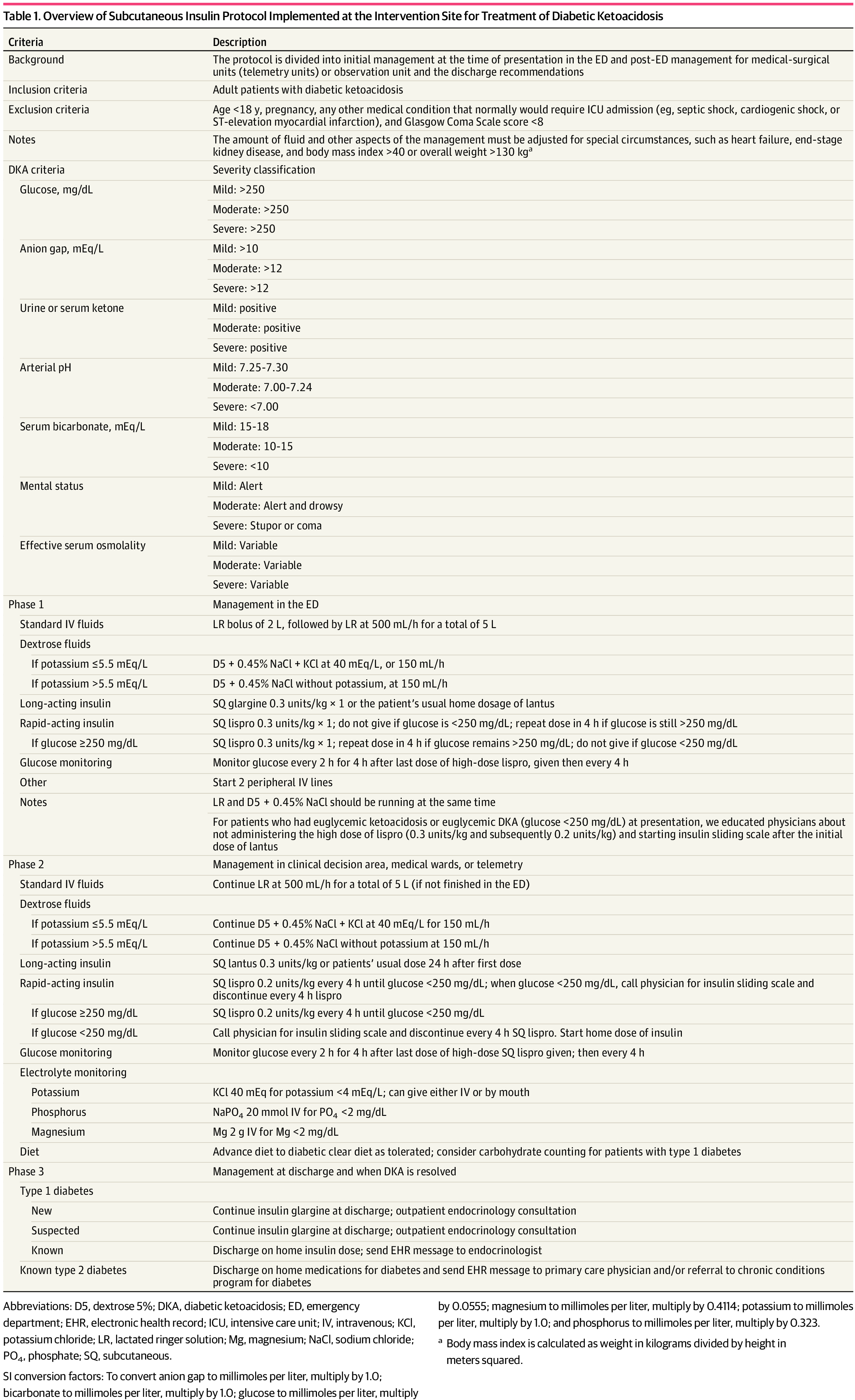
A recent JAMA article presents a retrospective evaluation of a prospectively-implemented DKA protocol (see "Full In-Depth" section) utilizing weight-based subcutaneous glargine and lispro, rather than IV regular insulin, as part of initial and ongoing floor-level inpatient treatment.
When compared to the period before the DKA protocol:
The only exclusion criteria were age <18 years, pregnancy, and presence of other condition that required ICU admission.
Bottom Line: Not all DKA requires IV insulin infusion.
At the very least, we should probably be utilizing early appropriate-dose subcutaneous long-acting insulin. With ongoing ICU bed shortages and the importance of decreasing unnecessary resource use and hospital costs, perhaps we should also be incorporating subcutaneous insulin protocols in our hospitals as well.
As a part of the DKA protocol, patients:
Elevated BMI was not included in exclusion criteria, however the authors note that their DKA protocol has been amended to exclude patients >166kg due to concerns regarding insulin absorption.
Rao P, Jiang S, Kipnis P, et al. Evaluation of Outcomes Following Hospital-Wide Implementation of a Subcutaneous Insulin Protocol for Diabetic Ketoacidosis. JAMA Netw Open. 2022;5(4):e226417. doi:10.1001/jamanetworkopen.2022.6417
Houshyar J, Bahrami A, Aliasgarzadeh A. Effectiveness of Insulin Glargine on Recovery of Patients with Diabetic Ketoacidosis: A Randomized Controlled Trial. J Clin Diagn Res. 2015 May;9(5):OC01-5. doi: 10.7860/JCDR/2015/12005.5883.
Mohamed A, Ploetz J, Hamarshi MS. Evaluation of Early Administration of Insulin Glargine in the Acute Management of Diabetic Ketoacidosis. Curr Diabetes Rev. 2021;17(8):e030221191986. doi: 10.2174/1573399817666210303095633.
Karoli R, Fatima J, Salman T, Sandhu S, Shankar R. Managing diabetic ketoacidosis in non-intensive care unit setting: Role of insulin analogs. Indian J Pharmacol. 2011 Jul;43(4):398-401. doi: 10.4103/0253-7613.83109.
Ersöz HO, Ukinc K, Köse M, Erem C, Gunduz A, Hacihasanoglu AB, Karti SS. Subcutaneous lispro and intravenous regular insulin treatments are equally effective and safe for the treatment of mild and moderate diabetic ketoacidosis in adult patients. Int J Clin Pract. 2006 Apr;60(4):429-33. doi: 10.1111/j.1368-5031.2006.00786.x.
